Introduction
Inflammatory disease of the liver, i.e., hepatitis,
represents a major problem in clinical medicine. Although hepatitis
comprises a heterogeneous group of diseases with different
etiologies and complex pathogeneses, previous studies have
indicated that the immune system plays a pivotal role in the
majority of these processes (1).
Neurogenic inflammation encompasses a series of
inflammatory responses triggered by the activation of primary
sensory neurons and the subsequent release of inflammatory
neuropeptides (2). The nervous and
immune systems have been shown to interact to modulate the immune
response via the secretion of neuropeptides. The neuropeptide
substance P (SP) is an 11 amino acid peptide encoded by the
preprotachykinin-A (PPT-A) gene, which is distributed throughout
the nervous systems of humans and animals (3). SP is a member of the tachykinin
family of neuropeptides, which interact with three natural
tachykinin (neurokinin) receptors: NK-1R, NK-2R and NK-3R (4); however, its effects are mainly
mediated through NK-1R, a G protein-coupled receptor (GPCR) that is
expressed in a number of tissues, including the nervous system,
gastrointestinal tract and cells of the immune system. A previous
study demonstrated that SP is a potent pro-inflammatory mediator
that plays an important role in inflammation and viral infections
(5).
SP has been shown to exert a vast range of
pro-inflammatory effects in vitro and in vivo,
affecting a number of immune and inflammatory disorders of the
respiratory, gastrointestinal and musculoskeletal systems. Although
SP is a peptide of neuronal origin, it is also located in
non-neural cells, including endothelial cells, macrophages,
granulocytes, lymphocytes and dendritic cells. SP stimulates immune
cells to produce inflammatory cytokines, including interleukin
(IL)-1, IL-6, tumor necrosis factor (TNF), interferon (IFN)-γ and
the macrophage inflammatory protein 1β. SP induces chemotaxis and
degranulation of neutrophils and also stimulates respiratory burst
(6).
Therefore, it is clear that extensive neuro-immune
inter-system crosstalk is necessary between SP and the inflammatory
response to injury. A previous study demonstrated that primary
afferent sensory neurons are necessary for disease activity in T
cell-mediated immune hepatitis in mice (7). Bang et al first demonstrated
the presence of NK-1R in mouse liver, in which it appeared
predominantly in nonparenchymal mononuclear cells; however, it was
also detected in hepatocytes. The authors reported that NK-1R was
mainly expressed in Kupffer cells (KCs), which corresponds to the
cell population that is primarily activated by lipopolysaccharide
(LPS) in the liver (8). However,
in their study, SP was not investigated and experiments were not
conducted in vitro. Therefore, more data are required
regarding the role of SP in the liver under physiological and
pathophysiological conditions. In the present study, we
investigated the effect of SP in a concanavalin A (ConA)-induced
model of hepatitis. We also cultured mouse KCs to examine the
functional consequences of exposure to SP and to determine whether
treatment with SP leads to pro-inflammatory signaling activities,
including the production of cytokines.
Materials and methods
Drugs and materials
ConA, L-703,606, SP, collagenase IV and Triton X-100
were purchased from Sigma (St, Louis, MO, USA). Percoll, RPMI-1640
medium and fetal bovine serum (FBS) were purchased from Gibco
(Carlsbad, CA, USA). The NK-1R antibody NB300-101 and rabbit
anti-NK-1R secondary antibody were purchased from Novus Biologicals
(Littleton, CO, USA). IL-6 and TNF-α enzyme-linked immunosorbent
assay (ELISA) kits were purchased from R&D Systems
(Minneapolis, MN, USA). The other commercial chemicals used in the
experiments were of analytical grade.
Animal experiments and drug
treatment
Male Swiss albino mice (25–30 g) were purchased from
the Experimental Animal Center of Shandong University School of
Medicine, Shandong, China. The animals were housed six per cage
under standardized conditions (25±3°C, 12 h light/dark cycle and
50±10% humidity) with free access to pelleted food and tap water.
All experiments were conducted with approval from the Institutional
Experimental Animal Care and Use Committee of Shandong
University.
After acclimation for 6–7 days, the animals were
randomly divided into three groups, each containing 12 mice, as
follows: the control group, the ConA model group and the NK-1R
antagonist group (L-703,606-pretreated group). Liver injury was
induced as previously described (9). ConA was dissolved in pyrogen-free
phosphate-buffered saline (PBS) and intravenously injected (25
mg/kg) into the mice of the ConA model group via the tail vein. The
mice in the control group were injected with saline. The mice in
the NK-1R antagonist group were treated with the NK-1R antagonist
L-703,606 at dose of 10 mg/kg prior to the ConA challenge.
