Introduction
Acetabular dysplasia (AD) is a developmental
dysplasia of the hip (DDH), and is also known as hip joint
instability. The characteristic pathological change in AD is a
shallow acetabulum that leads to insufficient acetabular
containment and coverage of the femoral head; however, radiographic
observations have demonstrated that the femoral head remains in the
true acetabulum (1). Studies from
China have revealed that 50–60% of the patients who received a
total hip arthroplasty (THA) suffered from osteoarthritis (OA)
secondary to hip dysplasia, and a large number of adult AD patients
ultimately undergo a total hip replacement (2,3). It
has previously been suggested that the femoral and acetabular
anatomical malformations that are apparent with AD increase
gradually, in correlation with femoral head displacement (4). Since the patients with these
anatomical malformations rarely develop further hip subluxations
and dislocations, the majority of doctors do not consider the
disorder to be a significant disability. However, anatomical
variations of the acetabulum and proximal femoral medullary cavity
are irregular (5), and
preoperative X-rays do not identify all patients with AD; the
correlation of the X-ray results with intraoperative findings
varies greatly. A femoral neck fracture with AD is easily missed in
clinical practice, and often leads to postoperative dislocation
(6). The Crowe classification
describes the proximal migration of the femoral head, regardless of
the acetabular deformity, and assumes that there is a direct
interrelation between the extent of the migration and the severity
of disease (7). By contrast, the
Hartofilakidis classification relies on the anatomy of the
acetabulum, as encountered during surgery (8). However, the two classifications are
not always valid, since the anatomy of the acetabulum and femur is
variable, and the extent of migration is not a definite criterion
for judging the type of dysplasia (8,9).
Therefore, these classifications have limited uses as surgical
guides, and for the selection of a suitable prosthesis.
Furthermore, there is no specialized classification for mild DDH,
such as AD.
With the increasing prevalence of THA, the incidence
of adverse results, such as a fracture in the region surrounding
the prosthesis and dislocation, has increased at follow-up. These
adverse effects are often correlated with improper intraoperative
management, most notably the implantation of a conventional
prosthesis into an abnormal medullary cavity (10). The correct placement of a suitable
prosthesis is the sole method of preventing adverse effects, and
ensuring the long-term stability of the prosthesis. Thus, a more
effective clinical classification is required to guide surgery.
Following an analysis of previous studies, we propose, in the
present study, a novel method of assessing acetabular and femoral
deformities.
Materials and methods
Patients
From 2007 to 2011, 63 consecutive patients who were
diagnosed with OA secondary to developmental dysplasia, or femoral
neck fracture with developmental dysplasia, and who would accept a
THA, were treated at Shanghai Sixth People’s Hospital (Shanghai,
China). The patient cohort consisted of 14 males and 49 females,
with a mean age of 55.6±12.5 years (range, 18–83 years). A total of
55 were diagnosed with OA, and eight with a femoral neck fracture.
Patients who had undergone acetabular or femoral osteotomies or who
suffered from rheumatoid arthritis were excluded from
participation. In addition, patients in whom the dysplasia may have
been affected by a neurological illness or Legg-Calvé-Perthes
disease were also excluded. There were 32 cases of bilateral and 31
cases of unilateral AD. A total of 10 patients underwent a
bilateral THA. Three-dimensional computed tomography (3DCT) was
used to clarify whether a deformity existed and, if the result was
positive, to identify the degree of acetabular or femoral deformity
(11,12). A total of 30 acetabula or femurs
were not able to be located in the normal anatomical sites, due to
a significant acetabular or femoral deformity, out of 73 dysplastic
hips. The study was conducted in accordance with the Declaration of
Helsinki and with approval from the Ethics Committee of Shanghai
Sixth People’s Hospital. Written informed consent was obtained from
all participants.
Radiographic evaluation
The radiographic evidence of AD included a
central-edge angle of Wiberg (CE angle) <20° on the
anteroposterior radiographs (13),
and a Sharp angle >45° for the Crowe type I subluxation
(14). In Crowe type I DDH, the
vertical subluxation of the hip (measured from the inferior margin
of the tear drop to the head-neck junction) is <50% of the
diameter of the femoral head (or <10% of the height of the
pelvis) (7). CT scans were
acquired at a thickness of 1.2 mm, and a table speed of 3.0 mm/s,
using a helical scanner (GE Lightspeed 16 Slice CT scanner, GE
Healthcare, Waukesha, WI, USA). The helical scanning was conducted
at 140 kVp and 300 mAs, and the field of view was 500 mm.
Classifying the abnormalities using 3DCT involved basic scanning,
ranging from 5 cm above the acetabular roof to the femoral
condyles. The CT data were transferred digitally to Digital Imaging
and Communications in Medicine (DICOM, version 3.0; National
Electrical Manufacturers’ Association, Rosslyn, VA, USA), where the
images were formatted (512×512 pixels), prior to the retrieval of
the images using a compact disc or a digital versatile disc. These
retrieved data were transferred to a personal laptop computer (IBM
Lenovo Thinkpad X220i, Lenovo, Inc., Beijing, China), and the 3D
bone images of the acetabulum and femur were reconstructed and
analyzed using Intage Realia software (KGT, Inc., Tokyo, Japan).
