Introduction
Gastrointestinal stromal tumors (GISTs) are the most
common form of mesenchymoma originating from the gastrointestinal
tract. In these GISTs, approximately 70% originate from stomach,
20–30% from the small intestine and less than 10% from the colon,
rectum and esophagus. It is thought that GISTs arise from the
interstitial cells of Cajal, and predominantly express
immunoreactivity for CD117, a tyrosine kinase growth factor
receptor (1).
Extragastrointestinal stromal tumors (EGISTs), which exhibit
similar clinicopathological and immunohistochemical features to
GISTs, are primarily observed in the greater omentum, mesentery and
retroperitoneum (2).
Immunohistochemical studies aid the correct diagnosis of EGIST.
More than 95% of EGISTs express CD117 and 50–100% express CD34,
while few are stained positively for desmin, S-100 protein, or
smooth muscle actin. Primary EGISTs originating from the prostate
are rarely encountered. To the best of our knowledge, only sporadic
cases of a confirmed primary EGIST of the prostate have been
recorded (3,4). In this study, we present a rare case
of a primary EGIST of the prostate, and describe its treatment. To
the best of our knowledge, this may have been the first case of a
prostatic EGIST treated using multimodal therapy, including radical
prostatectomy and imatinib.
Case report
A 39-year-old male presented with frequency, urgency
and dysuria for 1 year. A digital rectal examination demonstrated a
markedly enlarged prostate that exhibited the usual consistency,
and tenderness on palpation. The serum level of prostate specific
antigen (PSA) was 0.87 ng/ml, and the carcinoembryonic antigen
(CEA) and carbohydrate antigen (CA) 19-9 levels were normal. Pelvic
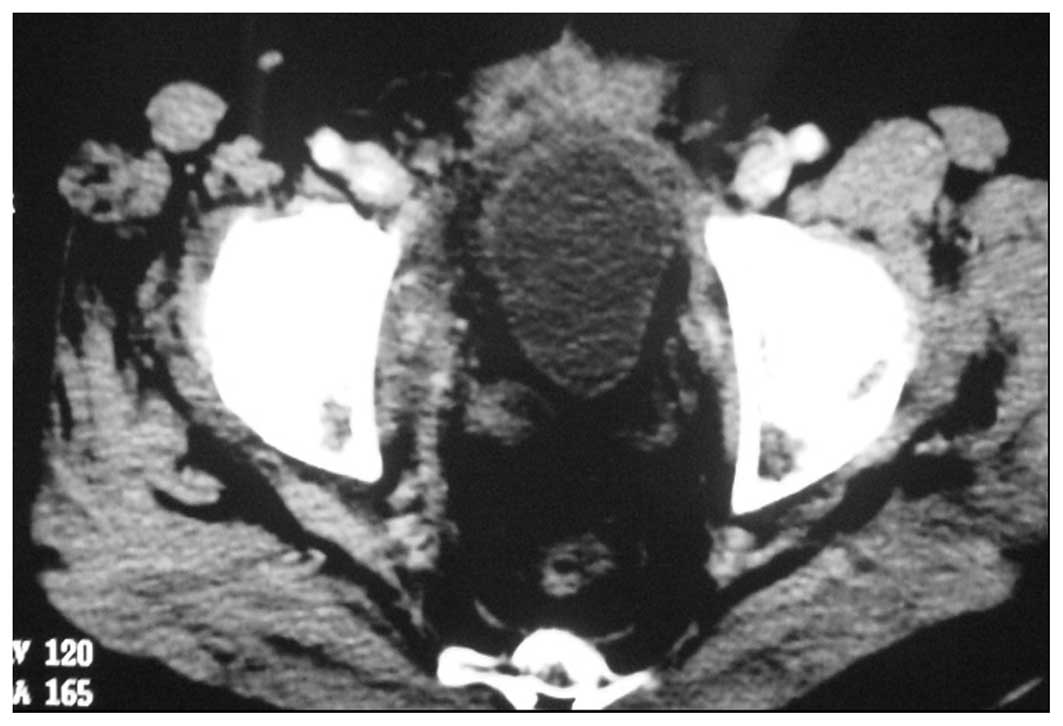
