Introduction
It is essential for clinicians to monitor the
arterial blood pressure (BP) of surgery patients who are under
general anesthesia. BP is a basic vital sign and is one of the most
important hemodynamic indices often utilized to guide therapeutic
interventions, particularly as part of the standard of care for
anesthesia and perioperative management. Acquiring timely and
accurate BP information is critical for monitoring the depth of
anesthesia and for guaranteeing the safety of the patient while
operating under general anesthesia. Inaccurate measurements of BP
may lead to inappropriate interventions.
BP may be measured by either invasive or
non-invasive methods in anesthetized patients. Intra-radial,
intra-femoral and intra-dorsalis pedis artery BP measurements are
the most common invasive methods used. By contrast, oscillometric
BP measurement is the most common non-invasive method used during
surgery. Invasive and non-invasive methods each have their own
advantages and disadvantages. Traditionally, BP measurements taken
via invasive methods are considered the gold standard and most
accurately reflect the BP at any given time (1). However, the placement of an arterial
catheter in patients is often technically challenging, costly and
accompanied by several complications, including trauma, bleeding,
infection, thrombosis, embolism, distal ischemia and the formation
of pseudoaneurysms (2–5). Although non-invasive methods are most
commonly used in routine surgeries due to convenience, non-invasive
BP (NIBP) measurements are less accurate and may be impacted by a
number of factors.
The comparison of BP measurements by invasive and
non-invasive sphygmomanometry has been a topic of study for
decades. Nevertheless, the extent of agreement between invasive and
non-invasive monitoring devices remains unknown. For instance, in
studies that compared NIBP monitoring techniques performed using
the Philips MP90 (Philips Medical Systems, BG Eindhoven, The
Netherlands), Nexfin HD (BMEYE, Amsterdam, The Netherlands) and
Finapres units (Finapres Medical Systems, Amsterdam, The
Netherlands) with those using intra-arterial BP (IABP) monitoring,
inconsistent data were observed (6–9).
However, NIBP data collected using the T-Line Tensymeter (Tensys
Medical, Inc., San Diego, CA, USA), Colin CBM-3000 (Colin
Electronics, Komaki, Japan) and Vasotrac (Medwave, Arden Hills, MN,
USA) instruments displayed good agreement with the intra-radial BP
(10–16). Although marked agreement was
observed between the Vasotrac and intra-radial artery BP, various
studies have identified differing biases affecting the systolic BP
(SBP), diastolic BP (DBP) and mean arterial blood pressure (MAP)
measurements (12–16). Several studies have shown that
these invasive and non-invasive methods produce different values.
The variations are likely to be due to differences between the
devices, the positions and cuff selections for the non-invasive
measurements, the age, weight and surgical status of the patients,
the range of narcotics administered and the varying patient
positions for surgery (17–21).
However, to the best of our knowledge, no studies have specifically
compared non-invasive and invasive BP measurements using the
Philips Intellivue MP50 monitor in surgery patients under general
anesthesia.
Therefore, the present retrospective study included
515 cases where the BP had been monitored using invasive methods at
the intra-radial, femoral or dorsalis pedis arteries and
oscillometric methods using the Philips Intellivue MP50 monitor.
All cases involved surgeries performed under general anesthesia
between January 2009 and April 2011 in Tongji Hospital (Hubei,
China). The aim of the study was to identify the correlation and
agreement between the standard invasive method and the
oscillometric method using the Philips Intellivue MP50 monitor.
Patients and methods
Participants
A retrospective review was performed of patients who
had undergone surgeries in which their BP was monitored by invasive
and non-invasive methods. The patients had been treated at Tongji
Hospital between January 2009 and April 2011. In total, the data of
515 patients were retrieved from files that were kept in the
Department of Anesthesia. The patients were of American Society of
Anesthesiologists (ASA) classification 1 or 2. Patients suffering
from cardiovascular disease, high BP or diabetes were excluded from
the study.
Procedures and outcomes
Measurement of NIBP
Patients were transferred to the operating room in
the supine position, where they were attached to standard monitors,
including an electrocardiography machine, an SpO2
monitor and a sphygmobolometer. Following a 10 min stabilization
period, the NIBP (oscillometric method) from the humerus of the
right arm was measured using the Philips Intellivue MP50
monitor.
Measurement of IABP
All 515 patients were of ASA physical status 1 or 2
and were scheduled to undergo elective surgery at Tongji Hospital.