The original data were reconstructed in 1 mm intervals on coronal
and sagittal images of the hip joint (12). Two experienced hip surgeons, who
were responsible for performing >200 cases each year,
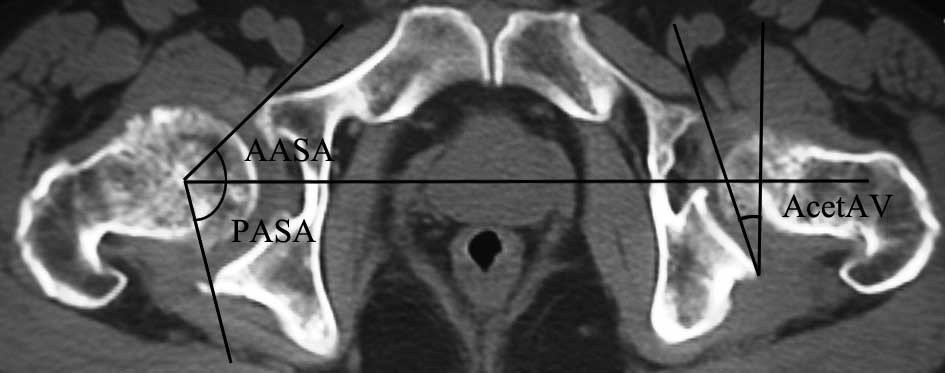
subsequently measured the following parameters, twice (8): i) Anterior acetabular section angle
(AASA), i.e. the angle between the centerline extending between the
bilateral femoral heads, and the line from the center of the head
to the anterior margin of the acetabulum (59–83° and 53–92° in
normal males and females, respectively (12); Fig.
1); ii) posterior acetabular section angle (PASA), i.e. the
angle between the centerline extending between the bilateral
femoral heads, and the line from the center of the head to the
posterior margin of the acetabulum [84–116° and 87–120° in normal
males and females, respectively (12); Fig.
1)]; iii) acetabular anteversion angle (AcetAV), i.e. the angle
between the line extending between the anterior and posterior
margins of the acetabulum, and the line perpendicular to the center
line connecting the bilateral femoral heads (12) (Fig.
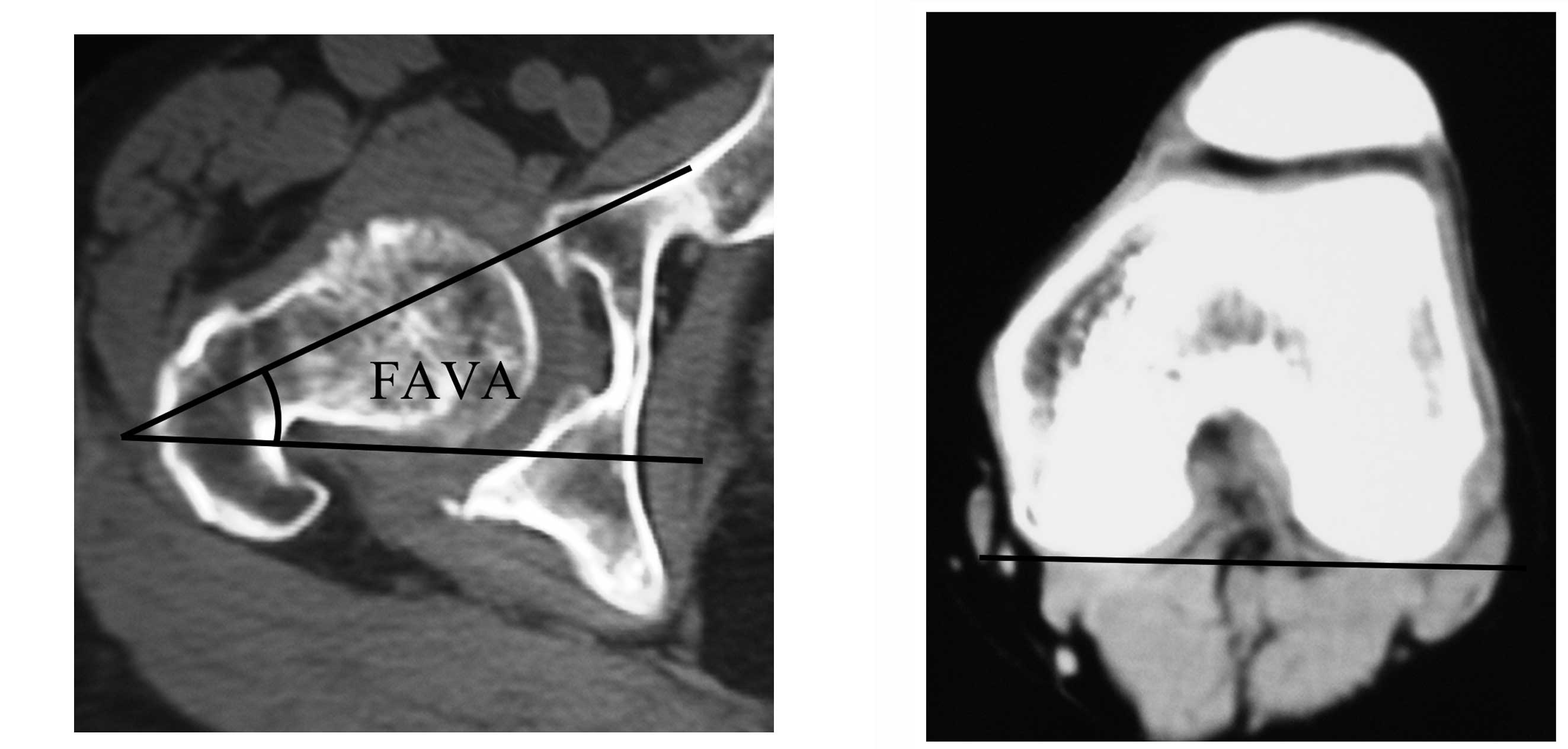
1); iii) femur anteversion angle (FAVA) (15) (Fig.
