Introduction
Chronic rhinosinusitis (CRS) with nasal polyps is a
heterogeneous group of inflammatory diseases of the nasal and
paranasal cavities (1).
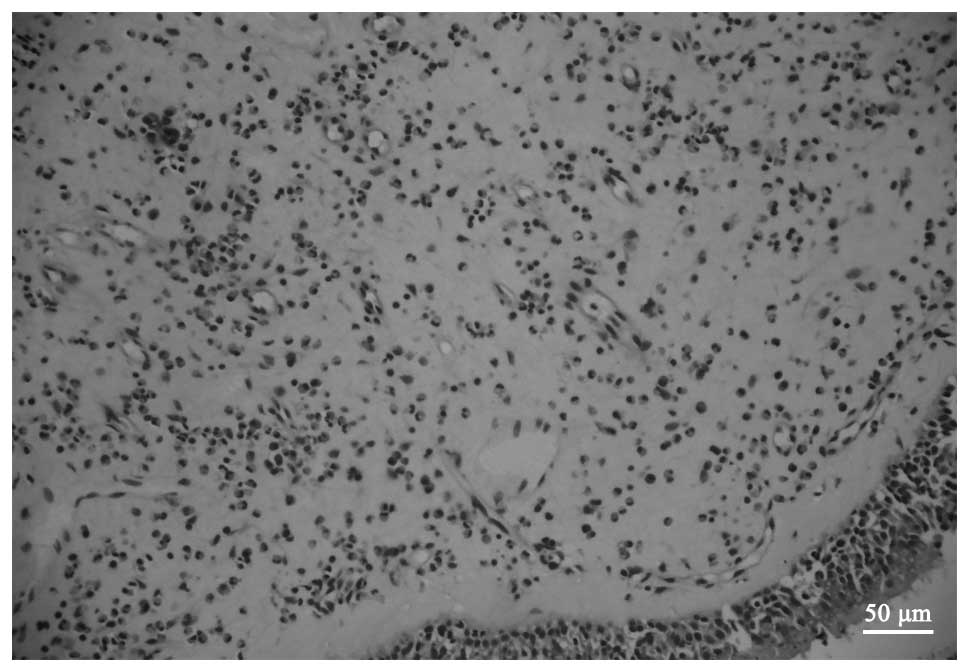
Histologically it manifests as an extremely edematous interstice
covered with respiratory epithelium. Inflammatory cell infiltration
occurs in the interstice, mainly eosinophil infiltration,
accompanied by long tubular gland formation (1,2).
Endoscopic sinus surgery (ESS) is a well-established strategy for
the treatment of CRS, which does not respond to medical treatment.
However, 5–10% of patients fail to respond to conventional ESS
(3). Previous studies have shown
that high-grade mucosal inflammation often results in a poor
outcome (4). Cellular infiltration
and local cytokine activity in the sinus mucosa collected at
surgery may have important prognostic value for long-term outcome
(5–7), Eosinophils, which contribute to
mucosal injury by secretion of toxic granule proteins, including
major basic protein and eosinophil cationic protein, play an
important role in these procedures (8). However, the altered properties of the
mucus in the nasal cavity decrease the function of the mucociliary
clearance system. Goblet cells and subepithelial thickening are the
histopathological parameters which correlate with the largest
number of symptoms of allergic and non-allergic patients with CRS
(9).
The aim of this study was to identify pathological
indicators to predict the efficacy of ESS and to understand the
pathological basis of refractory sinusitis.
Subjects and methods
Subjects
A total of 99 patients with CRS with nasal polyps
underwent ESS by the same doctor at the Department of
Otolaryngology, The First People’s Hospital of Foshan from January
2009 to December 2010. Of these, 53 patients who were able to
return for a second visit and complete a survey questionnaire were
selected, including 27 males and 26 females, ranging in age from 13
to 80 years (average, 36 years). All patients had nasal congestion,
rhinorrhea, hyposmia and/or headaches and other symptoms persisting
for >12 weeks. Anterior rhinoscopy or nasal endoscopy revealed
middle meatus and/or olfactory cleft mucosal swelling, sticky
purulent discharge and translucent neoplasm. Preoperative computed
tomography (CT) revealed that the sinus mucosa had widespread or
localized inflammatory lesions. Postoperative pathological biopsy
indicated chronic inflammation of the mucosa and nasal polyp. This
study was conducted in accordance with the Declaration of Helsinki
and with approval from the Ethics Committee of the First Hospital
of Foshan. Written informed consent was obtained from all
participants.