All surgeries were performed under general anesthesia in the
central operating room area and were prospectively entered into the
present study. Entropy electrodes were applied to the right
forehead of each patient and a Narcotrend monitor (MonitorTechnik,
Bad Bramstedt, Germany) was used to detect whether the depth of
anesthesia became insufficient at any time during the study.
The general anesthesia procedure was as follows:
Tidal volume method inhalation induction (8% sevoflurane oxygen
flow 6 l/min) followed by intravenous injections of femifentanil (1
μg/kg) and rocuronium (0.6 mg/kg). Tracheal intubation was
provided at a train of four (TOF) stimulation value of 0. Fentanyl
(2 μg/kg) was injected 3 min prior to the incision and the
anesthesia was maintained with remifentanil (0.3 μg/kg/min)
and sevoflurane to keep the Narcotrend value between 20 and 46. The
end tidal concentration of sevoflurane was monitored
continuously.
Following the induction of anesthesia, the same
primary team placed a 20-gauge catheter in the radial artery of the
wrist, the femoral artery of the inguinal region or the dorsalis
pedis artery of the instep. The location of the IABP was determined
by the disease and surgical site of the patient. The arterial
catheter was connected to a disposable pressure transducer (Edwards
Life Sciences, Irvine, CA, USA), which was calibrated to the level
of the patient’s heart. The tubing and the transducer were
inspected to ensure that there were no technical issues or air
bubbles that may have caused an erroneous recording. The Philips
Intellivue MP50 monitor was then interfaced with the patient to
allow simultaneous IABP data collection.
Once the hemodynamic changes had stabilized and the
preparations were complete, the invasive and non-invasive BP were
measured simultaneously and recorded every 5 min. To minimise the
errors caused by movement and reference point changes, only
patients who were not moved during surgery were selected for the
study.
Ethics
Approval for the present study was obtained from The
Ethics Committee of Tongji Medical College, Huazhong University of
Science and Technology (China). In accordance with this approval
for a retrospective analysis of patient data, no individual patient
consent was required.
Statistical analysis
The data were analyzed using SPSS software (version
12.0; SPSS, Inc., Chicago, IL, USA). Results are presented as the