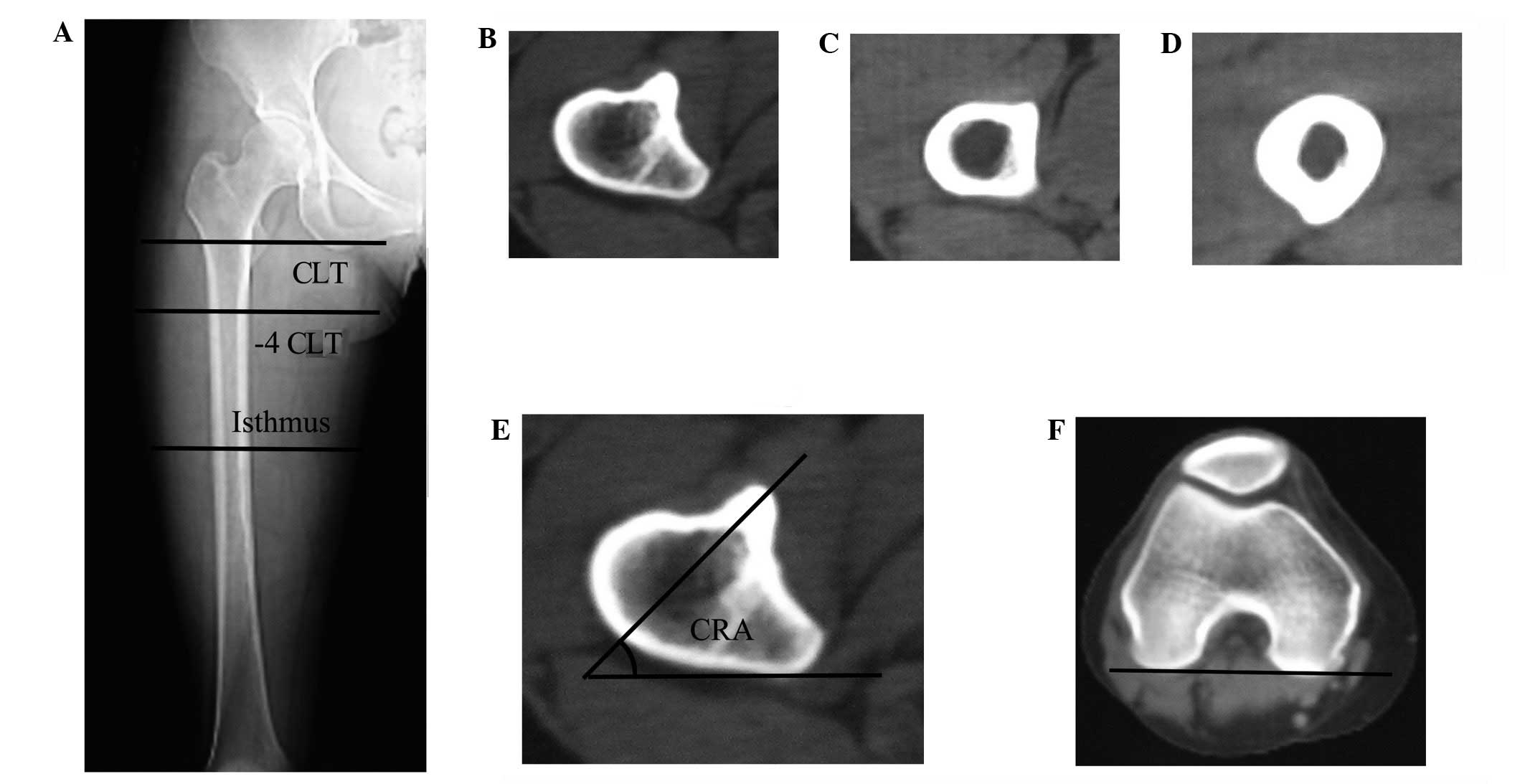
2); iv) canal rotation angle (CRA), i.e. the angle between the
major axis of the ellipses of best fit to the endosteal surface of
the femoral canal, and a tangent to the posterior aspect of the
femoral condyles (4,11) (Fig.