L-703,606 was dissolved in 0.9% saline and injected via the tail
vein through a 27 gauge needle. Within each experiment, all drugs
and doses were administered in a counterbalanced manner. Six hours
later, all mice were anesthetized to enable blood to be obtained
from the eye sockets and were then sacrificed prior to dissection
of the liver.
Measurement of SP levels
The liver samples were thawed, weighed and
homogenized at a ratio of 1:9 (w/v) in a 0.9% saline solution. The
homogenate was then centrifuged at 1,600 × g for 10 min at 4°C. The
levels of SP in the supernatant were measured using a mouse SP
ELISA kit according to the manufacturer’s instructions. A 96-well
microplate was loaded with 25 μl primary antibody specific
for rat SP. Aliquots of 50 μl each sample and 50 μl
standard SP dilutions (as a control) were mixed in the assigned
wells in duplicate, followed by the addition of biotinylated SP to
each well, with the exception of the blank control. The plate was
incubated for 2 h at room temperature and then washed six times
with the wash buffer provided in the kit. Subsequently, 100
μl biotinylated anti-SP antibody solution was added and the
plate was incubated for 1 h and then washed four times. Then, 100
μl streptavidinhorseradish peroxidase conjugate solution was
added to each well, with the exception of the chromogen blank, and
the plates were incubated for 1 h and washed again. After washing,
100 μl substrate solution provided in the kit was added to
each well and the plates were incubated for 1 h at room
temperature. The reaction was stopped with 2 mol/l HCl and the
optical density values were read at 492 nm. The concentration of SP
was expressed in pg/ml.
Measuring serum liver enzymes
Blood was collected in ethylenediaminetetraacetic
acid (EDTA) tubes. Following centrifugation of whole blood (1,600 ×
g for 10 min at room temperature), the serum was stored at −70°C
until analysis. The activities of alanine aminotransferase (ALT, a
specific marker for hepatic parenchymal injury) and aspartate
aminotransferase (AST, a nonspecific marker for hepatic injury) in
the serum were determined in units per liter using standard
auto-analyzer methods on an Hitachi Automatic Analyzer (Hitachi
Inc., Tokyo, Japan).
Histological examination
The livers were removed, fixed with 4%
phosphate-buffered paraformaldehyde and embedded in paraffin.
Tissue sections (4 μm) were prepared and stained with
hematoxylin/eosin and the sections were then examined under a light
microscope. In each section, three randomly selected areas were
screened for edema, granulocytes and hepatocyte apoptosis and
necrosis. Histological examination was performed without knowledge
of the treatment administered. The sections were examined by two
independent investigators in a blind manner.
Isolation and culture of KCs
KCs from mice were isolated by collagenase digestion
and differential centrifugation using Percoll density gradients as
described previously (10). Livers
were perfused in vitro through the vena cava with 80 ml
Ca2+/Mg2+-free Hank’s balanced salt solution
(HBSS) at 37°C and transferred to a 100-mm culture dish. Perfusion
was continued with complete HBSS containing 0.05% collagenase IV
and 3 mmol/l Ca2+ at 37°C. The liver tissue was finely
diced into 2-mm3-sized pieces and the suspension was
incubated under constant agitation at 37°C for 30 min. The liver
homogenate was filtered through a gauze mesh and the cell
suspension was centrifuged at 50 × g for 3 min at 4°C to remove the
hepatocytes. The non-parenchymal cell-enriched supernatant was
centrifuged at 400 × g for 6 min. The cell pellet was resuspended
in 30% Percoll with a density of 1.040 g/ml and this suspension was
carefully layered onto 60% Percoll with a density of 1.075 g/ml.
The double-layer discontinuous gradient formed was overlaid with 3
ml HBSS and centrifuged at 400 × g for 15 min at 4°C. The opaque
interface was collected, resuspended in HBSS and centrifuged at 400
× g for 5 min at 4°C. The cells were seeded onto tissue culture
plates at a density of 2×106 cells/ml and cultured in
RPMI-1640 medium containing 10% heat-inactivated FBS, 100 U/ml
penicillin/streptomycin and 10 mmol/l HEPES at 37°C with 5%
CO2. All adherent cells phagocytosed latex beads and
stained positive for catalase, confirming that they were KCs. The
cells were cultured for 24 h prior to the experiment.