Symptomatology survey
The Sino-Nasal Outcome Test-20 (SNOT-20) was used as
a reference to design a symptom survey questionnaire and scoring
standard (10), including
congestion, sneezing, rhinorrhea, cough, post-nasal discharge,
thick nasal discharge, ear fullness, dizziness, ear pain, facial
pain/pressure and olfaction. A total of 99 patients hospitalized in
the Department of Otolaryngology, The First People’s Hospital of
Foshan from January 2009 to December 2010 with CRS with nasal
polyps who underwent ESS by the same physician were notified by
telephone. Of the 99 patients, 53 patients returned to the hospital
for follow-up investigation. The same investigator conducted the
questionnaire survey and patients filled out the forms by
themselves or under guidance.
Pathological data survey
The surgical specimen biopsies of 53 patients were
retrospectively analyzed (Fig. 1)
and graded. A semi-quantitative method was used to determine
relevant pathological indicators, including eosinophils,
lymphocytes, goblet cell infiltration density, edema of the
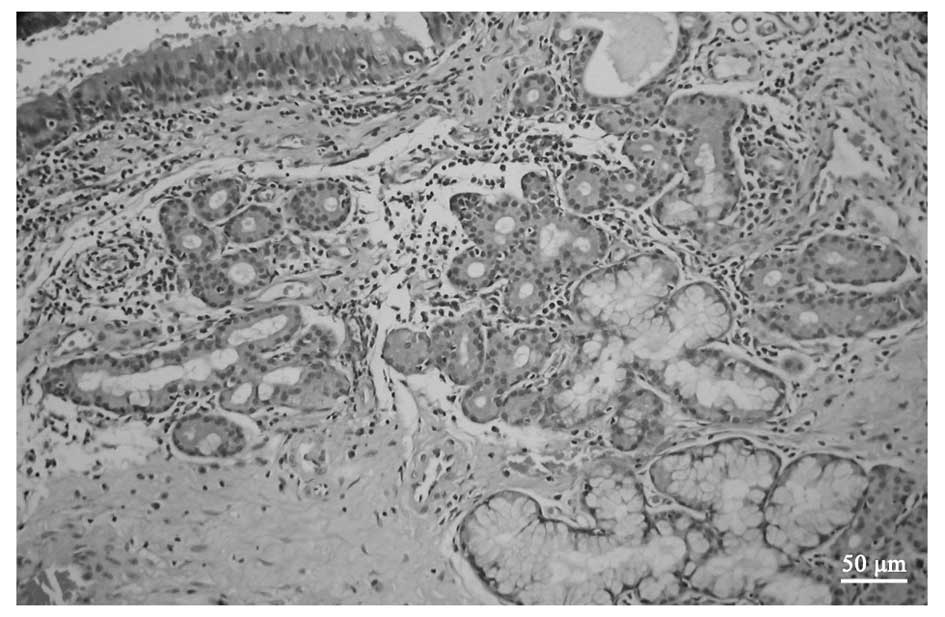
submucosa and pathological mucosal gland density. Pathological
glands refer to glands with lumen expansion, glands with cavities
containing blue-staining mucinous secretions and glands with cystic
dilatation (10,11), as shown in Fig. 2.
Specific grading criteria were as follows (9,12):
i) Goblet cell infiltration density classification (high power
field, magnification, ×400/0.144 mm2): 0, no goblet
cells in the gland; 1, scattered goblet cells; 2, goblet cells
diffusely distributed; and 3, flake-shaped goblet cells. ii)
Lymphocytic infiltration density classification (high power field,
magnification, ×400/0.144 mm2): 10 high power fields
were counted and the average number of lymphocytes was calculated.