computed tomography (CT) revealed an enlarged prostate (10×6 cm)
that compressed the rectum and urinary bladder, and that appeared
heterogeneous, following contrast enhancement (Fig. 1). Enteroscopy revealed no
abnormalities, and no metastases were identified in any other
organs through ultrasonography or CT scans. A 10-core transrectal
ultrasound-guided prostate biopsy was performed, in order to obtain
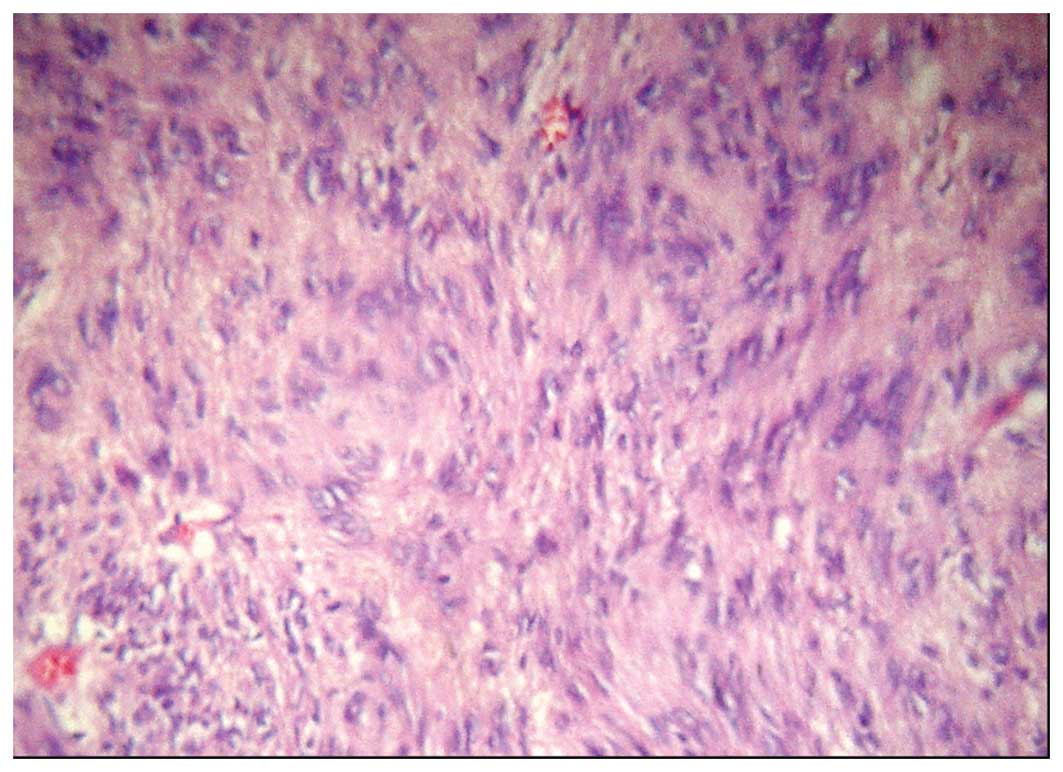
pathological specimens. The light microscopy examination
demonstrated that the tumor primarily consisted of spindle cells
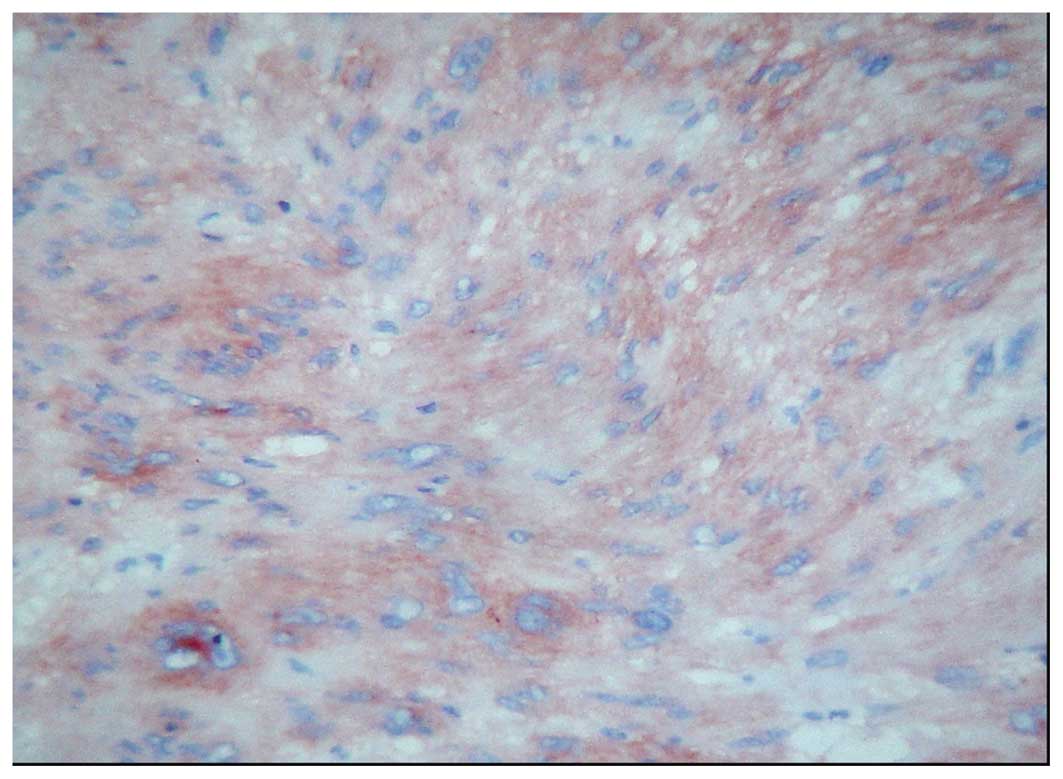
(Fig. 2). The immunohistochemical
analysis was positive for CD117 (Fig.
3), CD34 and vimentin, while negative results were obtained for
cytokeratin, desmin, S100 protein and smooth muscle actin. A
pathological diagnosis of EGIST of the prostate was made, prior to
the patient undergoing a radical prostatectomy. Intraoperatively,
the tumor was noted to be confined to the prostate, without the
involvement of the rectum, and no enlarged pelvic lymph nodes were
detected. The size of the resected prostate specimen was
10.0×7.0×6.5 cm, and the final pathological examination confirmed
the diagnosis of prostatic EGIST. The surgical margins were
evaluated, and a positive microscopic margin was identified at the
tip of the prostatic apex. Subsequently, the patient received
targeted imatinib therapy (400 mg, daily) for 1 year. The patient
was placed under observation for 24 months, and, in that period, no
recurrence or metastasis was exhibited (Fig. 4). This case report was approved by
the ethics committee of the Central South University (Changsha,
China), and informed patient consent was obtained.
Discussion
