Introduction
The majority of injuries to the great vessels in the
clavicular region are caused by penetrating trauma, which often
results in uncontrollable hemorrhage and brachial plexus injury.
Recently, coated endovascular stent grafting has been used to treat
injuries to the great vessels in the clavicular region (1,2), and
balloon-expandable and self-expandable endovascular intervention
has successfully treated patients with false aneurysms in these
vessels following injury (3,4).
However, these methods have certain limitations. In the present
study the patient presented with an injury to the proximal segment
of the axillary artery complicated by brachial plexus injury and
was treated with emergency coated endovascular stent placement
under C-arm fluoroscopy guidance on July 31, 2010. The patient was
followed up for 13 months and the results were favorable.
Case report
A 31-year-old male was injured by baamboo and was
admitted to Fuding People’s Hospital (Fuding, China) for wound
debridement and suturing. However, the patient was transferred to
The Affiliated Hospital of Wenzhou Medical College (Wenzhou, China)
due to progressive swelling and numbness of the right chest wall
and absence of pulses in the right upper limb. Physical examination
showed that the patient was anemic, with a reduced level of
consciousness, clear breath sounds bilaterally and blood pressure
<70/40 mmHg in the left upper limb following volume expansion.
Oxygen saturation of the right upper limb was 0% and the pulse rate
was 110 bpm. There were two right thoracic wounds; a 2-cm wound
located 1.5 cm below the medial end of the clavicle, and a 3-cm
wound located below the lateral end of the clavicle in the anterior
axillary fossa. The wounds were sutured, with evident capillary
hemorrhage in the wound at the lateral end of the clavicle. The
right chest wall and the right upper limb were swollen. The right
axillary, brachial and ulnar pulses were absent, and there was no
capillary return in the fingers. Traction on the limb produced pain
and increased numbness. Muscle strength was grade II and muscle
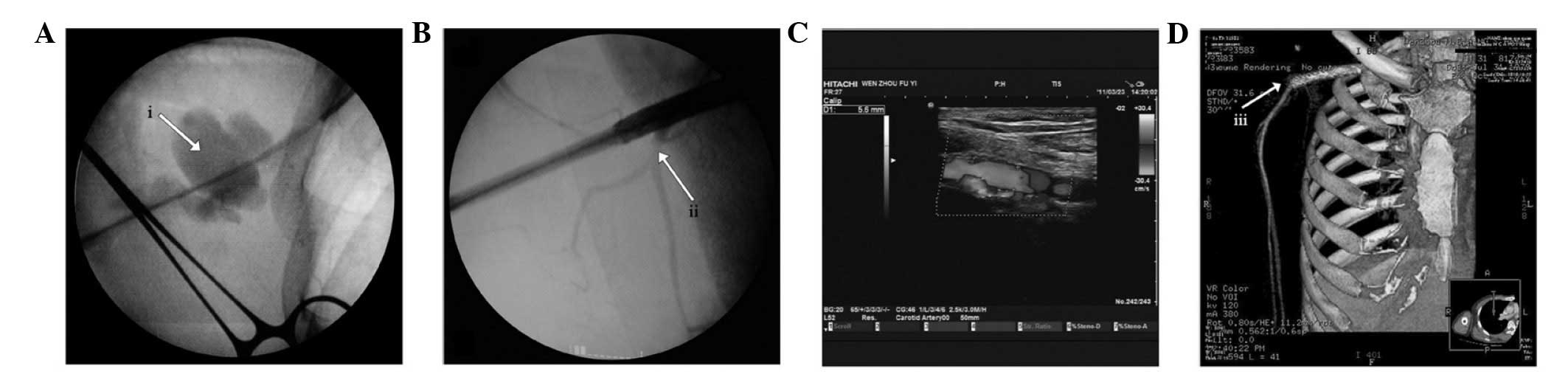
tone was normal. Thoracic CT scan images are shown in Fig. 1. The patient was diagnosed with
hemorrhagic shock, right axillary artery injury, right brachial
plexus injury, right scapular fracture, damage to the right
shoulder muscles and a large right shoulder hematoma. This study
was approved by the ethics committee of First Affiliated Hospital
of Wenzhou Medical College. The informed consent was obtained from
the patient.
Color ultrasonography showed an injury at the
junction of the right subclavian artery and the axillary artery.