3); v) medio-lateral and vi) antero-posterior canal width at
the level of the canal isthmus (the maximum value of the
medio-lateral or antero-posterior extracortical diameter of the
diaphysis was also recorded); and vii) canal diameter at the
isthmus (the point of the medullary canal with the smallest
cross-sectional area). The mean of the normal population was used
as the control (4,11). Forty-six healthy controls with
normal hip anatomy were also assessed, including 11 males and 35
females, with a mean age of 56.7±11.7 years (range, 25–80
years).
Classification
The acetabular abnormalities were classified into
A1-type anterior, A2-type posterior and A3-type lateral (including
mild and global) deficiencies (Table
I) (12). The femoral
classification was as follows: F1-type, FAVA <30°; F2-type, 30°≤
FAVA ≤40°, with mild abnormalities of the femoral canal rotation
and the diameter at the isthmus; F3-type, FAVA >40°, with
significant abnormalities of the femoral canal rotation and the
diameter at the isthmus (Tables II
and III). There were 21 A1-type
cases (26 hips), nine A2-type cases (13 hips) and 33 A3-type cases
(34 hips). In addition, there were 33 F1-type cases (35 hips), 26
F2-type cases (32 hips) and four F3-type cases (six hips).
 | Table I.Classification of acetabular
dysplasia. |
Table I.
Classification of acetabular
dysplasia.
| Parameter | A1-type anterior
deficiency | A2-type posterior
deficiency | A3-type lateral
deficiency
|
|---|
| Mild deficiency | Global
deficiency |
|---|
| AASA | <50° | ≥50° | ≥50° | <50° |
| PASA | ≥90° | <90° | ≥90° | <90° |
 | Table II.Comparison of computed tomography
measurements among the different types of acetabular
deficiency. |
Table II.
Comparison of computed tomography
measurements among the different types of acetabular
deficiency.
| Group | n | CE angle (°) | Sharp angle (°) | AcetAV (°) | AASA (°) | PASA (°) |
|---|
| A1-type | 26 | 12.7±7.1a | 50.2±3.1a | 22.5±1.8a | 48.3±2.4a | 93.3±6.0 |
| A2-type | 13 | 13.5±4.2a | 49.9±4.3a | 14.0±3.4a | 60.2±3.1a | 78.2±4.0a |
| A3-type | 34 | 11.9±5.7a | 52.1±5.0a | 19.6±4.6 | 54.6±8.5a | 88.4±10.1a |
| Control | 46 | 31.0±4.3 | 35.9±2.9 | 19.8±3.7 | 75.9±8.6 | 95.3±6.0 |
 | Table III.Anatomical parameters of control and
dysplastic femurs, based on the different types of acetabular
dysplasia. |
Table III.
Anatomical parameters of control and
dysplastic femurs, based on the different types of acetabular
dysplasia.
| Parameters | Control (n=46) | F1-type (n=35) | F2-type (n=32) | F3-type (n=6) |
|---|
| Medio-lateral canal
width at isthmus (mm) | 12.4±1.4 | 12.3±1.5 | 11.7±1.3a | 11.1±0.5a |
| Antero-posterior
canal width at isthmus (mm) | 13.6±1.4 | 13.4±1.6 | 12.8±1.3a | 12.2±0.7a |
| Canal diameter at
isthmus (mm) | 10.3±1.4 | 10.4±1.7 | 9.7±1.2a | 8.9±0.4a |
| Canal rotation
angle (°) | | | | |
| At CLT | 45.2±3.7 | 46.4±2.7 | 48.6±2.0a | 52.1±2.1b |
| CLT-4 cm | 49.8±3.4 | 50.7±2.7 | 54.0±3.2a | 58.6±1.1b |
| At isthmus | 85.2±3.6 | 84.1±2.5 | 82.4±1.6a | 79.8±1.8b |
| FAVA(°) | 18.6±5.0 | 25.8±1.5a | 32.2±2.5a | 45.0±3.7b |
Statistical analysis
The database was established via statistical
analysis using SPSS 19.0 (SPSS, Inc., Chicago, IL, USA). For
variables that were normally distributed, differences between the
types were evaluated using analysis of variance (ANOVA), followed
by the unpaired t-test for multiple pair-wise comparisons of all
significant variables. Categorical data were compared using the
χ2 test. To assess the intraobserver reliability of the
different parameters of the femur or the acetabulum, the
preoperative radiographs for each patient were templated by an
investigator, who subsequently repeated the templating two weeks
later. In addition, the templating procedure was repeated by a
second investigator, independently. The intra- and interobserver
effects were calculated using an intraclass correlation coefficient
(ICC) (8). Pearson’s correlation
coefficient was used to assess the correlations between various
measurements. P<0.05 was considered to indicate a statistically
significant difference (Tables II
and III).
