Introduction
Pressure ulcers are caused by long-term compression
of parts of the body, blood circulation disorder, sustained
ischemia, hypoxia of local tissue and nutritional deficiencies.
This leads to the loss of normal function of skin and causes tissue
damage and necrosis (1). The
pressure leads to poor circulation and eventually contributes to
cell death, skin breakdown and the development of an open wound. If
not adequately treated, open ulcers become a source of pain,
disability and infection. The prevalence of pressure ulcers in
nursing home residents ranges from 8 to 24% and the annual
incidence approaches 12% (2–4).
Methods to prevent and control pressure ulcers are the main focus
of clinical nursing (5). The
standard options for treating pressure ulcers include surgical,
mechanical, autolytic and enzymatic debridement (6). In China, therapies collectively
called traditional Chinese medicine (TCM) are commonly used. This
includes cured rot and flat sore ointment (CHMO), acupuncture and
moxibustion (7). TCM has been used
for the prevention and treatment of ulcers for many years. A
variety of methods have been used for pressure ulcer treatment,
although they have different prescription formulations, the role of
the main approach is to improve local blood circulation and enhance
tissue regeneration (8).
The doctors at The General Hospital of Jinan
Military Area Command (Jinan, China) use a variety of drugs for the
treatment of pressure ulcers, including Arnebia root oil
(ARO), Jing Wan Hong ointment and YuHong ointment. However, none of
these effectively alleviate the pain of patients lying in bed and
they have a slow curative effect and long healing time. With years
of clinical experience of the treatment of pressure ulcers and TCM
research, we developed a TCM ointment called cured rot and flat
sore ointment (CRFSO), composed of gypsum fibrosum (18 g) and three
herbal medicines: hydrargyrum oxydatum crudum (9 g); red orpiment
(6 g) and borneol (0.9 g). Following clinical use, the effect of
CRFSO in the treatment of pressure sores was observed to be
superior to that of other drugs. For verification, a randomized,
controlled and retrospective clinical study was conducted to
evaluate the efficacy and safety of CRFSO. A total of 35
consecutive patients with pressure sores following paraplegia
received CRFSO or ARO treatment from January 2004 to September
2010. The results of our study demonstrate that compared with ARO,
our novel Chinese herbal formula relieved pressure ulcers in
paraplegic patients with a shorter healing time and clear curative
effect.
Materials and methods
Materials
ARO was purchased from Xi’an Realherb Biotech Co.,
Ltd. (Xi’an, China) and CRFSO was prepared by The General Hospital
of Jinan Military Area Command.
Patients
This observational study was conducted from January
2004 to September 2010. The pressure ulcers were classified into
four stages (I, II, III and IV) according the guidelines of the
National Pressure Ulcer Advisory Panel. The pressure ulcer
treatment information of 35 paraplegic patients (69 ulcers) caused
by spinal cord injury from January 2004 to September 2010 was
reviewed. The data were collected from patient records in The
General Hospital of Jinan Military Area Command. Written consent
for data and image use from all patients was received
preoperatively. The inclusion criterion was at least one pressure
ulcer in stage IV. Patients with ulcers from other causes or a
primary site of pathology other than paraplegia were excluded.
Socio-demographic and clinical data were obtained in a predesigned
format. Socio-demographic information, including age, gender and
primary illness was obtained prior to treatment.
After treatment for 2 weeks, 6 patients sought other
modes of therapy, including surgical methods or CRFSO, due to their
own consideration of poor efficacy; these were all from the ARO
group. The other 29 patients completed the treatment evaluation
successfully. No statistical differences in the two groups of
patients were identified in ratio of gender, mean age and mean area
of pressure ulcer in different stages. The 29 patients in the two
groups had a total of 57 ulcers (31 were stage IV and 26 under
stage IV). Table I shows the
location distribution of these pressure ulcers. ARO was applied to
10 patients with a total of 20 ulcers (11 ulcers at stage IV) and
the other 19 patients with a total of 37 ulcers (20 ulcers at stage
IV) received the novel Chinese herbal formula. The demographic data
(Table II) demonstrated no
significant differences (P>0.05). The study was approved and
registered by The General Hospital of Jinan Military Area Command
in March 2010, the Ethics committee approved the screening,
treatment and data collection of these patients. All subjects
signed the written informed consent form. All work was undertaken
following the provisions of the Declaration of Helsinki.