Emergency repair of the injury was performed under general
anesthesia with tracheal intubation. A longitudinal incision was
made on the medial aspect of the right upper arm and an
endovascular stent delivery catheter system was inserted into the
brachial artery. C-arm fluoroscopy-guided arteriography showed
leakage of contrast medium from the proximal segment of the
axillary artery and the distal vessels were not visualized
(Fig. 1A). A 5-cm Wallgraft
artificial coated endovascular stent with Unistep Plus propulsion
system (Boston Scientific Ireland Ltd., Galway, Ireland) was placed
in the injured vessel. Arteriography following stent placement
showed contrast medium passing normally through the proximal
axillary artery, with distal and collateral vessels clearly
visualized (Fig. 1B). Radial and
ulnar pulses were palpable following the procedure, but limb
swelling increased following the intervention, possibly due to
ischemia/reperfusion injury and venous injury. Considering the
signs of brachial plexus injury, an exploratory surgery was
performed immediately. During the surgery, exploration revealed a
false aneurysm in the proximal segment of the axillary artery.
Following removal of the hematoma, a 1.5-cm U-shaped wound was
covered with a coated endovascular stent. Gauze was used to stop
bleeding and the ruptured accompanying vein was ligated. There was
no disruption of the brachial plexus and the surrounding hematoma
was removed. Clopidogrel was administrated orally for 2 weeks to
inhibit platelet aggregation postoperatively.
One week after injury, a CT scan of the right
clavicular region showed that the stent was correctly positioned
and patent, with no surrounding false aneurysm. A second-look
surgery was performed to remove the gauze and the organized blood
clot surrounding the stent. Doppler ultrasonography (Fig. 1C) and CT arteriography (CTA;
Fig. 1D) were performed at 1, 3
and 6 months after the second-look surgery, and showed a patent
coated endovascular stent, normal blood flow wave pattern, and the
right upper limb with 97–100% oxygen saturation on finger pulse
oximetry.
After injury, traction on the right upper limb
produced pain and increased numbness, and muscle strength was grade
II. During the first surgery, a false aneurysm was found in the
proximal segment of the axillary artery, with surrounding hematoma
causing brachial plexus compression. The hematoma was removed to
decompress the brachial plexus. One week after the initial surgery,