NK-1R immunofluorescence
Cells (5×104) were placed on
poly-L-lysine-coated slides in 200 μl media, fixed with 4%
paraformaldehyde, washed three times in 0.1 M PBS, blocked with
serum-free protein and permeabilized using 0.4% Triton X-100. The
fixed cells were incubated overnight at 4°C with the NK-1R antibody
NB300-101 (1:50), then subjected to PBS washes and incubation with
rabbit anti-NK-1R secondary antibody (1:500) for 1 h at room
temperature. Then, the sections were washed in PBS and mounted with
4′,6-diamidino-2-phenylindole (DAPI)-containing mounting medium
(Vector Laboratories, Burlingame, CA, USA). Images were acquired by
laser scanning confocal microscopy (LSM710; Carl Zeiss, Oberkochen,
Germany) and analyzed using Image Pro Plus 6.0 (Media Cybernetics
Rockville, MD, USA).
Quantitative polymerase chain reaction
(PCR)
Total RNA was extracted from KCs using Tri-Reagent
(Molecular Research Center Inc., Cincinnati, OH, USA) and the RNA
was quantitated and reverse-transcribed using the AffinityScript
qPCR cDNA Synthesis kit (Stratagene, Cedar Creek, TX, USA)
according to the manufacturer’s instructions. Total NK-1R mRNA was
quantified as described previously (11) using a primer set specific for a
109-bp fragment of the NK-1R transcripts (sense:
5′-GCATACACCGTAGTGGGAATC-3′; antisense:
5′-CATCATTTTGACCACCTTGC-3′). Glyceraldehyde 3-phosphate
dehydrogenase (GAPDH) was amplified as a control (sense:
5′-GGTGGTCTCCTCTGACTTCAACA-3′; antisense:
5′-GTTGCTGTAGCCAAATTCGTTGT-3′). Reverse transcription (RT)-PCR was
conducted with cycling conditions consisting of 15 min Taq
activation at 95°C followed by denaturing, annealing and extension
phases for 15 sec at 94°C, 30 sec at 54°C and 30 sec at 72°C,
respectively, for 40 cycles. The results for NK-1R are expressed as
the ratio to GAPDH.
Measurement of cytokine release
Micromolar concentrations of SP are typically used
during in vitro studies to identify the biological effects
on immune cells, particularly monocytes (12). KCs were seeded into 24-well plates
at a density of 1×106 cells/well and incubated with
fresh Dulbecco’s modified Eagle’s medium (DMEM) containing 1
μg/ml LPS at 37°C with 5% CO2. The KCs were
cultured with and without SP or with a combination of SP and
L-703,606 with fresh Dulbecco’s modified Eagle’s medium (DMEM)
containing 1 μg/ml LPS at 37°C with 5% CO2 and
challenged with SP (10−6 M) for 24 h. A dose of 1
μM (10−6 M) SP and a stimulation time of 24 h
were selected to ensure maximal cytokine release, as observed in a
previous study (13). At this
concentration, SP is reported to stimulate significant chemokine
production by pancreatic acinar cells and prime neutrophils
triggered by different stimuli to evoke various cellular responses,
including intracellular calcium changes, oxidative responses and
the formation of hydrogen peroxide and nitric oxide (14,15).
In some experiments, the cells were pretreated with L-703,606 (1
μM) for 15 min before SP stimulation, as previously
described (16). The medium from
the cultured KCs was collected and centrifuged at 1,000 × g for 5
min and the supernatant was stored at −70°C until the assays. The
IL-6 and TNF-α levels in the supernatant were determined using
mouse-specific ELISA kits. All samples, including the standard and
control solutions, were assayed in duplicate. The measurements were
performed according to the manufacturer’s instructions. No
cross-reactivity was observed with any other known cytokine. The
results are expressed in picograms per milliliter.
Statistical analysis
All data are presented as mean ± standard error of
the mean (SEM). Differences among the groups were assessed using
unpaired Student’s t-tests and one-way analysis of variance.
P<0.05 was considered to indicate a statistically significant
difference. The calculations were performed with the SPSS, version
11.0, statistical software package (SPSS, Inc., Chicago, IL,
USA).
Results
Detection of SP and liver function
As shown in Table
I, the levels of SP were significantly increased in the
ConA-treated group compared with the control group. Serum
biochemical marker determinations revealed that serum ALT and AST
levels were significantly increased in the ConA-treated group
compared with those in the control group. However, the levels of
serum ALT and AST were significantly decreased in the
L-703,606-pretreated group compared with those in the ConA-treated
group.
 | Table I.Levels of SP and enzymatic markers of
liver function in the different groups. |
Table I.