The gradings were as follows: 0, 0–20; 1, 21–50; 2, 51–80; and 3,
>80. iii) Eosinophil count (high power field, magnification,
×400/0.144 mm2): 10 high power fields were counted and
the average number of eosinophils was calculated. The gradings were
as follows: 0, 0–3; 1, 4–10; 2, 11–30; and 3, >30. iv) Mucosal
pathological gland density (low magnification, ×100): 0, 0–3; 1,
4–10; 2, 11–30; and 3, >30. v) The degree of submucosal tissue
edema (low magnification, ×100): 0, no edema; 1, mild edema; 2,
moderate edema; and 3, significant edema.
Statistical analysis
Correlation analysis between the main symptoms and
the pathological indicators of patients with ESS was performed
using Spearman’s rank correlation test. P<0.05 was considered to
indicate a statistically significant difference.
Results
Common symptoms following ESS
The five most common symptoms of patients with CRS
with nasal polyps following ESS are nasal congestion, runny
purulent nasal discharge, sneezing, rhinorrhea and postnasal drip,
successively.
Correlation between symptoms and
pathological indicators
The results of the statistical analysis of the
correlation between pathological parameters and symptomatology are
presented in Table I.
 | Table I.P-values for Spearman’s rank
correlation analysis of subjective symptoms and pathological
parameters of patients following endoscopic sinus surgery. |
Table I.
P-values for Spearman’s rank
correlation analysis of subjective symptoms and pathological
parameters of patients following endoscopic sinus surgery.
| Symptoms | Eosinophils
| Lymphocytes
| Goblet cells
| Pathological glands
| Tissue edema
|
|---|
| P-value | Correlation
coefficient | P-value | Correlation
coefficient | P-value | Correlation
coefficient | P-value | Correlation
coefficient | P-value | Correlation
coefficient |
|---|
| Nasal congestion | 0.349 | 0.131 | 0.317 | 0.140 | 0.070 | 0.251 | 0.625 | 0.069 | 0.128 | 0.212 |
| Sneezing | 0.087 | 0.237 | 0.959 | 0.007 | 0.039a | 0.284 | 0.547 | 0.085 | 0.230 | 0.168 |
| Rhinorrhea | 0.499 | 0.095 | 0.602 | 0.073 | 0.815 | 0.033 | 0.476 | 0.100 | 0.542 | 0.086 |
| Coughing | 0.757 | 0.044 | 0.143 | 0.204 | 0.799 | 0.036 | 0.839 | 0.029 | 0.558 | 0.082 |
| Postnasal drip | 0.124 | 0.214 | 0.421 | 0.113 | 0.906 | 0.017 | 0.102 | 0.227 | 0.040a | 0.283 |
| Purulent nasal
discharge | 0.129 | 0.211 | 0.692 | 0.056 | 0.036a | 0.289 | 0.773 | 0.041 | 0.398 | 0.118 |
| Ear fullness | 0.465 | 0.102 | 0.957 | 0.008 | 0.706 | 0.053 | 0.361 | 0.128 | 0.431 | 0.110 |
| Dizziness | 0.344 | 0.133 | 0.360 | 0.128 | 0.227 | 0.169 | 0.008a | 0.359 | 0.088 | 0.237 |
| Ear pain | 0.796 | 0.036 | 0.652 | 0.063 | 0.976 | 0.004 | 0.847 | 0.027 | 0.918 | 0.015 |
| Facial pain | 0.824 | 0.031 | 0.890 | 0.020 | 0.694 | 0.055 | 0.728 | 0.049 | 0.164 | 0.194 |
| Hyposmia | 0.931 | 0.012 | 0.280 | 0.151 | 0.267 | 0.155 | 0.668 | 0.060 | 0.419 | 0.113 |
Correlation between eosinophil
infiltration density and symptoms
There was not determined to be a statistically
significant correlation between eosinophil infiltration density and
any of the symptoms (P>0.05).