mean ± standard deviation. The various invasive BP measurements and
oscillometric methods were examined using correlation, regression
and Bland-Altman analyses (22).
P<0.05 was considered to indicate a statistically significant
difference.
Results
Baseline characteristics and clinical
data
The clinical characteristics of the study population
are summarized in Table I. A total
of 515 patients that were scheduled to undergo elective surgery
were enrolled in the present retrospective study: The intra-radial
group consisted of 165 patients (85 males and 80 females; mean age,
55±16 years; mean weight, 62±12 kg). The intra-femoral group
consisted of 179 patients (96 males and 83 females; mean age, 57±14
years; mean weight, 58±11 kg). A total of 171 patients (86 males
and 85 females; mean age, 42±16 years; mean weight, 59±12 kg)
formed the intra-dorsalis pedis artery group.
 | Table I.Patient characteristics. |
Table I.
Patient characteristics.
| Factors | Location of IABP
monitoring
|
|---|
| Intra-radial
artery | Intra-femoral
artery | Intra-dorsalis pedis
artery |
|---|
| Male | 85 | 96 | 86 |
| Female | 80 | 83 | 85 |
| Age (years) | 55±16 | 57±14 | 42±16 |
| Weight (kg) | 62±12 | 58±11 | 59±12 |
| Head and neck surgery
(n) | - | - | 160 |
| Chest surgery
(n) | 59 | 82 | 6 |
| Abdominal surgery
(n) | 83 | 97 | 5 |
| Pelvic surgery
(n) | 19 | - | - |
| Limb surgery (n) | 4 | - | - |
| Number of
patients | 165 | 179 | 171 |
Comparison between the intra-radial
and oscillometric BP
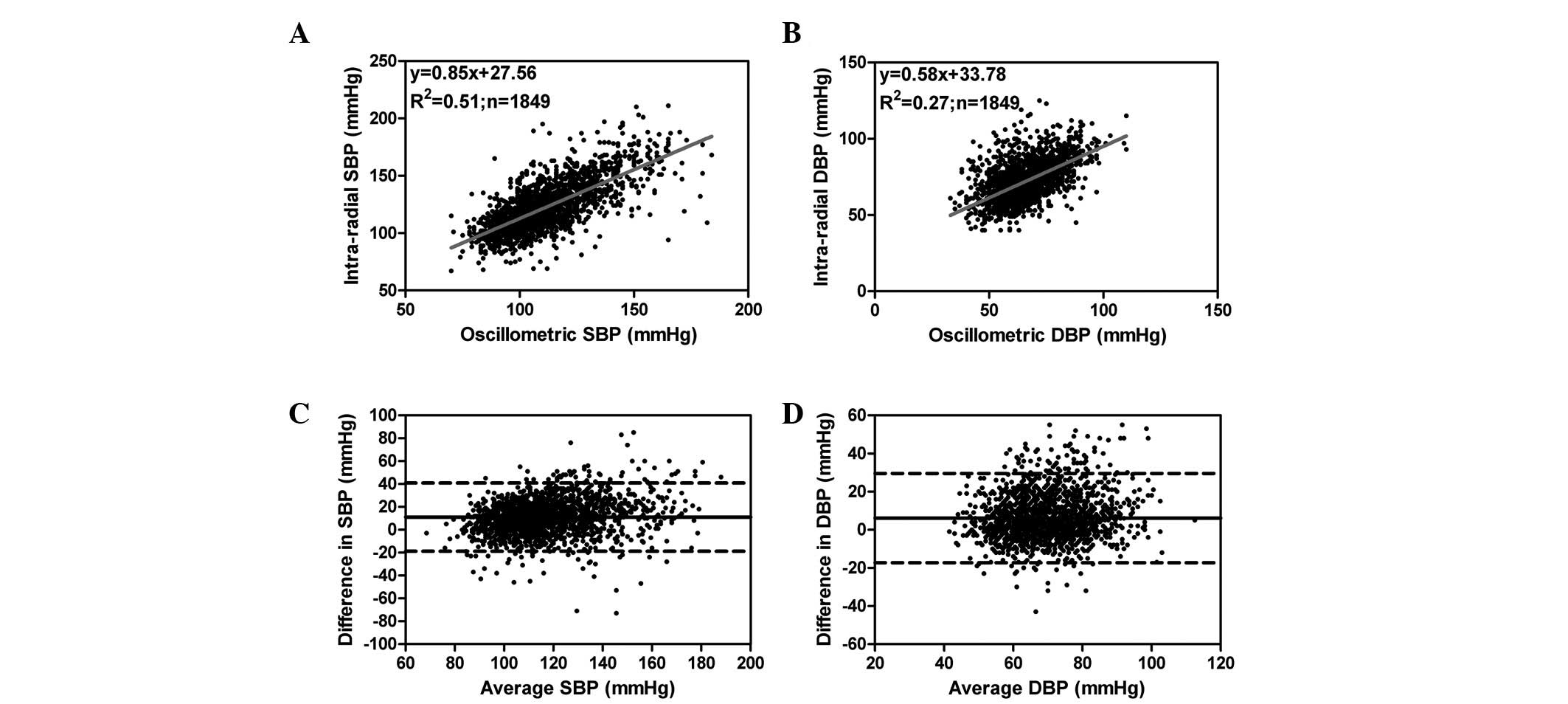
The correlation and the regression and Bland-Altman
analyses of SBP and DBP between the intra-radial and oscillometric
BP measurements are shown in Fig.
1 and Table II. Based on 1,849
measurements from 165 patients, there was a moderate correlation
between the intra-radial and oscillometric measurements for SBP
(r2=0.51, P<0.001) and a limited correlation for DBP
(r2=0.27, P<0.001). The Bland-Altman analysis showed
poor agreement for the SBP (mean bias of 11.04±15.22, with a
precision of 14.76±11.64 mmHg) and DBP (mean bias of 6.17±11.95,
with precision of 9.77±9.25 mmHg), measured using the intra-radial
and oscillometric methods, with limits of agreement ranging from
40.87 to −18.79 mmHg and 29.59 to −17.25 mmHg, respectively.
Between the methods, 38.78% of the SBP values and 38.34% of the DBP
values differed by >10 mmHg.
 | Table II.Bias, limits of agreement and
precision between IABP and NIBP for SBP and DBP. |
Table II.