Neoplasms that occur as primary tumors outside the
alimentary tract, and that exhibit similar morphological,
immunophenotypical and molecular genetic characteristics to GISTs,
are known as EGISTs. Due to the EGISTs, it is important to confirm
whether the tumor is associated with the digestive tract, prior to
making the diagnosis of EGIST. There are few case reports
concerning EGISTs with a potential origin in the prostate; however,
several cases of GISTs arising from the rectum have been
misdiagnosed as prostatic EGISTs (5). When making a diagnosis of prostatic
EGIST, it is necessary for clinicians to be prudent. The first case
of a GIST that potentially originated from the prostate was
revealed by Van der Aa et al (5). A 49-year-old male was demonstrated to
have a large prostatic mass, and a biopsy revealed the presence of
a GIST. Treatment with imatinib resulted in a reduction in the size
of the mass. However, it was not possible to confirm the diagnosis
of prostatic EGIST in the absence of surgical excision. In the
present case, enteroscopy and CT revealed no abnormalities intra-
or extrarectally, and the light microscopy examination and
immunohistochemical analysis of the biopsy specimens confirmed the
pathological diagnosis of GIST. Intraoperatively, the tumor was
noted to be confined to the prostate, without involvement of the
rectum. The preoperative examinations, pathological results and
intraoperative investigations confirmed that the tumor was an
EGIST, primarily originating from the prostate. Two additional
cases of GISTs of a prostatic origin have been studied by Lee et
al and Yinghao et al (3,4). The
patients concerned in these cases received radical prostatectomy,
which revealed that the tumors were confined to the prostate.