 | Table ISite of pressure ulcers in paraplegic
patients. |
Table I
Site of pressure ulcers in paraplegic
patients.
| Site of ulcers | No. of patients | No. of ulcers | No. of stage IV
ulcers |
|---|
| Sacrococcygeal
region | 11 | 24 | 16 |
| Hip | 11 | 19 | 8 |
| Ankle | 5 | 10 | 5 |
| Heel | 2 | 4 | 2 |
 | Table IIBaseline characteristics of the
patients (n=29). |
Table II
Baseline characteristics of the
patients (n=29).
| Characteristics | ARO group | CRFSO group | P-value |
|---|
| No. of patients | 10 | 19 | >0.05 |
| No. of male
patients | 6 | 13 | >0.05 |
| Median age
(years) | 58. 6±3.5 | 59.7±4.2 | >0.05 |
| Number of ulcers at
stage IV | 11 | 20 | >0.05 |
| Pressure ulcer area
(cm2) | 14.8±2.6 | 16.1±3.3 | >0.05 |
Procedures
A 0.9% sodium chloride injection was used to clean
wounds (ulcers) and then vesicular, ulcerated and necrotic tissue
was removed. An infrared lamp was used to irradiate the disinfected
pressure ulcers and the surrounding 2–3 cm area for ∼30 min.
Following routine disinfection, the majority of the necrotic flesh
was cut away using repeated hydrogen peroxide and saline cleaning.
Then the ARO or CRFSO was administered to the affected area.
The ARO group was treated with the application of a
gentamicin wet gauze (100 ml 0.9% sodium chloride injection plus
240,000 units gentamicin) on the pressure ulcers and the CRFSO
group received 68 g CRFSO. Aseptic dressing and bandages were used
in the two groups and changed every 1–2 days until the ulcers had
healed. All patients underwent necessary care and pain treatment
during the study.
Evaluation methods
Evaluation was conducted after 28 days of treatment.
The therapeutic effect was divided into the following grades: i)
healing: the ulcer healed, became a scab and was shed; ii)
effective: the ulcer was apparently contractible and the growth of
granulation tissue was good with significant alleviation of pain;
iii) improved: the ulcer area and secretion were reduced and pain
was alleviated; and iv) no response: no changes or the local wound
was infected. The therapeutic duration was recorded as the ulcer
healing time.
Statistical analysis
Therapeutic duration is presented as mean ± SD.
Comparisons of continuous variables between the two groups were
performed by one-way analysis of variance (ANOVA). If the F
distribution was significant, a t-test was used to specify
differences between groups. P<0.05 was considered to indicate a
statistically significant difference. The SPSS 19.0 software
package (SPSS, Inc., Chicago, IL, USA) was used for the statistical
tests.