Results
When the acetabular and femoral abnormalities were
divided into subgroups, using 3DCT, it was observed that there was
a crossover between each of the femoral subtypes (F1, F2 and F3)
and the acetabular subtypes (A1, A2, or A3), with the exception
that the F3-type deficiency did not appear in conjunction with the
A2-type deficiency. Significant differences were demonstrated in
the AcetAV (P<0.05), AASA (P<0.05) and PASA (P<0.05)
between the A1, A2 and A3-type deficiencies (A1 versus A2, A1
versus A3 and A2 versus A3); however, no significant differences
were observed in the CE angle (P>0.05) or the Sharp angle
(P>0.05). The AASA values of the A1, A2 and A3-type deficiencies
were significantly different from that of the control group
(P<0.05), whereas only the PASA values of the A2 and A3-type
deficiencies were significantly different in comparison with the
PASA value of the control group (P<0.05; Table II). There was a significant
Pearson’s correlation between the AASA and the AcetAV (r=−0.353,
P=0.002), and between the PASA and the AcetAV (r= 0.5, P= 0.001),
indicating that hips with a greater AASA also had a lower AcetAV,
and that those with a greater PASA also had a higher AcetAV. No
significant differences were observed in the AcetAV between the
A3-type deficiency and the control (t=0.102, P=0.92). The intra-
and interobserver reliability values of the acetabular
classification, obtained using ICC, were 0.843 and 0.862,
respectively, which indicated good reproducibility in the
acetabular measurements.
Table III displays
the canal width at the level of the isthmus in the antero-posterior
and medio-lateral directions, and the canal diameter at the
isthmus; significant differences were observed between the control
and the F2 and F3-type deficiencies (P<0.05), but not between
the control and the F1-type deficiency (P>0.05). There was no
significant difference in the canal diameter at the isthmus between
the F2 and F3-type deficiencies (P=0.336), although the mean
diameter of the canal of the F3-type femurs was smaller than that
of the F2-type femurs (8.9 mm versus 9.7 mm). The CRAs at the three
levels were significantly different between the F2 and F3-type
deficiencies (P<0.05). There were no significant differences in
the CRAs between the F1-type deficiency and the control cases;
however, significant differences were observed in a comparison
between the F2 and F3-type deficiencies and the control
(P<0.05). From the center of the lesser trochanter (CLT) to the
medullary cavity of the isthmus, a gradual increase was observed in
the CRA. However, it was observed that there was a significantly
higher mean increase in the CRA from the CLT to the isthmus in the
control cases (40°), in comparison with that of the F2 (34°) and F3
(28°)-type deficiencies. The variation in femoral anteversion in
the F3-type deficiency was of a greater significance than that in
the F1 and F2-type hips (P<0.05). It was observed that femurs
with a greater FAVA also appeared to have narrower canals
(r=−0.315, P=0.007), and a smaller CRA at the isthmus (r=−0.696, P=
0.007).
There was no significant correlation between the
FAVA and the AcetAV in the dysplastic hips overall (r=0.001,
P=0.996). However, when the hips were divided into subgroups, a
significant positive correlation was observed between the FAVA and
the AcetAV in the anterior deficiency subgroups (r= 0.394, P=
0.046). By contrast, there was no significant correlation between
the FAVA and the AcetAV in the posterior and global deficiency
subgroups (r=−0.006, P=0.973; and r=0.038, P=0.829, respectively).
The intra- and interobserver reliability values of the femoral
classification, obtained using ICC, were 0.813 and 0.822,
respectively, which indicated that there was an acceptable
reliability in the femoral measurements. There were no significant
differences in the average age (t=0.585, P= 0.561) or gender
(χ2= 0.040, P= 0.836) of the 63 patients with AD
compared with the 46 healthy controls. In the control hips, no
significant correlations were observed between the FAVA and the
AcetAV, Sharp angle or CE angle (r=−0.115, P= 0.448; r= 0.041, P=
0.785; and r= 0.026, P= 0.078, respectively). However, there was a
significant positive correlation between the FAVA and the Sharp
angle (r=0.456, P=0.00), and a significant negative correlation
between the FAVA and the CE angle (r=−0.473, P=0.00) in the
dysplastic hips.
Discussion
In this study of 73 dysplastic hips and 46 normal
hips, the morphological differences between dysplastic and normal
hips were observed, and significant correlations between the AcetAV
and the acetabular anterior or posterior deficiency subgroups were
identified. In addition, it was demonstrated that there was a
significant correlation betwen the femoral anteversion and the
AcetAV in the anterior deficiency subgroup. It was revealed by
Akiyama et al (5) that
changes in the AASA, PASA and AcetAV may be detected by 3DCT, and
that 3DCT clearly exhibits the location and extent of the
dysplasia. In a study by Ito et al (12), 22 of 84 AD hips (26%) were
classified as having an anterior deficiency; 17 (20%), a posterior
deficiency; and 45 (54%), a lateral deficiency. Hips with poor
anterior acetabular support were defined as those with an AASA
<50°, while hips with poor posterior support were defined as
those with a PASA <90° (12).