Levels of SP and enzymatic markers of
liver function in the different groups.
| Groups | ALT (U/l) | AST (U/l) | SP (pg/ml) |
|---|
| Control group | 42.05±8.31 | 51.12±9.16 | 138.52±13.23 |
| ConA model group | 782.37±21.51a | 1004.25±18.24a | 387.23±29.36a |
| L-703,606-pretreated
group | 402.22±16.42b | 581.45±17.51b | |
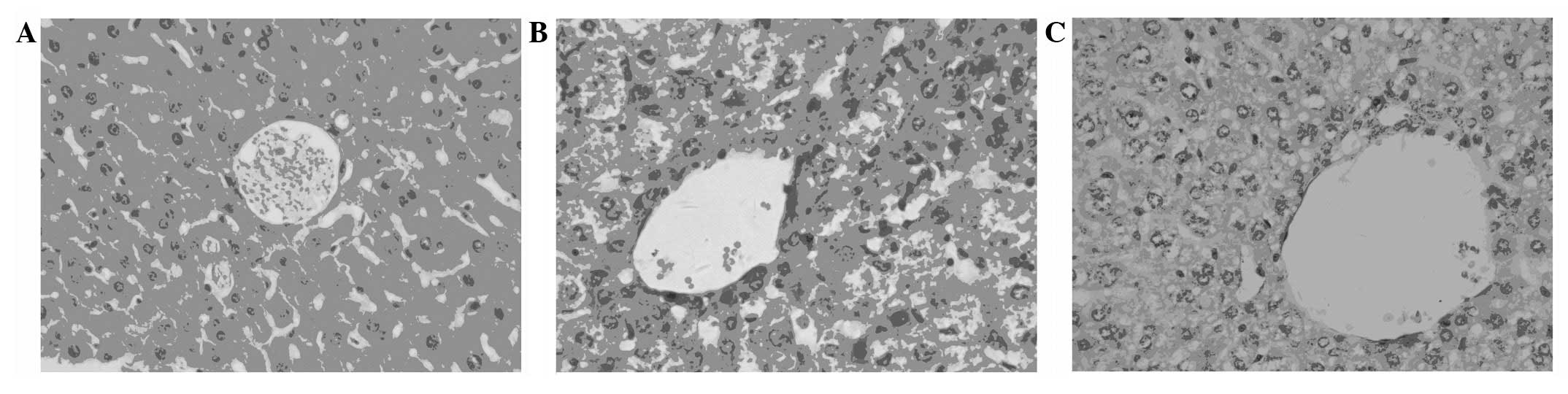
Histopathological changes
A model of hepatic immune injury in mice was
successfully established in this study. Our histological
observations revealed that edema, hepatocellular apoptosis and
granulocyte infiltration were present in the livers of the ConA
model group. Compared with those of the control group (Fig. 1A), the liver tissues from the mice
in the ConA-treated group exhibited significant cytoplasmic
vacuolization, sinusoidal congestion, extensive hepatic cellular
necrosis and massive cellular infiltration (Fig. 1B). However, the parenchymal
appearance was essentially normal in the L-703,606 -pretreated
group. Mild cellular infiltration, necrosis and a comparatively
preserved lobular architecture were observed in the livers of mice
treated with L-703,606 (Fig. 1C).
The NK-1R antagonist L-703,606 was shown to significantly alleviate
ConA-induced liver injury. These results suggest a therapeutic
significance of L-703,606 for protection from ConA-induced liver
injury.