a second-look surgery was performed to examine the brachial plexus
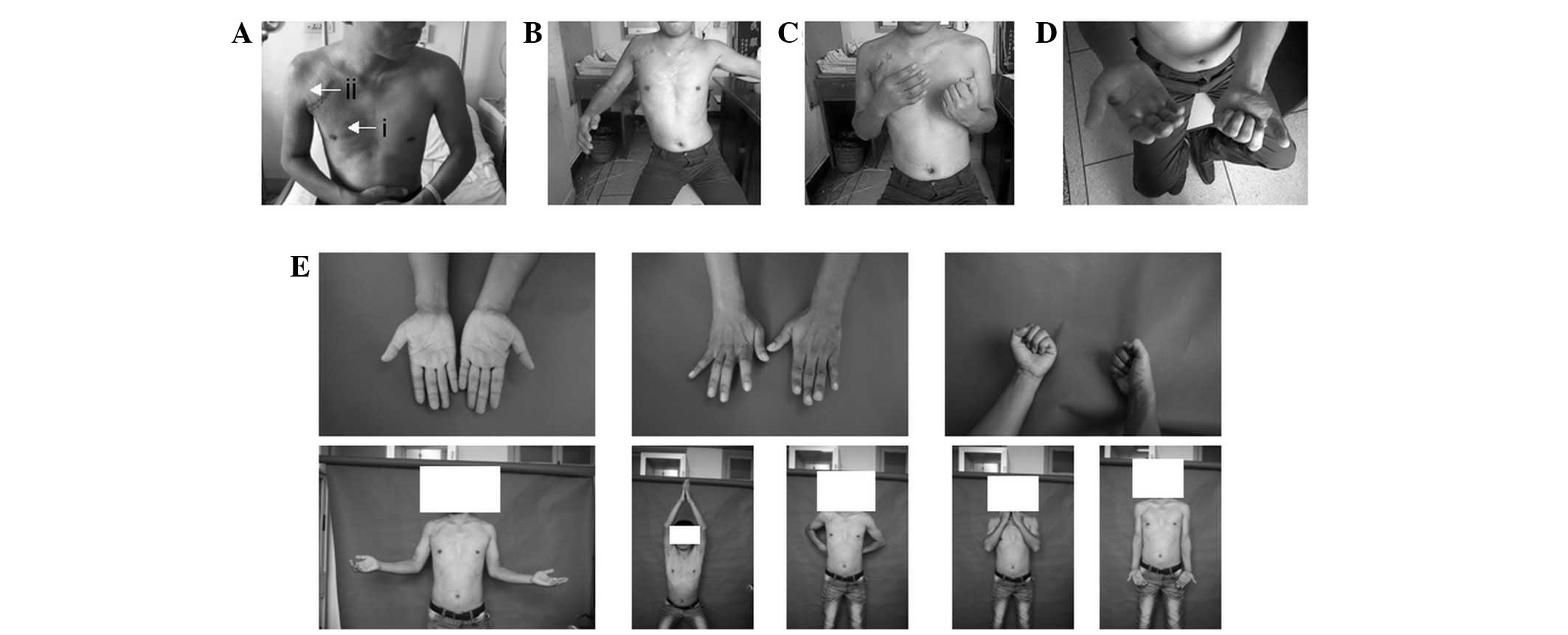
and remove the organized blood clot. At 1 month after the initial
operation, the patient had developed atrophy of the pectoralis
major, pectoralis minor, deltoid and infraspinatus muscles
(Fig. 2A). Right upper limb
function was examined (Fig. 2B–D)
and evaluated using various clinical scales; the Gilbert score
(5) for shoulder joint function
was stage I, the Gilbert and Raimondi score (5) for elbow function was 3 points (Grade
II), the Raimondi score (5) for
hand and wrist function was stage II and the disabilities of the
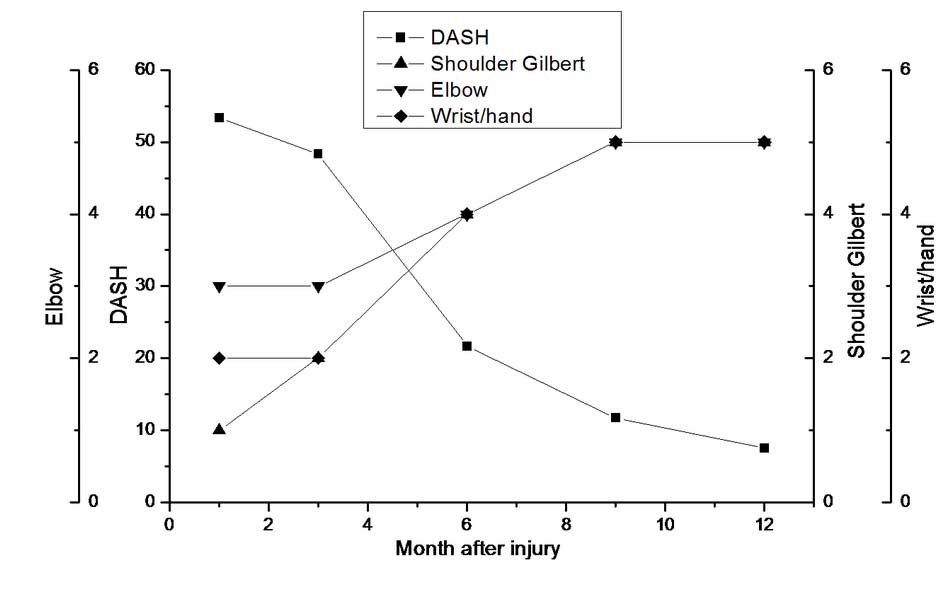
arm, shoulder and hand (DASH) score (6) was 53.33 (Fig. 3). After 3 months of oral
neurotrophic medication, the Gilbert score for shoulder function
had increased to stage II and the DASH score had decreased to
48.33, indicating partial recovery of shoulder function. However,
the elbow, hand and wrist function scores had not improved, and the
region innervated by the ulnar nerve had not recovered.
Electromyography (EMG) showed injury to the right cord of the
brachial plexus, including severe injury to the median, ulnar and
axillary nerves and mild injury to the radial and musculocutaneous
nerves. The second brachial plexus neurolysis was performed at 3.5
months after injury. The right upper limb function was re-evaluated
following the second brachial plexus neurolysis, and the shoulder,
elbow, wrist and hand function and DASH scores are shown in
Fig. 2E and Fig. 3.
 | Figure 3.Shoulder, elbow, wrist and hand
functional scores, and disabilities of the arm, shoulder and hand
(DASH) scores. From 1 to 3 months after injury, elbow and
wrist/hand function remained impaired, the shoulder regained some
function, and the DASH scores were reduced. After the second
neurolysis (3.5 months after injury), the shoulder, elbow and
wrist/hand functional scores increased, and the DASH scores further
decreased. |
The patient was followed up until 13 months
postoperatively. Color B-mode Doppler ultrasonography showed that
the stent at the junction of the right axillary artery and the
subclavian artery had a 5.3–8.7 mm internal diameter, with intimal
thickening of ≤2.7 mm, and slower blood flow than that on the
contralateral side. Part of the right axillary vein was reversed
and used to form a collateral branch. CT angiography (CTA) showed
the stent and the normal size and appearance of the right
subclavian and axillary arteries, with no evidence of stenosis.