Bias, limits of agreement and
precision between IABP and NIBP for SBP and DBP.
| Group | Mean bias (mmHg) | Upper/lower limit of
agreement (mmHg) | Precision (mmHg) | Measurements, n |
|---|
| Intra-radial BP | | | | |
| SBP | 11.04±15.22 | 40.87/−18.79 | 14.76±11.64 | 1849 |
| DBP | 6.17±11.95 | 29.59/−17.25 | 9.77±9.25 | 1849 |
| Intra-femoral BP | | | | |
| SBP | 14.79±14.55 | 43.31/−13.73 | 17.15±11.68 | 3413 |
| DBP | 4.12±9.70 | 23.13/−14.89 | 7.49±7.40 | 3413 |
| Intra-dorsalis pedis
BP | | | | |
| SBP | 13.00±16.81 | 45.95/−19.95 | 17.34±12.28 | 5726 |
| DBP | 0.17±11.27 | 22.26/−21.92 | 8.44±7.46 | 5726 |
Comparison between the intra-femoral
and oscillometric BP
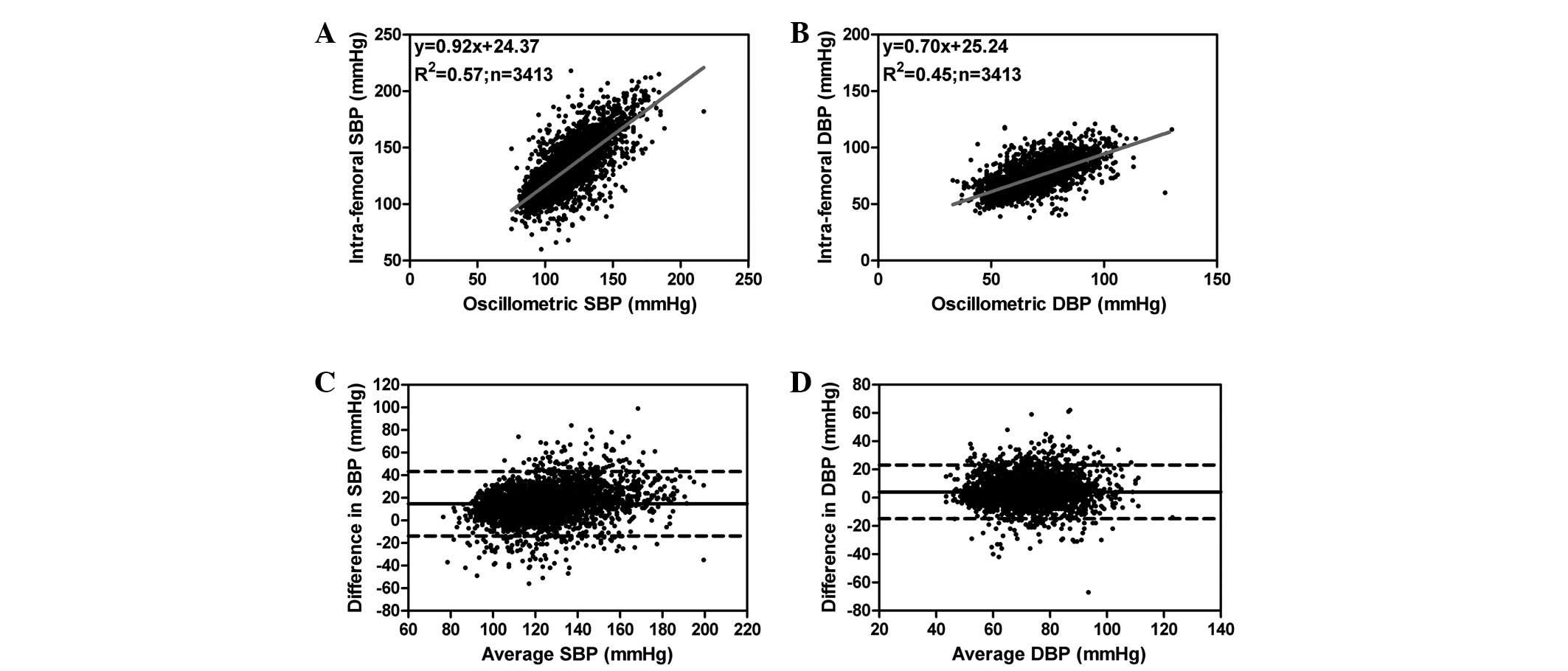
The correlation and the regression and Bland-Altman
analyses of the SBP and DBP between the intra-femoral and
oscillometric BP measurements are shown in Fig. 2 and Table II. Based on 3,413 measurements from
179 patients, there was a moderate correlation between the
intra-femoral and oscillometric measurements for the SBP
(r2=0.57, P<0.001) and a limited correlation for the
DBP (r2=0.45, P<0.001). The Bland-Altman analysis
showed poor agreement for the SBP (mean bias of 14.79±14.55 with
precision of 17.15±11.68 mmHg) and the DBP (mean bias of 4.12±9.70
with precision of 7.49±7.40 mmHg) measured using intra-femoral and
oscillometric methods, with limits of agreement ranging from 43.31
to −13.73 mmHg and 23.13 to −14.89 mmHg, respectively. Between the
methods, 72.25% of the SBP values and 27.92% of the DBP values
differed by >10 mmHg.