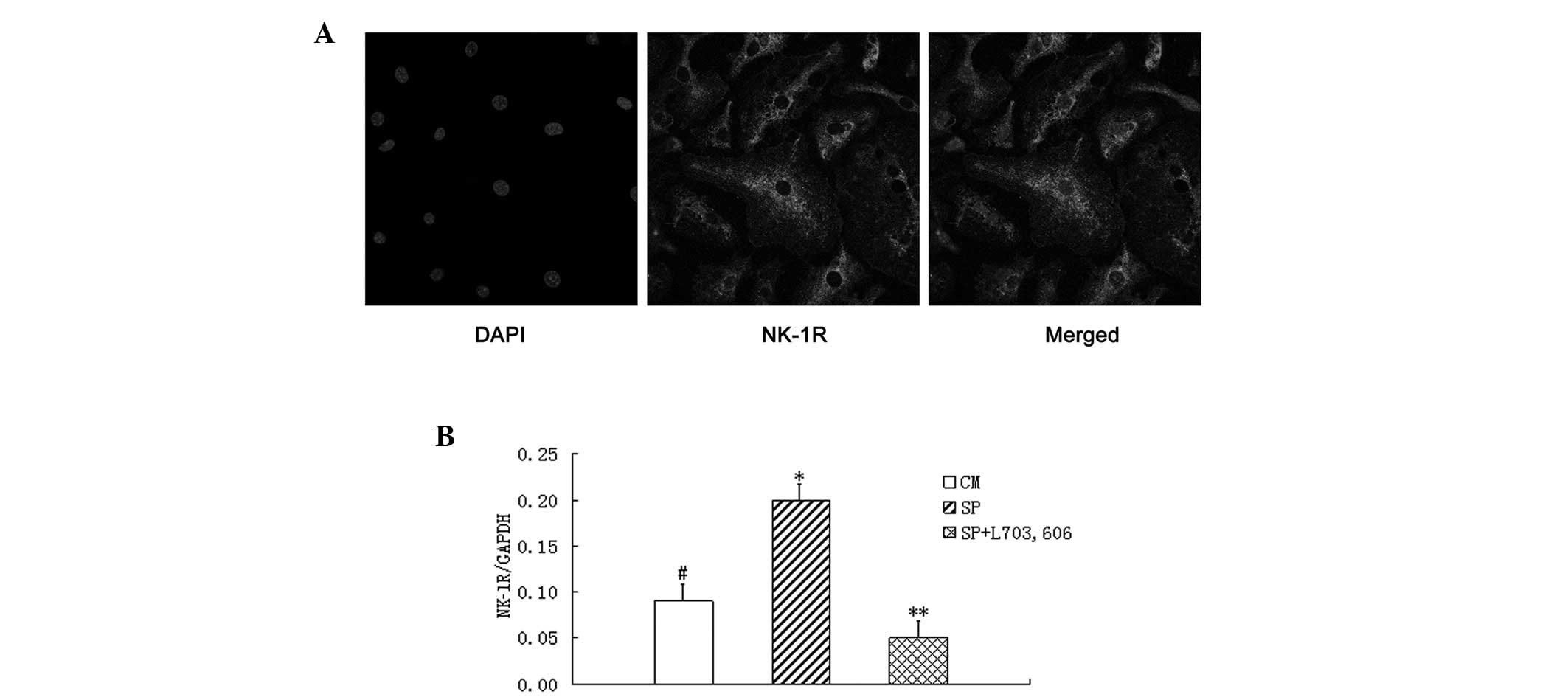
Mouse KCs express NK-1R and SP increases
NK-1R mRNA expression in KCs in vitro
NK-1R was analyzed in KCs from mice, based on
immunohistochemical localization using fluorescein. The
immunoreactivity was concentrated in the cell cytoplasm (Fig. 2A), which is different from the
results of other studies (8).
NK-1R mRNA levels were upregulated in KCs incubated with SP for 24
h. According to quantitative PCR, the results further demonstrated
that SP increased NK-1R mRNA expression 2.5-fold (Fig. 2B). NK-1R blockade eradicated the
effect of SP on NK-1R mRNA expression and significantly reduced
NK-1R mRNA expression to below the level observed in control
culture medium.
SP enhances IL-6 and TNF-α secretion and
L-703,606 inhibits SP-induced IL-6 and TNF-α release from KCs in
vitro
In order to determine whether SP-induced IL-6 and
TNF-α release is mediated through the NK-1R, KCs were pre-incubated
with the NK-1R antagonist L-703,606 (10 μM) for 15 min and
during stimulation with SP (1 μM). As shown in Table II, the cytokine (IL-6 and TNF-α)
levels in the super-natant resulting from the release from cultured
KCs revealed a substantial increase in the SP-pretreated group
compared with the control group. The IL-6/TNF-α levels of the
supernatant in the L-703,606-pretreated group were significantly
lower compared with those in the SP-pretreated group. In other
words, the SP-induced IL-6 and TNF-α secretion from KCs was
eradicated by pretreatment with L-703,606.
 | Table II.IL-6 and TNF-α levels in the
different groups. |
Table II.