Correlation between lymphocyte
infiltration density and symptoms
No statistically significant correlation was
identified between the lymphocyte infiltration density and any of
the symptoms (P>0.05).
Correlation between goblet cell density
and symptoms
There were statistically significant correlations
between goblet cell density and sneezing and purulent nasal
discharge (P=0.039 and P=0.036, respectively) with no correlation
between goblet cell density with other symptoms.
Correlation between the number of
pathological glands and symptoms
The number of pathological glands and dizziness
presented a statistically significant correlation (P=0.008) with no
correlation between pathological glands and other symptoms.
Correlation between degree of tissue
edema and symptoms
The correlation between the degree of tissue edema
and postnasal drip was revealed to be statistically significant
(P=0.040) There was no correlation between degree of tissue edema
and other symptoms.
Discussion
The aim of this study was to identify pathological
features associated with the outcome of ESS and to understand the
pathological basis of refractory sinusitis. The study demonstrated
that the most common nasal symptoms that distress patients
following ESS are nasal congestion, runny purulent nasal discharge,
rhinorrhea, postnasal drip and sneezing. Goblet cells and
pathological glands are signification in the development of certain
symptoms following ESS.
Lanza and Kennedy (13) suggested that since the diagnostic
criteria of sinusitis are based on the local symptoms of the
patient, indicators for determining the success or failure of
chronic nasal-sinusitis surgery should also be based on the
assessment of symptom relief. A number of questionnaires have been
designed to evaluate the quality of life of patients and studies
have shown that the health status of 88% of patients improved
following ESS (14,15). The Medical Outcome Study Short
Form-36 (SF-36) is a universal scale, which provides a good
evaluation of a patient’s overall postoperative health situation.
However, it also contains entries for emotional state and the
correlation analysis for certain pathological conditions of the
sinus mucosa is unrealistic. Therefore in the present study, we
assessed local situations related to nasal symptoms using the
SNOT-20 questionnaire. Since there was no entry concerning sense of
smell among the questions, we added hyposmia to improve the
assessment of nasal symptoms. In our study of 53 patients with CRS
with nasal polyps 1–2 years after ESS, we identified that the most
common nasal symptoms that distress patients following surgery are
nasal congestion, runny purulent nasal discharge, sneezing,
rhinorrhea and postnasal drip.
A previous study demonstrated that asthma or a
history of allergic rhinitis, previous nose surgery and nasal
polyps are adverse prognostic factors of ESS (4). In addition, CT grading of sinus
disease, nasal partial cell infiltration and infiltration of
cytokines, including an increase in eosinophils and interleukin
(IL)-5 activity enhancement, indicate a poor prognosis (5). However, a study by Kountakis et
al (15) demonstrated that
preoperative and postoperative symptom scores (SNOT-20) of patients
with CRS with nasal polyps are not related to the severity grading
determined by CT, endoscopy and presence of asthma or allergy
symptoms, since ∼25% of the imaging evidence indicated no clinical
symptoms for sinusitis patients.
The pathology of CRS with nasal polyps is a chronic
inflammatory disease. Endoscopic surgery removes irreversible
lesions, opens blocked sinus ostia and creates conditions for the
restoration of normal physiological function of the nasal cavity
and sinus; however, in certain cases with poor outcomes, this is
not successful. Local inflammation has a significant impact on
surgical outcomes. Giger et al (16) identified that, in the middle
turbinate mucosa, non-specific inflammatory cell (lymphocytes and
plasma cells) infiltration density and nasal congestion (VSA
measurement table and nasal resistance meter assessment) are
closely related, which is important in determining the prognosis of
ESS. The degree of infiltration of inflammatory cells in the middle
turbinate mucosa is a good indicator of recurrence following
surgery. Baudoin et al (17) considered that pathological
parameters contribute to the prediction of the presence of certain
chronic nasal-sinusitis symptoms.