Surgical resection is currently the primary
treatment option for non-metastatic EGISTs (6). For prostatic masses, transrectal
ultrasound-guided prostate biopsies may assist in the determination
of a treatment strategy. With regard to prostatic EGISTs, radical
prostatectomy is considered to provide satisfactory results. In the
present case report, a radical prostatectomy was conducted on the
patient, since preoperative examinations did not reveal metastases.
Imatinib, a selective protein tyrosine kinase inhibitor, has been
demonstrated to be an effective treatment for GISTs and EGISTs
(7–10). In the present case, the
postoperative pathological examination revealed a positive
microscopic margin in the surgical specimen. As a result of this,
the patient was considered to be at a high risk of recurrence;
therefore, the patient received imatinib treatment for 1 year, in
addition to surgery. In the two cases of prostatic EGISTs mentioned
previously, the patients received surgical treatment without
imatinib therapy, since positive microscopic margins were not
identified. However, in the present case, the absence of recurrence
or metastasis in the 24-month follow-up period indicated that
surgery combined with imatinib therapy was an effective course of
treatment for this patient.
In conclusion, this study presents a rare case of an
EGIST originating from the prostate, which was treated using
multi-modal therapy. The results from this case indicate that
surgical resection, followed by imatinib therapy, may offer a
promising outcome for patients diagnosed with prostatic EGIST,
where there is a high risk of recurrence.
References
|
1.
|
Gold JS and Dematteo RP: Combined surgical
and molecular therapy: the gastrointestinal stromal tumor model.
Ann Surg. 244:176–184. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Reith JD, Goldblum JR, Lyles RH and Weiss
SW: Extragastrointestinal (soft tissue) stromal tumors: an analysis
of 48 cases with emphasis on histologic predictors of outcome. Mod
Pathol. 13:577–585. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Lee CH, Lin YH, Lin HY, Lee CM and Chu JS:
Gastrointestinal stromal tumor of the prostate: a case report and
literature review. Hum Pathol. 37:1361–1365. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Yinghao S, Bo Y and Xiaofeng G:
Extragastrointestinal stromal tumor possibly originating from the
prostate. Int J Urol. 14:869–871. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Van der Aa F, Sciot R, Blyweert W, et al:
Gastrointestinal stromal tumor of the prostate. Urology.
65:3882005.PubMed/NCBI
|
|
6.
|
Xue D, Chen H and Chen Y: Giant
extragastrointestinal stromal tumor in the transverse mesocolon
concomitant with gastric cancer in an elderly patient: Case report.
Oncol Lett. 5:627–630. 2013.PubMed/NCBI
|
|
7.
|
van Oosterom AT, Judson I, Verweij J, et
al European Organisation for Research and Treatment of Cancer Soft
Tissue and Bone Sarcoma Group: Safety and efficacy of imatinib
(STI571) in metastatic gastrointestinal stromal tumours: a phase I
study. Lancet. 358:1421–1423. 2001.PubMed/NCBI
|
|
8.
|
Demetri GD, von Mehren M, Blanke CD, et
al: Efficacy and safety of imatinib mesylate in advanced
gastrointestinal stromal tumors. N Engl J Med. 347:472–480. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Casali PG, Jost L, Reichardt P and
Schlemmer M: Gastrointestinal stromal tumors: ESMO clinical
recommendations for diagnosis, treatment and follow-up. Ann Oncol.
19(Suppl 2): ii35–ii38. 2008.PubMed/NCBI
|
|
10.
|
Barros A, Linhares E, Valadão M, Gonçalves
R, Vilhena B, Gil C and Ramos C: Extragastrointestinal stromal
tumors (EGIST): a series of case reports. Hepatogastroenterology.
58:865–868. 2011.PubMed/NCBI
|