IL-6 and TNF-α levels in the
different groups.
| Group | IL-6 (pg/ml) | TNF-α (pg/ml) |
|---|
| Control group | 71.13±9.36 | 31.02±7.26 |
| SP-pretreated
group |
194.12±11.09a | 92.15±8.56a |
|
L-703,606-pretreated group | 68.16±9.51b | 28.38±5.04b |
Discussion
Various factors, including viral infections,
autoimmune reactions and metabolic disorders are involved in liver
injury. ConA-induced hepatitis, which closely mimics the
pathogenesis mechanisms and pathological changes of patients, has
long been regarded as an appropriate model of human immune-mediated
liver disease (17). ConA is a
type of lectin, which is purified from Canavalia
brasiliensis. The mechanisms of the ConA model have interested
numerous scientists; when mice are treated with ConA, lymphocytes
and other mononuclear cells release lymphokines and there is a
rapid inflammatory alteration of the liver tissue, including clear
infiltration of neutrophils, macrophages and T cells, as well as a
significant simultaneous increase in the level of aminotransferase
in the peripheral blood (18). In
the current study, an acute hepatitis model was successfully
established (Fig. 1B).
Previous studies have demonstrated that the
autonomic nervous system has a pronounced effect on immune-mediated
experimental hepatitis in mice (19). It is well known that
pro-inflammatory signaling mediated by SP acts through NK-1Rs
(20). Therefore, since neurogenic
inflammation is a result of the action of SP on NK-1Rs, we aimed to
investigate whether the effects of the blockade of selective NK-1Rs
using a specific NK-1R antagonist reduced the injury. L-703,606 is
a selective NK-1R antagonist. Studies have verified that the
effects of L-703,606 are attributable to pharmacological blockade
of endogenous SP/NK-1R interactions in parallel using NK-1R −/−
animals (21). In the current
study, we observed that pretreatment with the NK-1R antagonist
L-703,606 significantly improved liver function. This was supported
by histopathological changes and our results demonstrated that
disruption of the interaction between SP and its receptor had a
therapeutic effect on liver inflammation. Therefore, it was
concluded that SP receptor (NK-1R) antagonists are good candidates
in the prevention of ConA-induced liver injury. We speculate that
this protective effect may act in part via the reduction in
cytokine levels. Therefore, we investigated whether SP induces KC
secretion of IL-6 and TNF-α in vitro.
KCs are non-parenchymal cells, which account for
∼15% of the total liver cell population and constitute 80–90% of
the tissue-resident macrophages in the whole body (22–23).
KCs represent the major source of inflammatory cytokine production
and thus the systemic release of pro-inflammatory mediators
(24). There is considerable
evidence indicating that the activation of KCs and their production
of pro-inflammatory cytokines contribute to the pathogenesis of
various liver injuries, including alcoholic liver disease (ALD),
non-alcoholic fatty liver disease (NAFLD) and liver failure
(25). The activation of KCs
results in the release of an array of inflammatory mediators,
growth factors and reactive oxygen species, including TNF-α and
IL-6, which contribute to hepatocellular damage (26). Furthermore, accumulating evidence
indicates that inactivation of KCs prevents liver injury (27). Therefore, the factors that control
the KC response are clearly critical in the progression of liver
injury. SP has been shown to affect cytokine production and release
from various immune cells. For example, SP modulates the release of
IL-1, IL-6 and TNF-α from human blood monocytes (12). In monocytes and macrophages, SP
also stimulates the release of arachidonic acid metabolites and
pro-inflammatory cytokines; it induces the respiratory burst and
acts as a potent chemoattractant (28). SP has been detected in the liver,
and receptors for SP have also been detected on KCs and
hepatocytes. However, there is limited information concerning the
correlation between SP and cytokines in KCs. Previous studies have
indicated that NK-1Rs are upregulated at sites of inflammation in a
number of tissues, including joints and the intestine (29–31).
The current study demonstrates that mouse KCs expressed NK-1R and
that treatment with SP increased NK-1R mRNA expression in KCs in
vitro. However, at this early stage, the cytokine (IL-6 and
TNF-α) levels in the supernatant resulting from the release from
cultured KCs without LPS were below the minimum detection range
(data not shown). Although LPS was involved in the experiment, it
did not affect our study since the three groups of KCs were all
incubated with it. The cytokine (IL-6 and TNF-α) levels are shown
in Table II. To the best of our
knowledge, we report for the first time that SP induces IL-6 and
TNF-α production in KCs. In the current study, L-703,606 exhibited
strong activity by reducing the production of TNF-α and IL-6 in
SP+LPS-stimulated KCs, suggesting that the inhibition of
pro-inflammatory cytokine (TNF-α and IL-6) release by KCs may
contribute to L-703,606-mediated liver protection. Further in
vivo and in vitro studies are required to determine the
exact molecular pathways affected by L-703,606, which may be useful
in the development of novel treatments for hepatic injury and
fibrosis.