These results indicate that the endovascular stent was stable and
remained patent in vivo, and may be used to repair injured
great vessels in the clavicular region. Notably, stent distortion
or deformation due to the large range of motion of the shoulder
joint did not cause stenosis during the follow-up period. However,
the possibility of stenosis resulting from the large range of
motion should be considered when repairing vessels close to the
shoulder joint. All parameters of EMG at 13 months were
significantly improved compared with the results at 3 months. The
right upper limb function was almost restored to normal, with the
exception of hypothenar muscle atrophy, limited interphalangeal
joint extension, limited intrinsic muscle function and numbness of
the fourth and fifth fingers and ulnar palm. The DASH score at 13
months was 7.5, indicating minimal influence on the life and work
of the patient.
Discussion
Since the subclavian artery is protected by the
clavicle and the superficial muscles, the incidence of subclavian
artery injury is extremely low (7). However, rupture of the subclavian
artery causes local hemorrhage and may result in ischemia and
necrosis of the upper limb, brachial plexus injury and even
hemorrhagic shock or mortality. In the present study, the arterial
injury was in the proximal segment of the axillary artery, at the
point where the subclavian artery exits the thoracic cage, and was
repaired using techniques for subclavian artery repair. Subclavian
and proximal axillary artery injuries are usually repaired early to
promptly reconstruct blood flow (1,2,6).
Since the wall of the subclavian artery is very elastic, loosening
of the arterial clamp during vascular anastomosis may lead to the
proximal end of the subclavian artery retracting into the thoracic
cavity, possibly resulting in increased hemorrhage (8). Vascular anastomosis is also more
difficult following hemorrhage, and the incidence rate of
thrombosis and distal vascular embolism is increased (9).
In the present study, we placed the coated
endovascular stent under C-arm fluoroscopy guidance rather than
using a digital subtraction angiography workstation, as it was
simpler and more convenient. Patients with suspected arterial and
venous injury or brachial plexus injury may be treated with
intravascular stent grafting followed by open surgery.
Simultaneously, the veins and the brachial plexus may be examined
to determine the necessity for anastomosis and repair, thus
reducing the concern over further hemorrhage. However, the surgeon
should handle the tissues gently to avoid damaging the implanted
stent. Coated endovascular stent grafting may effectively stop
bleeding and greatly reduce surgical risks (10). Interventional surgeries have
previously been performed under digital subtraction angiography
(DSA) guidance (4), which is
simple and obtains high quality images, but is not appropriate for
patients with severe injuries to the great vessels.
Coated endovascular stent grafts are not recommended
for use in limbs since the large range of motion of the limbs may
cause the stents to distort or deform. In the present case, the
injury was located in the proximal segment of the axillary artery,
where the range of motion is limited. At the 13 month follow-up,
CTA showed no obvious stent displacement or distortion. Coated
endovascular stent grafting is therefore safe for this type of
injury. However, further investigation is required to determine the
safety of using this technique for injuries adjacent to the
shoulder joint.
Intimal thickening, stenosis and embolism are common
complications following endovascular stent placement, and directly
influence postoperative function and prognosis. The coated
endovascular stent has a smoother inner wall than other
endovascular stents, which reduces the incidence of intimal
thickening, stenosis and embolism. The patency of coated
endovascular stents has been reported as 98.2, 89.5 and 84.5% at 1,
2 and 5 years postoperatively (8).
In the present case, a 5-cm endovascular stent was placed and there
was intimal thickening after 6 months which was not increased at 13
months. A study with a larger sample size and a longer follow-up
period should be undertaken to further evaluate the long-term
prognosis of such stents.
Since it is difficult to determine clinically if
brachial plexus injury is a direct result of nerve injury or is
secondary to vessel injury, exploratory surgery is important in
cases of subclavian artery injury, even when there is no severe
limb ischemia.
Following treatment of injury to the great vessels,
upper limb function should be evaluated and brachial plexus injury
should be treated. It is important to determine the necessity and
timing of secondary surgery. Patients with brachial plexus injury
show certain disturbances of upper limb function, which may recover
following treatment. It is generally accepted that there may be
partial spontaneous recovery of nerve function prior to surgery.
Dubuisson and Kline (11) suggest
that a second-look surgery should be performed at 2–4 months after
open brachial plexus injury if there has been no recovery of nerve
function. However, other researchers have different opinions on the
optimal timing of second-look surgery, ranging from 1 to 6 months
(12,13). One previous study observed that a
delay of longer than 5 months may result in poor long-term upper
limb function (14).