Comparison between the intra-dorsalis
pedis and oscillometric blood pressure
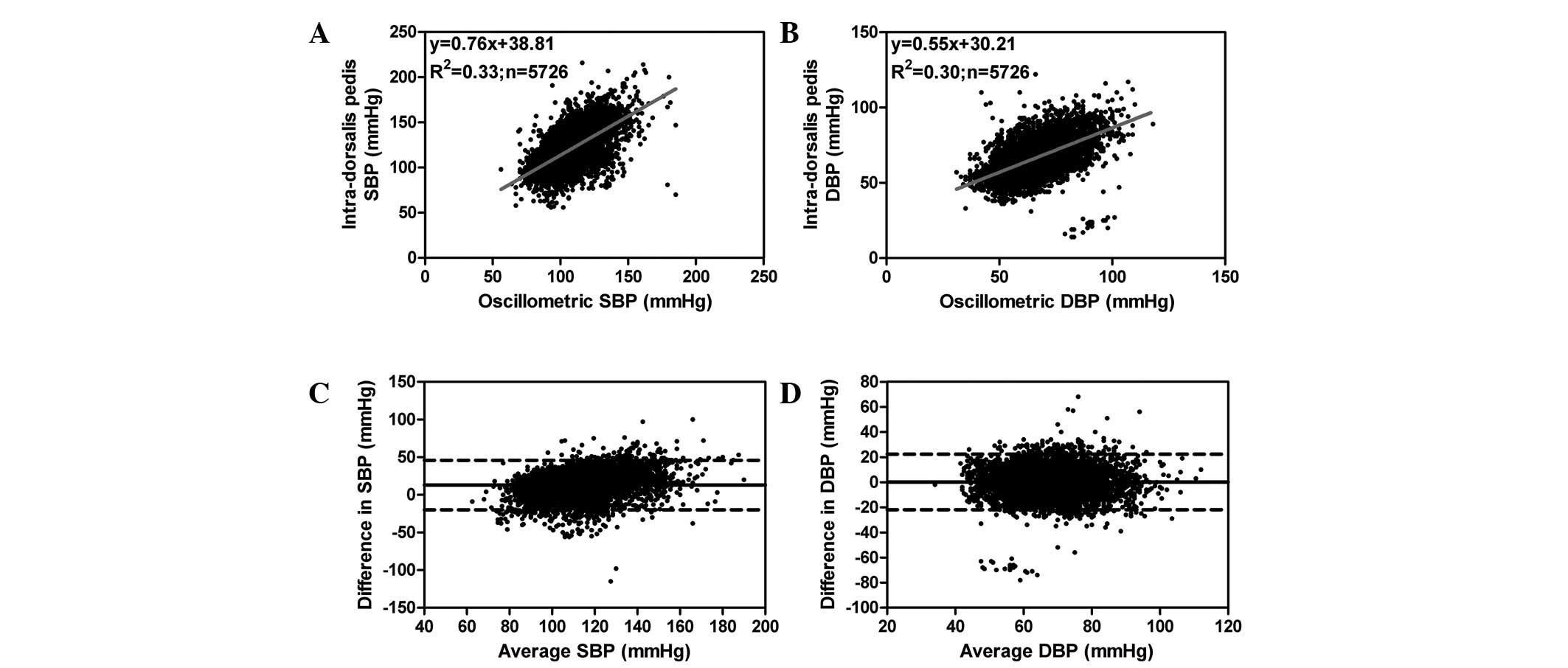
The correlation and the regression and Bland-Altman
analyses of the SBP and DBP are shown in Fig. 3 and Table II. Based on 5,726 measurements from
171 patients, there were limited correlations between the
intra-dorsalis pedis and oscillometric measurements for SBP
(r2=0.33, P<0.001) and DBP (r2=0.30,
P<0.001). The Bland-Altman analysis showed poor agreement for
SBP (mean bias of 13.00±16.81, with precision of 17.34±12.28 mmHg)
and DBP (mean bias of 0.17±11.27, with precision of 8.44±7.46 mmHg)
measured using intra-dorsalis pedis and oscillometric methods, with
limits of agreement ranging from 45.95 to −19.95 mmHg and 22.26 to
−21.92 mmHg, respectively. Between the methods, 69.44% of the SBP
values and 34.46% of the DBP values differed by >10 mmHg.