Results
No patient had any ointment-related serious adverse
reaction during the treatment. Of the 29 patients that received
external application of ointment to treat pressure ulcers, we
observed a higher healing rate (17 of 20 in the CRFSO group and 5
of 11 in the ARO group) and lower no response rate (1 of 20 in the
CRFSO group and 2 of 11 in the ARO group) in patients treated with
CRFSO compared with ARO. Treatment was effective in 2 of 20
patients in the CRFSO group and 3 of 11 in the ARO group. Improved
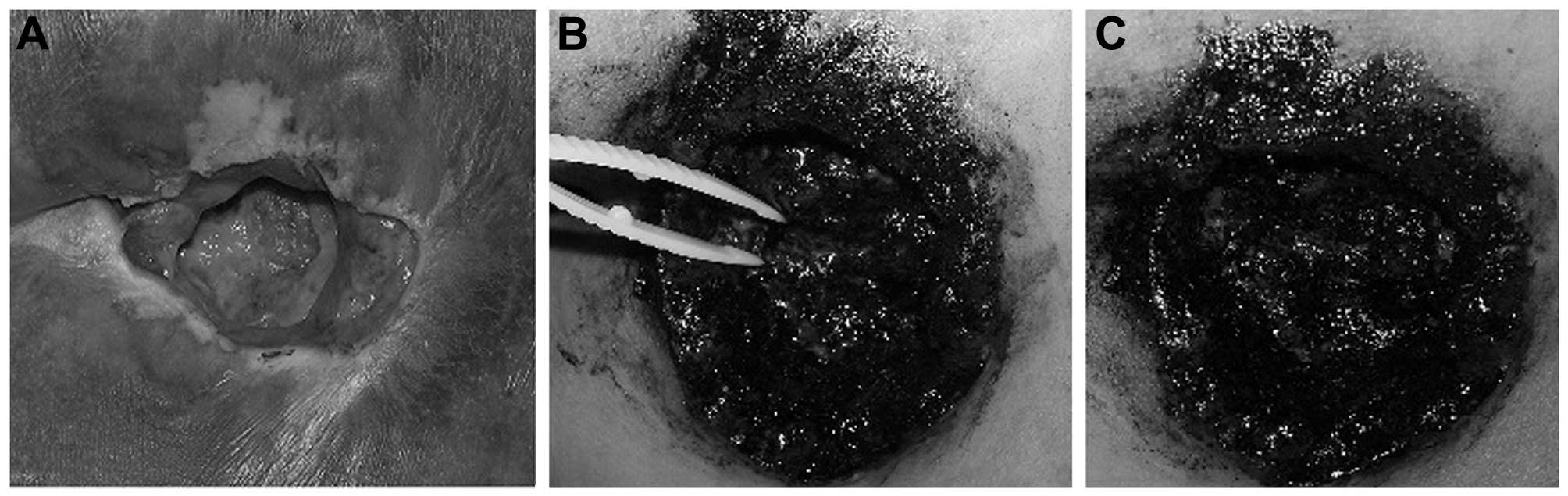
results were observed in 1 of 11 ulcers in the ARO group. Fig. 1 shows the treatment result of one
pressure ulcer (stage IV) with CRFSO. The therapeutic duration of
treatment with ARO ranged from 19 to 43 days (mean, 29.18±3.18
days); a relatively shorter treatment time was recorded for CRFSO,
which ranged from 14 to 36 days (mean, 19.47±4.99 days). The
therapeutic effect and therapeutic duration of the two groups are
summarized in Fig. 2. Statistical
analysis revealed that the therapeutic duration of the two groups
was significantly different (P<0.05).
Compared with ARO, the CRFSO treatment time is
shorter and the patient outcome is improved. This traditional
Chinese herbal formula relieves pressure sores in paraplegic
patients effectively and inpatient rehabilitation is significantly
improved.
Discussion
Pressure ulcer management is divided into
non-surgical and surgical methods. Drug-based inhibition of
pressure ulcers by the use of a single medicine for external
application, has provided a useful and cost-effective procedure
without risk to the patient (9). A
pressure ulcer in paraplegic patients is a unique type of chronic
ulcer with its own characteristics and healing is much more
difficult compared with that of an ordinary wound. Despite
aggressive treatment for pressure ulcers, individualized therapy
must be tailored to each patient according to gender, age,
pathophysiology, expectations and financial situation.
TCM and its extracts are commonly used topically in
the clinic and show unique efficacy, particularly for burns,
diabetic foot ulcers, cervical erosion, herpes zoster, chronic
ulcers (oral and skin) and warts (10–13).
We developed a TCM ointment, (CRFSO), which comprises four
ingredients: gypsum fibrosum, hydrargyrum oxydatum crudum, red
orpiment and borneol. Gypsum fibrosum was used to dilute the
concentration of the active organic ingredient (14) and to treat heat syndrome according
to the ‘Yin-yang’ theory (15).