In the present study, we conducted Spearman’s
correlation analysis for postoperative symptoms and pathological
indicators of patients with CRS with nasal polyps following nasal
endoscopic surgery. We did not identify indicators related to all
nasal symptoms. It is difficult to predict and assess nasal
symptoms following surgery from only one pathological indicator.
However, we identified pathological indicators of nasal polyp
tissue that are associated with certain symptoms following ESS: i)
The correlation of goblet cell density and sneezing and purulent
nasal discharge is statistically significant (P>0.05) and goblet
cells are pathological indicator that correlate the most with
postoperative symptoms. Baudoin et al (9,17)
identified that the density of goblet cells is associated with
nasal congestion, rhinorrhea, itching, headache and coughing;
therefore, goblet cells are considered most valuable for predicting
postoperative symptoms. ii) The correlation between the number of
pathological glands and dizziness was statistically significant
(P=0.008). Airway epithelial goblet cells and mucosal lamina
propria mucus glands produce mucus. The majority of scholars
consider that in chronic nasal sinusitis, nasal congestion and an
increase of viscous secretions are mainly due to the formation of
new pathological glands, normal mucous gland hyperplasia and
reactivity enhancement (10,11,18,19).
However, the present study did not observe a statistically
significant correlation between the number of pathological glands
and an increase in nasal secretions. We consider that the presence
of dizziness following ESS may be due to a large amount of viscous
secretion that is difficult to discharge, leading to the
obstruction of the sinus ostium. iii) The correlation between the
degree of tissue edema and postnasal drip was statistically
significant (P=0.040). iv) The correlation between the number of
eosinophils and clinical symptoms was not statistically significant
(P>0.05). Lacroix et al identified a significantly
greater number of eosinophils in the polyps and lymphocytes of
African patients while plasmocytes were abundant in polyps from
Chinese and Caucasian individuals (20). In the present study, there was an
increase in eosinophil number in the sinus mucous membrane of ∼50%
of patients with CRS with nasal polyps. There are four main types
of basic protein in eosinophil granule proteins, including ∼50% of
major basic protein (MBP). MBP causes basophils and mast cells to
release histamine, leading to a series of clinical symptoms,
including sneezing, nasal itching and nasal congestion. However, in
this group of patients, we did not identify a significant
correlation between the degree of eosinophil infiltration and
clinical symptoms. v) The correlation between lymphocytic
infiltration density and all clinical symptoms was not
statistically significant (P>0.05).
In the current study, we identified that overall
improvement of patient symptoms with CRS with nasal polyps does not
rely solely on the pathological indicators; however, some
pathological indicators have a certain value in forecasting certain
nasal symptoms. Previous outcome studies have shown that patients
with a poor outcome and high-grade inflammatory load may show
improved results with more radical surgery (21–23).
More studies are required to determine whether patients with a
greater number of goblet cells and pathological glands require more
radical surgery.
References
|
1.
|
Van Crombruggen K, Zhang N, Gevaert P,
Tomassen P and Bachert C: Pathogenesis of chronic rhinosinusitis:
inflammation. J Allergy Clin Immunol. 128:728–732. 2011.PubMed/NCBI
|
|
2.
|
Bernstein JM, Gorfien J and Noble B: Role
of allergy in nasal polyposis: a review. Otolaryngol Head Neck
Surg. 113:724–732. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Senior BA, Kennedy DW, Tanabodee J, Kroger
H, Hassab M and Lanza D: Long-term results of functional endoscopic
sinus surgery. Laryngoscope. 108:151–157. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Bassiouni A, Naidoo Y and Wormald PJ: When
FESS fails: the inflammatory load hypothesis in refractory chronic
rhinosinusitis. Laryngoscope. 122:460–466. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Lavigne F, Nguyen CT, Cameron L, Hamid Q
and Renzi PM: Prognosis and prediction of response to surgery in
allergic patients with chronic sinusitis. J Allergy Clin Immunol.
105:746–751. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Smith TL, Mendolia-Loffredo S, Loehrl TA,
Sparapani R, Laud PW and Nattinger AB: Predictive factors and
outcomes in endoscopic sinus surgery for chronic rhinosinusitis.