Discussion
The accurate measurement of BP is essential for the
rational hemodynamic management of surgery patients. However, it is
unclear whether invasive and non-invasive BP measurements may be
used interchangeably. The data from the present study revealed that
the non-invasive method using the Philips Intellivue MP50 monitor
was not an appropriate substitute for standard invasive BP
measurement techniques, including those for intra-radial,
intra-femoral and intra-dorsalis pedis artery blood pressure, thus
supporting the use of direct intra-arterial methods for monitoring
BP and guiding treatment decisions due to the accuracy of the
invasive methods.
BP is the pressure exerted by circulating blood upon
the walls of the blood vessels (23). Invasive and non-invasive techniques
reflect the effects of all fluids. However, the two techniques have
intrinsic differences as they involve the measurement of different
quantities. For example, in the invasive technique, the sum of the
lateral pressure (measured by the non-invasive BP) and the
converted kinetic energy are recorded. Accordingly, the invasive
and non-invasive methods of measurement are different (24,25).
Moreover, differences between non-invasive and invasive BP
measurements have been documented in various clinical situations
(6–21).
The Philips Intellivue MP50 monitor provides a
non-invasive, near-continuous method for monitoring BP, and is
designed to be an alternative to direct IABP measurement. By
compressing the artery with a cuff and then slowly releasing the
pressure, pulsations from the artery are transmitted as
oscillations to the cuff and the SBP and DBP values are recorded.
In the Tongji hospital, the Philips Intellivue MP50 monitor is used
to monitor the NIBP and IABP of surgery patients in the operating
room. However, there is little information with regard to the
correlation and agreement between the NIBP measured by the Philips
Intellivue MP50 and the IABP in surgery patients under general
anesthesia.
In the present study, measurements from various IABP
locations (intra-radial, intra-femoral and intra-dorsalis pedis
arteries) were compared with measurements obtained by the
oscillometric method from the humerus of the right arm of surgery
patients under anesthesia in the supine position. It was identified
that there were clinically low positive correlations and poor
agreement between the direct BP measurements, including the
intra-radial, intra-femoral and intra-dorsalis pedis BP
measurements, and the oscillometric BP for the SBP and DBP measured
by the Philips Intellivue MP50. The data demonstrated that the mean
bias and precision of the DBP between the intra-femoral BP and the
NIBP were within the minimum performance standards set by the
Association for the Advancement of Medical Instrumentation (AAMI),
which recommended that non-invasive BP devices should be accurate
within 5 mmHg and have a precision within 8 mmHg. However, the
results also demonstrated that between all methods, >10% of the
arterial BP values of the SBP and DBP differed by >10 mmHg,
which was not in agreement with the standards proposed by the AAMI
(26). In addition, the process of
making clinical and therapeutic decisions was weakened by the
calculated standard deviations of ±15.22, ±11.95, ±14.55, ±9.70,
±16.81 and ±11.27 mmHg, which were determined for the oscillometric
method.
A possible explanation for the observed differences
between the two systems may be that since the oscillometric method
is not standardized, algorithm measurements may differ between
manufacturers and even between devices. Belani et al
(12), observed a good correlation
and agreement between the IABP measurements and the Vasotrac (a
device that uses frequent gentle compression and decompression of
the radial artery at the wrist and displays the arterial pressure
wave approximately every 12 to 15 heart beats) in a study of 80
critically ill surgical patients positioned in the supine position.
The study demonstrated a bias and precision of 0.0±5.4 and 3.9±3.7
mmHg, respectively, for the SBP and −0.4±3.9 and 2.7±2.8 mmHg,
respectively, for the DBP. Moreover, in another study by Belani
(13), the differences between the
measurements did not exceed 10 mmHg for >90% of the paired
values. McCann et al (15)
reached the same conclusion by comparing the radial artery BP
determined by the Vasotrac device and IABP monitoring in
adolescents undergoing scoliosis surgery. Janelle and Gravenstein
(10) identified a good agreement
between the T-Line Tensymeter (continuous non-invasive blood
pressure management device) BP and IABP measurements in surgery
patients, with a bias and precision of 1.7±7.0 and 5.7±4.4 mmHg,
respectively, for the SBP, 2.3±6.9 and 5.7±4.5 mmHg, respectively,
for the DBP and 1.7±5.3 and 4.0±4.8 mmHg, respectively, for the
mean BP.