Hydrargyrum oxydatum crudum is mainly used in the treatment of
furuncles, trauma and anal fistulae (16). Red orpiment (Realgar) is an
important component of traditional Chinese medicine formulation,
which have effects of detoxifying, insecticidal and drying
(17). Borneol is commonly used on
the skin to accelerate the permeability of other pharmaceutical
ingredients (18). Combined with
other traditional Chinese formulae, we identified a formulation
with reasonable proportions. During years of clinical application,
this formula has been shown to be effective.
Compared with Western medicine, the toxicity and
adverse effects of Chinese medicines are fewer and relatively more
common in meridians and collaterals (19). According to of Chinese herbalism
theory, interactions among the herbs may produce synergistic
effects and neutralize the potential toxicity or side-effects of
the individual constituents (20).
A number of clinical studies have demonstrated the efficacy of TCM
in the treatment of pressure ulcers (12,13,20).
In our retrospective evaluation of the efficacy of
CRFSO in the treatment of stage IV pressure ulcers, the average
healing rates in the ARO and CRFSO groups were 45.45% and 85%,
respectively. A shorter therapeutic duration was recorded in CRFSO
group compared with ARO group; average 29.18±3.18 days in the ARO
group and 19.47±4.99 days in the CRFSO group.
The TCM principle of ‘boosting qi, increasing
collateral dredging, activating stagnant blood and dissolving
stasis’ (21–24) was applied in our formula and the
positive outcome of this study demonstrated that the TCM formula
CRFSO is a promising treatment for pressure ulcers.
In recent years, combinations of traditional Chinese
and Western medicine treatment have been used as effective clinical
treatments for a number of diseases (25,26).
With the result of the current retrospective clinical evaluation,
further studies concerning the possibility of combing this novel
Chinese herbal formula with Western medicine to treat pressure
ulcers is required. Additionally, limited by sample size, the
results require further confirmation in a larger randomized,
controlled clinical trial, which is ongoing.
References
|
1.
|
Fogerty M, Guy J, Barbul A, Nanney LB and
Abumrad NN: African Americans show increased risk for pressure
ulcers: a retrospective analysis of acute care hospitals in
America. Wound Repair Regen. 17:678–684. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Baumgarten M, Margolis D, Gruber-Baldini
AL, et al: Pressure ulcers and the transition to long-term care.
Adv Skin Wound Care. 16:299–304. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Davis CM and Caseby NG: Prevalence and
incidence studies of pressure ulcers in two long-term care
facilities in Canada. Ostomy Wound Manage. 47:28–34.
2001.PubMed/NCBI
|
|
4.
|
Bates-Jensen BM: Quality indicators for
prevention and management of pressure ulcers in vulnerable elders.
Ann Intern Med. 135:744–751. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
David J: The size of the problem of
pressure ulcers. 1981 J Tissue Viability. 15:12–14. 2005.
View Article : Google Scholar
|
|
6.
|
Niezgoda JA and Mendez-Eastman S: The
effective management of pressure ulcers. Adv Skin Wound Care.
19(Suppl 1): 3–15. 2006. View Article : Google Scholar
|
|
7.
|
Zhang QH, Sun ZR, Yue JH, et al:
Traditional Chinese medicine for pressure ulcer: a meta-analysis.
Int Wound J. 10:221–231. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Wang YF, Que HF, Xu JN, et al: Assessment
of external methods of traditional Chinese medicine in patients
with chronic ulcer of the lower extremities: study protocol of a
multicenter, randomized, parallel-group, prospective trial. Zhong
Xi Yi Jie He Xue Bao. 10:166–175. 2012.(In Chinese).
|
|
9.
|
Barton A and Barton M: Drug-based
inhibition of pressure ulcers. 1981. J Tissue Viability. 15:10–11.