In summary, the present study and our previous
findings indicate that inflammatory cytokine-mediated apoptotic
liver injury is affected by neuropeptides. NK-1R agonists,
including SP appear to be major players in this scenario by
upregulating the pro-inflammatory cytokine response. If the data
from our mouse experiments on the hepatoprotective potential of
NK-1R antagonists is transferred to clinical practice, it is likely
to have potential clinical implications, providing a future
strategy for therapeutic intervention in the treatment of liver
injuries through the suppression of KC activation and
pro-inflammatory cytokines. Moreover, these findings may offer
novel therapeutic targets for ameliorating liver fibrosis and
cirrhosis progression. In future experiments we aim to investigate
whether SP is as important in chronic liver injury as it is in
acute liver injury; this may provide new avenues of investigation
for the treatment of acute and chronic liver inflammation.
Specifically, further studies focusing on whether SP plays a role
in other biological processes of KCs, including proliferation,
survival and migration, are required to improve our
understanding.
Abbreviations:
|
Con A
|
concanavalin A;
|
|
SP
|
substance P;
|
|
NK-1R
|
neurokinin 1 receptor;
|
|
KC
|
Kupffer cell;
|
|
IL
|
interleukin;
|
|
TNF-α
|
tumor necrosis factor α
|
Acknowledgements
This study was funded by Qilu Hospital
of Shandong University
References
|
1.
|
Mackay IR: Immunological aspects of
chronic active hepatitis. Hepatology. 3:724–728. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Richardson JD and Vasko MR: Cellular
mechanisms of neurogenic inflammation. J Pharmacol Exp Ther.
302:839–845. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Sternberg EM: Neural regulation of innate
immunity: a coordinated nonspecific host response to pathogens. Nat
Rev Immunol. 6:318–328. 2006. View
Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Greco SJ, Corcoran KE, Cho KJ and
Rameshwar P: Tachykinins in the emerging immune system: relevance
to bone marrow homeostasis and maintenance of hematopoietic stem
cells. Front Biosci. 9:1782–1793. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Satake H and Kawada T: Overview of the
primary structure, tissue-distribution, and functions of
tachykinins and their receptors. Curr Drug Targets. 7:963–974.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Sterner-Kock A, Braun RK, van der Vliet A,
et al: Substance P primes the formation of hydrogen peroxide and
nitric oxide in human neutrophils. J Leukoc Biol. 65:834–840.
1999.PubMed/NCBI
|
|
7.
|
Bang R, Biburger M, Neuhuber WL and Tiegs
G: Neurokinin-1 receptor antagonists protect mice from CD95- and
tumor necrosis factor-alpha-mediated apoptotic liver damage. J
Pharmacol Exp Ther. 308:1174–1180. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Bang R, Sass G, Kiemer AK, Vollmar AM,
Neuhuber WL and Tiegs G: Neurokinin-1 receptor antagonists
CP-96,345 and L-733,060 protect mice from cytokine-mediated liver
injury. J Pharmacol Exp Ther. 305:31–39. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Kunstle G, Hentze H, Germann PG, et al:
Concanavalin A hepatotoxicity in mice: tumor necrosis
factor-mediated organ failure independent of caspase-3-like
protease activation. Hepatology. 30:1241–1251. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Smedsrød B and Pertoft H: Preparation of
pure hepatocytes and reticuloendothelial cells in high yield from a
single rat liver by means of Percoll centrifugation and selective
adherence. J Leukoc Biol. 38:213–230. 1985.PubMed/NCBI
|
|
11.
|
Lai JP, Douglas SD, Wang YJ and Ho WZ:
Real-time reverse transcription-PCR quantitation of substance P
receptor (NK-1R) mRNA. Clin Diagn Lab Immunol. 12:537–541.