Magalon et al (15) stated that exploration should be
performed within 7 days after the injury since exploration is
easier at that time and allows earlier nerve grafting. In the
present case, the hematoma was removed and complete or partial
rupture of the brachial plexus was prevented. Therefore, the timing
of the second surgery depended on the neurological recovery of the
patient. At the 3 month follow-up, the function of the elbow, wrist
and hand had not recovered significantly, and shoulder function had
improved slightly. EMG results indicated the necessity for a second
surgery. The subsequent recovery of upper limb function
demonstrated the effectiveness of the second neurolysis.
C-arm fluoroscopy-guided endovascular stent grafting
shortens treatment time and facilitates treatment for brachial
plexus injury and other complications. Open trauma to the
infraclavicular region is complicated by brachial plexus injury.
Therefore, early exploration to assess nerve continuity, removal of
the surrounding hematoma, active follow-up, regular examination of
stent location and patency, evaluation of brachial plexus function
and optimal timing of the second neurolysis operation may help to
restore upper limb function.
References
|
1.
|
Hernandez JA, Pershad A and Laufer N:
Subclavian artery pseudoaneurysm successful exclusion with a
covered self-expanding stent. J Invasive Cardiol. 14:278–279.
2002.PubMed/NCBI
|
|
2.
|
Pastores SM, Marin ML, Veith FJ, Bakal CW
and Kvetan V: Endovascular stented graft repair of a pseudoaneurysm
of the subclavian artery caused by percutaneous internal jugular
vein cannulation: case report. Am J Crit Care. 4:472–475.
1995.PubMed/NCBI
|
|
3.
|
Sullivan TM, Bacharach JM, Perl J and Gray
B: Endovascular management of unusual aneurysms of the axillary and
subclavian arteries. J Endovasc Surg. 3:389–395. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
du Toit DF, Strauss DC, Blaszczyk M, de
Villiers R and Warren BL: Endovascular treatment of penetrating
thoracic outlet arterial injuries. Eur J Vasc Endovasc Surg.
19:489–495. 2000.PubMed/NCBI
|
|
5.
|
Haerle M and Gilbert A: Management of
complete obstetric brachial plexus lesions. J Pediatr Orthop.
24:194–200. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Hudak PL, Amadio PC and Bombardier C;
Upper Extremity Collaborative Group (UECG): Development of an upper
extremity outcome measure: the DASH (disabilities of the arm,
shoulder and hand) [corrected]. Am J Ind Med. 29:602–608. 1996.
|
|
7.
|
Abouljoud MS, Obeid FN, Horst HM, Sorensen
VJ, Fath JJ and Chung SK: Arterial injuries of the thoracic outlet:
a ten-year experience. Am Surg. 59:590–595. 1993.PubMed/NCBI
|
|
8.
|
Wang KQ, Wang ZG, Yang BZ, et al:
Long-term results of endovascular therapy for proximal subclavian
arterial obstructive lesions. Chin Med J (Engl). 123:45–50.
2010.PubMed/NCBI
|
|
9.
|
Gray BH, Sullivan TM, Childs MB, Young JR
and Olin JW: High incidence of restenosis/reocclusion of stents in
the percutaneous treatment of long-segment superficial femoral
artery disease after suboptimal angioplasty. J Vasc Surg. 25:74–83.
1997. View Article : Google Scholar
|
|
10.
|
Wynn Parry CB: Brachial plexus injuries.
Br J Hosp Med. 32:130–132. 134–139. 1984.
|
|
11.
|
Dubuisson AS and Kline DG: Brachial plexus
injury: A survey of 100 consecutive cases from a single service.
Neurosurgery. 51:673–682. 2002.PubMed/NCBI
|
|
12.
|
Hentz VR and Narakas A: The results of
microneurosurgical reconstruction in complete brachial plexus
palsy. Assessing outcome and predicting results. Orthop Clin North
Am. 19:107–114. 1988.PubMed/NCBI
|
|
13.
|
Kline DG: Surgical repair of peripheral
nerve injury. Muscle Nerve. 13:843–852. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Kandenwein JA, Kretschmer T, Engelhardt M,
Richter HP and Antoniadis G: Surgical interventions for traumatic
lesions of the brachial plexus: a retrospective study of 134 cases.
J Neurosurg. 103:614–621. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
Magalon G, Bordeaux J, Legre R and Aubert
JP: Emergency versus delayed repair of severe brachial plexus
injuries. Clin Orthop Relat Res. 237:32–35. 1988.PubMed/NCBI
|