In a previous study, the AASA, PASA, and AcetAV measurements were
demonstrated to be effective for the precise evaluation of various
acetabular deficiencies (16).
Anda et al (17) revealed
that the AcetAV in the anterior deficiency subgroup was
significantly larger than in the other groups. By contrast, the
AcetAV in the posterior deficiency subgroup has been observed to be
smaller than that in the normal and global deficiency subgroups
(5). The results of these studies
supported the observations in the present study. In addition, the
results of the present study demonstrated a trend towards increased
or decreased acetabular anteversion in shallow hips with poor
anterior or posterior support.
The previously mentioned results indicated the
existence of a potential developmental interaction between the
femur and acetabulum. When the dysplastic hips were divided
according to the location of the acetabular bone defect,
significant differences in acetabular version were observed among
the subgroups. It was demonstrated that hips with a larger FAVA
appeared to additionally have an increased AcetAV, indicating a
biomechanical cycle resulting in the pathology of dysplastic hips
with anterior acetabular deficiency (5). By contrast, no correlation in version
was observed in hips with a posterior or global deficiency.
However, it was demonstrated that there was a significant
correlation between the FAVA and the Sharp/CE angles in the
dysplastic acetabula.
Although the previous studies indicated that each
type of dysplasia was correlated with the degree of the dysplasia,
rather than the specific type of severity, they did not offer a
systematic and detailed guide for THA. The large individual
acetabular morphological variability across all levels of dysplasia
observed in this study demonstrated that it is not possible to
select an acetabular prosthesis for dysplastic hips on the basis of
the severity of the subluxation alone. The results of the study
suggested that there is a requirement for the surgeon to choose the
type of socket implantation according to the type and extent of the
acetabular defect, and to adapt to the individual FAVA. Thus, it is
necessary for each patient be considered individually, in order
that the angle of the acetabular cup may be customized to suit
(9). For the A1-type deficiency, a
reduction in the AcetAV or a neutral position is required when the
cup is implanted. In cases with an excessive FAVA, a decrease in
the FAVA is required for the inclusion and congruity of the hip
joint (5). For the A2-type
deficiency, an appropriate increase in the AcetAV is required to
resolve the initial instability, in order to prevent the
aggravation of the posterior acetabular insufficiency. In the
present study, no significant differences were found in the AcetAV
between the A3-type deficiency (mild or global) and the control
group. The acetabular defects predominantly occurred on the upper
and lateral margins of the acetabulum, although anterior and
posterior deficiencies were also observed with the global
deficiency. Due to the absence of structural bone defects in the
acetabula, and since the acetabular cup covers >70% of the bone
bed, there is a requirement for the acetabular cup to be placed at
the center of the acetabulum, and for normal anteversion to be
maintained (2). Since mild or
global deficiencies of the acetabulum require similar methods of
prosthetic implantation, hips with these types of deficiency may be
classified as having a lateral deficiency (12). The treatment of femoral
abnormalities or variations with A1, A2 or A3-type deficiencies are
described in greater detail later in this study.
The present study revealed the morphological
characteristics of dysplastic femurs, and investigated the effects
of the disorder on the geometry of the intramedullary canal. These
results were then compared with a control group. It was
demonstrated that in cases with excessive anteversion, the
dysplastic femurs were smaller than the control femurs, with
narrower, straighter and less-tapered canals. Sugano et al
and Noble et al (4,11) observed that the 3D anatomy of a
femur with the mildest degree of subluxation (Crowe type I)
exhibited a significantly different FAVA and medullary cavity
rotation, and that several patients had a FAVA >60°. In
addition, it was demonstrated that the diameter of the femoral
medullary cavity was reduced in the Crowe type I femurs. The
minimum diameter of the canal in the Crowe type I femurs was 1 mm
less than in the control femurs (4,11).
Argenson et al (9) revealed
that the mean diameter of the medullary cavity was >1.6 mm
narrower in the antero-posterior and >1.9 mm narrower in the
medio-lateral position in the Crowe type I than in the control
femurs (9,11). The canal flare and metaphyseal
canal flare indices were used to assess variations in the width of
the femoral medullary cavity on anteroposterior radiographs
(18). X-rays are only able to
assess the femoral marrow cavity in two dimensions; however, with
the exception of the differences in canal width, it is important
that the morphological characteristics of the femoral medullary
cavity at different levels are identifiable with 3DCT. Therefore,
the measurements were performed in three dimensions, i.e. in the
axial, coronal and sagittal planes (19). It was observed that the normal
rotation angle of the medullary canal gradually increased from the
CLT to the isthmus. However, in the dysplastic femurs, the
increased ante-version of the proximal femur resulted in a
reduction in the rotation in the medullary canal, predominantly in
the region from the CLT to the canal at the isthmus (4,11).