Another explanation for the observed difference may
be due to the anesthesia. Lakhal et al (27) reported that the IABP and arm
oscillometric non-invasive MAP readings of patients without general
anesthesia were significantly and positively correlated
(r2=0.85; P<0.001) and that the agreement between
these two methods was acceptable (mean bias, 3.4±5.0 mmHg;
lower/upper limit of agreement, −6.3/13.1 mmHg). In addition to
this, Lee et al (18)
observed that the values of arterial BP measurements were as high
as those measured by non-invasive methods under general anesthesia
using sevoflurane. This is in contrast to the results from the
present study. However, Lee et al did not perform a
correlation and agreement analysis between the IABP and NIBP.
Certain limitations of the present study require
discussion. Firstly, the NIBP of the 515 patients was recorded from
the humerus of the right arm. There are no comparisons between the
NIBP or the IABP of the thigh or ankle. One reason for this is that
in the majority of hospitals, the NIBP of patients was recorded
from the arm due to its practicality and simplicity. Recordings
were taken from the thigh or ankle in only a few patients for
specific reasons, e.g., due to arm diseases. Another reason is that
the NIBP of the arm, measured oscillometrically, has a relatively
good agreement with the IABP, whereas the NIBP for the thigh and
ankle using the invasive reference shows less agreement (27). Thus, in the present study comparing
NIBP with IABP, the NIBP measurements were obtained from the arm
rather than the thigh or ankle. Secondly, the focus of the study
was on the SBP and DBP, rather than on analyzing the accuracy of
oscillometric blood pressure measurements of the MAP. The SBP and
DBP are values that are directly measured by the Philips Intellivue
MP50 monitor system. By contrast, the MAP is deduced from the SBP
and DBP. Therefore, the SBP and DBP values were used as direct
measurements of BP values, rather than the calculated value of the
MAP.
Although widely used, the oscillometric method of
measuring blood pressure used by the Philips Intellivue MP50
monitor was inaccurate in this subset of surgery patients under
general anesthesia, and the parameters obtained should be used
cautiously. Therefore, the results from the present study suggest
that the use of the oscillometric method monitoring system in
surgery patients under general anesthesia should not be generally
recommended. Whether such a tool may be reliable in certain other
patients remains to be determined.
Acknowledgements
This study was supported by the
National Natural Science Foundations of China (no. 30901404).
References
|
1.
|
Bigatello LM and George E: Hemodynamic
monitoring. Minerva Anestesiol. 68:219–225. 2002.
|
|
2.
|
Bowdle TA: Complications of invasive
monitoring. Anesthesiol Clin North America. 20:571–588. 2002.
View Article : Google Scholar
|
|
3.
|
Scheer B, Perel A and Pfeiffer UJ:
Clinical review: complications and risk factors of peripheral
arterial catheters used for haemo-dynamic monitoring in anaesthesia
and intensive care medicine. Crit Care. 6:199–204. 2002. View Article : Google Scholar
|
|
4.
|
Frezza EE and Mezghebe H: Indications and
complications of arterial catheter use in surgical or medical
intensive care units: analysis of 4932 patients. Am Surg.
64:127–131. 1998.PubMed/NCBI
|
|
5.
|
Wilkins RG: Radial artery cannulation and
ischaemic damage: a review. Anaesthesia. 40:896–899. 1985.
View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Mireles SA, Jaffe RA, Drover DR and
Brock-Utne JG: A poor correlation exists between oscillometric and
radial arterial blood pressure as measured by the Philips MP90
monitor. J Clin Monit Comput. 23:169–174. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Stover JF, Stocker R, Lenherr R, Neff TA,
Cottini SR, Zoller B and Béchir M: Noninvasive cardiac output and
blood pressure monitoring cannot replace an invasive monitoring
system in critically ill patients. BMC Anesthesiol. 9:62009.
View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Kermode JL, Davis NJ and Thompson WR:
Comparison of the Finapres blood pressure monitor with
intra-arterial manometry during induction of anaesthesia. Anaesth
Intensive Care. 17:470–475. 1989.PubMed/NCBI
|
|
9.
|
Gibbs NM, Larach DR and Derr JA: The
accuracy of Finapres noninvasive mean arterial pressure
measurements in anesthetized patients. Anesthesiology. 74:647–652.