2005.PubMed/NCBI
|
|
12.
|
Lotz M, Vaughan JH and Carson DA: Effect
of neuropeptides on production of inflammatory cytokines by human
monocytes. Science. 241:1218–1221. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Amoruso A, Bardelli C, Gunella G,
Ribichini F and Brunelleschi S: A novel activity for substance P:
stimulation of peroxisome proliferator-activated receptor-gamma
protein expression in human monocytes and macrophages. Br J
Pharmacol. 154:144–152. 2008. View Article : Google Scholar
|
|
14.
|
Dianzani C, Lombardi G, Collino M, Ferrara
C, Cassone MC and Fantozzi R: Priming effects of substance P on
calcium changes evoked by interleukin-8 in human neutrophils. J
Leukoc Biol. 69:1013–1018. 2001.PubMed/NCBI
|
|
15.
|
Ramnath RD and Bhatia M: Substance P
treatment stimulates chemokine synthesis in pancreatic acinar cells
via the activation of NF-kappaB. Am J Physiol Gastrointest Liver
Physio. 291:G1113–G1119. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Barreto SG, Carati CJ, Schloithe AC, et
al: The combination of neurokinin-1 and galanin receptor
antagonists ameliorates caerulein-induced acute pancreatitis in
mice. Peptides. 31:315–321. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Kaneko Y, Harada M, Kawano T, et al:
Augmentation of Valpha14 NKT cell-mediated cytotoxicity by
interleukin 4 in an autocrine mechanism resulting in the
development of concanavalin A-induced hepatitis. J Exp Med.
191:105–114. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Miyazawa Y, Tsutsui H, Mizuhara H,
Fujiwara H and Kaneda K: Involvement of intrasinusoidal hemostasis
in the development of concanavalin A-induced hepatic injury in
mice. Hepatology. 27:497–506. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Neuhuber WL and Tiegs G: Innervation of
immune cells: evidence for neuroimmunomodulation in the liver. Anat
Rec A Discov Mol Cell Evol Biol. 280:884–892. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
20.
|
Bhatia M, Zhi L, Zhang H, Ng SW and Moore
PK: Role of substance P in hydrogen sulfide-induced pulmonary
inflammation in mice. Am J Physiol Lung Cell Mol Physiol.
291:L896–L904. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
21.
|
Chauhan VS, Kluttz JM, Bost KL, et al:
Prophylactic and therapeutic targeting of the neurokinin-1 receptor
limits neuro-inflammation in a murine model of pneumococcal
meningitis. J Immunology. 186:7255–7263. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
22.
|
Vollmar B and Menger MD: The hepatic
microcirculation: mechanistic contributions and therapeutic targets
in liver injury and repair. Physiol Rev. 89:1269–1339. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
23.
|
Carini R and Albano E: Recent insights on
the mechanisms of liver preconditioning. Gastroenterology.
125:1480–1491. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
24.
|
Hildebrand F, Hubbard WJ, Choudhry MA, et
al: Kupffer cells and their mediators: the culprits in producing
distant organ damage after trauma-hemorrhage. Am J Pathol.
169:784–794. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
25.
|
Solga SF and Diehl AM: Non-alcoholic fatty
liver disease: lumen-liver interactions and possible role for
probiotics. J Hepatol. 38:681–687. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
26.
|
Koo DJ, Chaudry IH and Wang P: Kupffer
cells are responsible for producing inflammatory cytokines and
hepatocellular dysfunction during early sepsis. J Surg Res.
83:151–157. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
27.
|
Wang YY, Dahle MK, Agren J, et al:
Activation of the liver X receptor protects against hepatic injury
in endotoxemia by suppressing Kupffer cell activation. Shock.
25:141–146. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
28.
|
O’Connor TM, O’Connell J, O’Brien DI,
Goode T, Bredin CP and Shanahan F: The role of substance P in
inflammatory disease. J Cell Physiol. 201:167–180. 2004.
|
|
29.
|
Reed KL, Fruin AB, Gower AC, et al:
NF-kappaB activation precedes increases in mRNA encoding
neurokinin-1 receptor, proinflammatory cytokines, and adhesion
molecules in dextran sulfate sodium-induced colitis in rats. Dig
Dis Sci. 50:2366–2378. 2005. View Article : Google Scholar
|
|
30.
|
Keeble J, Blades M, Pitzalis C, Castro da
Rocha FA and Brain SD: The role of substance P in microvascular
responses in murine joint inflammation. Br J Pharmacol.
144:1059–1066. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
31.
|
Karagiannides I, Kokkotou E, Tansky M, et
al: Induction of colitis causes inflammatory responses in fat
depots: evidence for substance P pathways in human mesenteric
preadipocytes. Proc Natl Acad Sci USA. 103:5207–5212. 2006.
View Article : Google Scholar : PubMed/NCBI
|