The variation between the F2 and F3-type deficiencies supported
this observation. With regard to surgery, this variation is
critical, since it is necessary to be aware of variations in the
width of the medullary cavity when the femoral canal is reamed, in
order to avoid femoral fractures. When the femoral stem is
implanted, there is a requirement for the morphological differences
that occur at different levels of the medullary cavity to be
considered, in order to ensure that the prosthesis closely matches
the medullary cavity of the femur. Therefore, when the FAVA is
exaggerated, the rotational orientation has a marked effect on the
size and shape of the canal (11),
and the concomitant twist of the femoral canal increases the
difficulty of the joint replacement.
The results of the present study demonstrated that
the position of the femoral anterior arch in the femurs with AD was
not significantly different from that observed in the control
group. This indicated that the primary anatomical feature affecting
the successful placement of the stem is increased femur
anteversion, leading to secondary rotational anomalies and a
narrowing of the canal at the isthmus. Therefore, these features
were the basis of our classification (4,9).
With regard to the F1-type deficiency (FAVA <30°), femoral stem
implantation with a normal FAVA is possible. For the F2-type
deficiency (30°≤ FAVA <40°, with mild abnormalities of the
femoral canal rotation and the isthmus diameter) it may be
appropriate to adjust the FAVA from 15° to 25°, due to the
anteversion of the acetabular cup. However, following femoral neck
osteotomy, the cross-section of the long axis of the femur is not
usually consistent with that required by the femoral stem. If a
proximal fixed prosthesis is chosen, stability is poor; therefore,
in the majority of cases a prosthesis with a straight and thin
distal stem is required to accommodate this diaphyseal femoral
anatomy (20). With regard to
F3-type deficiencies, with significant abnormalities of the femoral
canal rotation and a reduced isthmus diameter, it has been
demonstrated that modular or customized components are necessary,
in order to accommodate the shape of these dysplastic canals
(21,22). Furthermore, the present study
indicated that the templating technique exhibited the desired
reliability, with all the ICC values exceeding 0.8 (8).
A retrospective database and image review was used
to summarize the diversity of mild dysplasia; this reinforced the
observations of a number of previous studies, concerning the
exaggerated anteversion in mildly dysplastic femurs. At present,
the majority of doctors do not consider the disorder of mild
dysplasia to be a great disability, and, furthermore, preoperative
3DCT scans are not routinely requested for Crowe type I hips, due
to the additional medical expense. However, the present study
revealed the anatomical variations of the acetabulum and proximal
femoral medullary cavity to be irregular and interrelated (∼41.1%
of cases), and preoperative X-rays and 2DCT scans of the hip joint
are not able to identify any correlation between these variations.
It is therefore important that the results of 3D scans are assessed
preoperatively, and that any interrelation between the femoral and
acetabular morphologies is identified by the surgeons. The aim of
this investigation was to emphasize the morphological variations in
mild dysplasia, particularly in the femoral medullary cavity and
the acetabulum, as a primary step to determining the potential
requirements for surgical procedures. The results of this study are
likely to provide a greater insight into the morphological
characteristics of dysplastic hips, and the challenges confronting
joint replacement surgeons.
In addition to suggesting a novel anatomic
classification, this study provided a detailed characterization of
the anatomical variations to be considered in hip arthroplasty
implants for patients with AD. The purpose of this 3D morphometric
analysis was to serve as an anatomical reference for acetabular and
femoral implants. The novel classification employed in this study
used 3DCT measurements to clarify the location and extent of
acetabular deficiency, the diameter of the medullary cavity at the
isthmus and the degree of rotational deformity. This is likely to
facilitate the improved management of malformations of the
acetabulum and femur, and to ensure the selection of a suitable
prosthesis. Since the initial assessment of the patients with AD
has been adopted, the individualized prosthesis implantation and
surrounding bone matching have achieved the desired results,
thereby increasing the long-term survival rates of the
prostheses.
Acknowledgements
This study was supported by the
Interdisciplinary (Engineering-Medical) Research Fund of Shanghai
Jiao Tong University (grant no. YG2011MS30), Shanghai Municipal
Health Bureau Science Fund for Young Scholars (grant no.
2010QJ036A), the Opening Project of the State Key Laboratory of
High Performance Ceramics and Superfine Microstructure (grant no.
SKL201206SIC) and the National Natural Science Foundation of China
(grant no. 81171688).
References
|
1.
|
Hartofilakidis G, Yiannakopoulos CK and
Babis GC: The morphologic variations of low and high hip
dislocation. Clin Orthop Relat Res. 466:820–824. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Xu WD, Li J, Zhou ZH, Wu YS and Li M:
Results of hip resurfacing for developmental dysplasia of the hip
of Crowe type I and II. Chin Med J (Engl). 121:1379–1383.