Laryngoscope. 115:2199–2205. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Matsuwaki Y, Ookushi T, Asaka D, et al:
Chronic rhinosinusitis: risk factors for the recurrence of chronic
rhinosinusitis based on 5-year follow-up after endoscopic sinus
surgery. Int Arch Allergy Immunol. 146(Suppl 1): S77–S81.
2008.PubMed/NCBI
|
|
8.
|
Ponikau JU, Sherris DA, Kephart GM, et al:
Striking deposition of toxic eosinophil major basic protein in
mucus: implications for chronic rhinosinusitis. J Allergy Clin
Immunol. 116:362–369. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Baudoin T, Kalogjera L, Geber G, Grgić M,
Cupić H and Tiljak MK: Correlation of histopathology and symptoms
in allergic and non-allergic patients with chronic rhinosinusitis.
Eur Arch Otorhinolaryngol. 265:657–661. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Piccirillo JF, Merritt MG Jr and Richards
ML: Psychometric and clinimetric validity of the 20-Item Sino-Nasal
Outcome Test (SNOT-20). Otolaryngol Head Neck Surg. 126:41–47.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Tos M and Mogensen C: Mucus production in
chronic maxillary sinusitis. A quantitative histopathological
study. Acta Otolaryngol. 97:151–159. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Petruson B: Secretion from gland and
goblet cells in infected sinuses. Acta Otolaryngology Suppl.
515:33–37. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Lanza DC and Kennedy DW: Adult
rhinosinusitis defined. Otolaryngol Head Neck Surg. 117:S1–S7.
1997. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Hoffman SR, Dersarkissian RM, Buck SH,
Stinziano GD and Buck GM: Sinus disease and surgical treatment: a
results oriented quality assurance study. Otolaryngol Head Neck
Surg. 100:573–577. 1989.PubMed/NCBI
|
|
15.
|
Kountakis SE, Arango P, Bradley D, Wade ZK
and Borish L: Molecular and cellular staging for the severity of
chronic rhinosinusitis. Laryngoscope. 114:1895–1905. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Giger R, Landis BN, Zheng CQ, et al:
Objective and subjective evaluation of endoscopic nasal surgery
outcomes. Am J Rhinol. 17:327–333. 2003.PubMed/NCBI
|
|
17.
|
Baudoin T, Cupić H, Geber G, Vagić D,
Grgić M and Kalogjera L: Histopathologic parameters as predictors
of response to endoscopic sinus surgery in nonallergic patients
with chronic rhinosinusitis. Otolaryngol Head Neck Surg.
134:761–766. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Majima Y, Masuda S and Sakakura Y:
Quantitative study of nasal secretory cells in normal subjects and
patients with chronic sinusitis. Laryngoscope. 101:1515–1518. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Berger G, Kattan A, Bernheim J and Ophir
D: Polypoid mucosa with eosinophilia and glandular hyperplasia in
chronic sinusitis: a histopathological and immunohistochemical
study. Laryngoscope. 112:738–745. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
20.
|
Lacroix JS, Zheng CG, Goytom SH, Landis B,
Szalay-Quinodoz I and Malis DD: Histological comparison of nasal
polyposis in black African, Chinese and Caucasian patients.
Rhinology. 40:118–121. 2002.PubMed/NCBI
|
|
21.
|
Cutler JL, Duncavage JA, Matheny K, Cross
JL, Miman MC and Oh CK: Results of Caldwell-Luc after failed
endoscopic middle meatus antrostomy in patients with chronic
sinusitis. Laryngoscope. 113:2148–2150. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
22.
|
Murr AH: Contemporary indications for
external approaches to the paranasal sinuses. Otolaryngol Clin
North Am. 37:423–434. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
23.
|
Videler WJ, van Drunen CM, van der Meulen
FW and Fokkens WJ: Radical surgery: effect on quality of life and
pain in chronic rhinosinusitis. Otolaryngol Head Neck Surg.
136:261–267. 2007. View Article : Google Scholar : PubMed/NCBI
|