1991. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Janelle GM and Gravenstein N: An accuracy
evaluation of the T-Line Tensymeter (continuous noninvasive blood
pressure management device) versus conventional invasive radial
artery monitoring in surgical patients. Anesth Analg. 102:484–490.
2006. View Article : Google Scholar
|
|
11.
|
Kemmotsu O, Ueda M, Otsuka H, et al: Blood
pressure measurement by arterial tonometry in controlled
hypotension. Anesth Analg. 73:54–58. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Belani K, Ozaki M, Hynson J, et al: A new
noninvasive method to measure blood pressure: results of a
multicenter trial. Anesthesiology. 91:686–692. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Belani KG, Buckley JJ and Poliac MO:
Accuracy of radial artery blood pressure determination with the
Vasotrac. Can J Anaesth. 46:488–496. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Cua CL, Thomas K, Zurakowski D and Laussen
PC: A comparison of the Vasotrac with invasive arterial blood
pressure monitoring in children after pediatric cardiac surgery.
Anesth Analg. 100:1289–1294. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
McCann ME, Hill D, Thomas KC, Zurakowski D
and Laussen PC: A comparison of radial artery blood pressure
determination between the Vasotrac device and invasive arterial
blood pressure monitoring in adolescents undergoing scoliosis
surgery. Anesth Analg. 101:978–985. 2005. View Article : Google Scholar
|
|
16.
|
Jagomägi K, Raamat R, Talts J, Ragun U and
Tähepõld P: Measurement of mean arterial pressure: comparison of
the Vasotrac monitor with the finger differential oscillometric
device. Physiol Res. 59:691–696. 2010.PubMed/NCBI
|
|
17.
|
Bruner JM, Krenis LJ, Kunsman JM and
Sherman AP: Comparison of direct and indirect methods of measuring
arterial blood pressure, part III. Med Instrum. 15:182–188.
1981.
|
|
18.
|
Lee JH, Kim JM, Ahn KR, et al: Study for
the discrepancy of arterial blood pressure in accordance with
method, age, body part of measurement during general anesthesia
using sevoflurane. Korean J Anesthesiol. 60:323–328. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Araghi A, Bander JJ and Guzman JA:
Arterial blood pressure monitoring in overweight critically ill
patients: invasive or noninvasive? Crit Care. 10:R642006.
View Article : Google Scholar : PubMed/NCBI
|
|
20.
|
Clark JA, Lieh-Lai MW, Sarnaik A and
Mattoo TK: Discrepancies between direct and indirect blood pressure
measurements using various recommendations for arm cuff selection.
Pediatrics. 110:920–923. 2002. View Article : Google Scholar
|
|
21.
|
Bur A, Herkner H, Vlcek M, et al: Factors
influencing the accuracy of oscillometric blood pressure
measurement in critically ill patients. Crit Care Med. 31:793–799.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
22.
|
Bland JM and Altman DG: Statistical
methods for assessing agreement between two methods of clinical
measurement. Lancet. 1:307–310. 1986. View Article : Google Scholar
|
|
23.
|
Williams B, Poulter NR, Brown MJ, et al:
British Hypertension Society: Guidelines for management of
hypertension: report of the fourth working party of the British
Hypertension Society, 2004-BHS IV. J Hum Hypertens. 18:139–185.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
24.
|
No authors listed. 1999 World Health
Organization-International Society of Hypertension Guidelines for
the Management of Hypertension. Guidelines Subcommittee. J
Hypertens. 17:151–183. 1999.
|
|
25.
|
Nichols WW and O’Rourke MF: General
principles for measuring arterial waves. McDonald’s Blood Flow in
Arteries: Theoretical, Experimental and Clinical Principles.
Nichols WW: Oxford University Press; New York: pp. 129–164.
1998
|
|
26.
|
American National Standard: Manual,
electronic or automated sphygmomanometers ANSI/AAMI sp 10-1992.
Association for the Advancement of Medical Instrumentation;
Arlington, VA: 1992
|
|
27.
|
Lakhal K, Macq C, Ehrmann S, Boulain T and
Capdevila X: Noninvasive monitoring of blood pressure in the
critically ill: reliability according to the cuff site (arm, thigh,
or ankle). Crit Care Med. 40:1207–1213. 2012. View Article : Google Scholar : PubMed/NCBI
|