2008.PubMed/NCBI
|
|
3.
|
Jasty M, Anderson MJ and Harris WH: Total
hip replacement for developmental dysplasia of the hip. Clin Orthop
Relat Res. 311:40–45. 1995.PubMed/NCBI
|
|
4.
|
Sugano N, Noble PC, Kamaric E, Salama JK,
Ochi T and Tullos HS: The morphology of the femur in developmental
dysplasia of the hip. J Bone Joint Surg Br. 80:711–719. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Akiyama M, Nakashima Y, Fujii M, et al:
Femoral anteversion is correlated with acetabular version and
coverage in Asian women with anterior and global deficient
subgroups of hip dysplasia: a CT study. Skeletal Radiol.
41:1411–1418. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Spangehl MJ, Berry DJ, Trousdale RT and
Cabanela ME: Uncemented acetabular components with bulk femoral
head autograft for acetabular reconstruction in developmental
dysplasia of the hip: results at five to twelve years. J Bone Joint
Surg Am. 83-A:1484–1489. 2001.PubMed/NCBI
|
|
7.
|
Jawad MU and Scully SP: In brief: Crowe’s
classification: arthroplasty in developmental dysplasia of the hip.
Clin Orthop Relat Res. 469:306–308. 2011.PubMed/NCBI
|
|
8.
|
Yiannakopoulos CK, Chougle A, Eskelinen A,
Hodgkinson JP and Hartofilakidis G: Inter- and intra-observer
variability of the Crowe and Hartofilakidis classification systems
for congenital hip disease in adults. J Bone Joint Surg Br.
90:579–583. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Argenson JN, Flecher X, Parratte S and
Aubaniac JM: Anatomy of the dysplastic hip and consequences for
total hip arthroplasty. Clin Orthop Relat Res. 465:40–45.
2007.PubMed/NCBI
|
|
10.
|
Shen B, Yang J, Wang L, Zhou ZK, Kang PD
and Pei FX: Midterm results of hybrid total hip arthroplasty for
treatment of osteoarthritis secondary to developmental dysplasia of
the hip-Chinese experience. J Arthroplasty. 24:1157–1163. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Noble PC, Kamaric E, Sugano N, Matsubara
M, Harada Y, Ohzono K and Paravic V: Three-dimensional shape of the
dysplastic femur: implications for THR. Clin Orthop Relat Res.
417:27–40. 2003.PubMed/NCBI
|
|
12.
|
Ito H, Matsuno T, Hirayama T, Tanino H,
Yamanaka Y and Minami A: Three-dimensional computed tomography
analysis of non-osteoarthritic adult acetabular dysplasia. Skeletal
Radiol. 38:131–139. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Paliobeis CP and Villar RN: The prevalence
of dysplasia in femoroacetabular impingement. Hip Int. 21:141–145.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Omeroglu H, Bicimoglu A, Agus H and Tumer
Y: Acetabular development in developmental dysplasia of the hip. A
radio-graphic study in anatomically reduced and uncomplicated hips.
Bull NYU Hosp Jt Dis. 65:276–279. 2007.PubMed/NCBI
|
|
15.
|
Sugano N, Noble PC and Kamaric E: A
comparison of alternative methods of measuring femoral anteversion.
J Comput Assist Tomogr. 22:610–614. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Tallroth K and Lepistö J: Computed
tomography measurement of acetabular dimensions: normal values for
correction of dysplasia. Acta Orthop. 77:598–602. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Anda S, Terjesen T, Kvistad KA and
Svenningsen S: Acetabular angles and femoral anteversion in
dysplastic hips in adults: CT investigation. J Comput Assist
Tomogr. 15:115–120. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Casper DS, Kim GK, Parvizi J and Freeman
TA: Morphology of the proximal femur differs widely with age and
sex: relevance to design and selection of femoral prostheses. J
Orthop Res. 30:1162–1166. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Memon AR, Butler J, Guerin S, Galbraith J,
Flanagan O and Harty J: Proximal femoral anatomy in total hip
arthroplasty. A tri-planar computed tomographic assessment. Acta
Orthop Belg. 77:488–493. 2011.PubMed/NCBI
|
|
20.
|
Schmidutz F, Beirer M, Weber P, Mazoochian
F, Fottner A and Jansson V: Biomechanical reconstruction of the
hip: comparison between modular short-stem hip arthroplasty and
conventional total hip arthroplasty. Int Orthop. 36:1341–1347.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
21.
|
Ito H, Tanino H, Yamanaka Y, Nakamura T
and Matsuno T: Hybrid total hip arthroplasty using
specifically-designed stems for patients with developmental
dysplasia of the hip. A minimum five-year follow-up study. Int
Orthop. 35:1289–1294. 2011.PubMed/NCBI
|
|
22.
|
Sakai T, Sugano N, Ohzono K, Nishii T,
Haraguchi K and Yoshikawa H: Femoral anteversion, femoral offset,
and abductor lever arm after total hip arthroplasty using a modular
femoral neck system. J Orthop Sci. 7:62–67. 2002. View Article : Google Scholar : PubMed/NCBI
|