2005. View Article : Google Scholar
|
|
10.
|
Kopp J, Wang GY, Horch RE, Pallua N and Ge
SD: Ancient traditional Chinese medicine in burn treatment: a
historical review. Burns. 29:473–478. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Tam JC, Lau KM, Liu CL, et al: The in vivo
and in vitro diabetic wound healing effects of a 2-herb formula and
its mechanisms of action. J Ethnopharmacol. 134:831–838. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
No authors listed. Clinical study of huang
wu san on the treatment of cervical erosion. Zhong Xi Yi Jie He Za
Zhi. 5:208–210. 1941985.(In Chinese).
|
|
13.
|
Huang Y, Zhang L, Liu G, Huang W, Jia X
and Naomi M: Clinical observation on therapeutic effect of Ji De
Sheng She Yao tablet on 16 cases with AIDS complicated by herpes
zoster. J Tradit Chin Med. 21:34–36. 2001.PubMed/NCBI
|
|
14.
|
Carretero MI and Pozo M: Clay and non-clay
minerals in the pharmaceutical industry Part I. Excipients and
medical applications. Applied Clay Science. 46:73–80. 2009.
View Article : Google Scholar
|
|
15.
|
MenJiuzhang GL: A General Introduction to
Traditional Chinese Medicine in Fundamental Contents of the Theory
of Five Elements in TCM. 1st edition. CRC Press; NY, USA: pp.
84–86. 2009
|
|
16.
|
Che YM, Wang JB, Liu YH, Zuo YG and Fang
K: Clinical observation on the treatment of 30 cases of condyloma
accuminatum by external using hydrargyrum oxydatum crudum. Guiding
Journal of TCM. 11:23–25. 2007.
|
|
17.
|
Zhong L, Chen F, Han J, Shao N and Ouyang
R: Effects of red orpiment on cell morphology and expression of PML
mRNA and protein in NB4 and HL-60 cells. Chin Med J (Engl).
116:148–150. 2003.
|
|
18.
|
Lü Y, Lu JY, Zhao M, Li ZH and Yang Y:
Effect of change in high mobility group protein box 1 expression on
activity of immunocytes in spleen of mice with multiple organ
dysfunction syndrome. Zhongguo Wei Zhong Bing Ji Jiu Yi Xue.
21:25–28. 2009.(In Chinese).
|
|
19.
|
Han J: Meridian is a three-dimensional
network from bio-electromagnetic radiation interference: an
interference hypothesis of meridian. Cell Biochem Biophys.
62:297–303. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
20.
|
Fan AY, Lao L, Zhang RX, Zhou AN and
Berman BM: Preclinical safety evaluation of the aqueous acetone
extract of Chinese herbal formula Modified Huo Luo Xiao Ling Dan.
Zhong Xi Yi Jie He Xue Bao. 8:438–447. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
21.
|
Hu B, Tian D and He Y: Studies on the
effects of Qi-boosting toxin-resolving decoction on proliferation
of nasopharyngeal carcinoma cell. Lin Chung Er Bi Yan Hou Tou Jing
Wai Ke Za Zhi. 23:558–560. 2009.(In Chinese).
|
|
22.
|
Chen Q, Weidner R, Vossel S, Weiss PH and
Fink GR: Neural mechanisms of attentional reorienting in
three-dimensional space. J Neurosci. 32:13352–13362. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
23.
|
Guo LF, Wang FL and Wang YH: Efficacy
observation of treating early and midterm chronic renal failure
patients by qi supplementing, collateral dredging, detoxifying, and
turbidity descending recipe combined with basic methods of Western
medicine. Zhongguo Zhong Xi Yi Jie He Za Zhi. 32:1042–1045.
2012.(In Chinese).
|
|
24.
|
Lu X and Li B: Exploration of the effect
and mechanism of activating blood circulation and stasis-removing
therapy on tumor metastasis. Chin J Integr Med. 15:395–400. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
25.
|
Wu M, Jiang H and Wei GL: Retrospection
and reflection on the integrated Chinese and Western medicine.
Zhongguo Zhong Xi Yi Jie He Za Zhi. 30:1209–1212. 2010.(In
Chinese).
|
|
26.
|
Zhang AL, Changli Xue C and Fong HHS:
Integration of Herbal Medicine into Evidence-Based Clinical
Practice: Current Status and Issues. Herbal Medicine: Biomolecular
and Clinical Aspects. 2nd edition. Benzie IFF and Wachtel-Galor S:
Boca Raton, FL, USA: 2011, View Article : Google Scholar : PubMed/NCBI
|