Introduction
The incidence of pulmonary embolism is increasing,
and deep vein thrombosis (DVT) in the lower extremities is one of
the main causes. It is reported that one-third of patients with an
acute phase of DVT may suffer from acute pulmonary embolisms
(1,2). Vena cava filter (VCF) placement is an
effective measure for preventing pulmonary embolisms in DVT
patients. It has the advantage of being a simple procedure, with
minimal trauma and few complications, and has been widely applied
clinically (3–6). As the outer sheaths of commercially
available filters are becoming increasingly thinner, the
traditional VCF placement method has changed from the percutaneous
incision of a deep vein to Seldinger’s method (7,8),
dominated by the percutaneous puncture of a deep vein. Currently,
the placement pathways for VCFs are mainly the femoral and jugular
veins (9), and the pathways of the
subclavian, brachial and external jugular veins have also been
reported (10,11). However, since a risk of
complications arising from VCF placement via puncture of a deep
vein remains, it is important to investigate safe and feasible
puncture pathways for clinical use. The great saphenous vein (GSV),
as a superficial vein, is not a traditional pathway for
intracavitary therapy in lower extremity veins, but the puncture
and incision via the superficial venous pathway has been reported
(12,13). In the current study, using
ultrasound positioning, the placement of a VCF via the percutaneous
puncture of the GSV was performed on DVT patients, and the
feasibility and safety of this method were investigated.
Materials and methods
General data
A total of 12 patients with DVT (5 males and 7
females) were enrolled in this study at the Affiliated Suzhou
Hospital of Nanjing Medical University. The patients were aged
between 48 and 87 years, with an average age of 51.5 years
(Table I). The disease onset time
was <1 week. All patients were diagnosed with unilateral DVT
(left lateral, 9 cases; right lateral, 3 cases) using color Doppler
ultrasound, venography and plasma D-dimer determination. According
to the results of the venography, there were 4 central type, 4
peripheral type and 4 mixed type cases of DVT. VCFs were provided
by Johnson & Johnson Co. (New Brunswick, NJ, USA).
Trapease® permanent filters were used to treat 4
patients, while the other 8 patients were treated with
Optease® temporary filters. THe present study was
approved by the Ethics Committee of Affiliated Suzhou Hospital of
Nanjing Medical University (Suzhou, China). Informed consent was
obtained from the patient.
 | Table I.Clinical and puncture
characteristics. |
Table I.
Clinical and puncture
characteristics.
| Total (n) | 12 |
| Male | 5 |
| Female | 7 |
| Age, mean (range),
years | 51.5 (48–87) |
| DVT (n) | |
| Central | 4 |
| Peripheral | 4 |
| Mixed | 4 |
| GSV puncture (n) | |
| Left | 9 |
| Right | 3 |
Preoperative preparation
A preoperative routine blood test, blood coagulation
test and other examinations were conducted on all patients. The
inclusion criteria for VCF placement were as follows: definite
pulmonary infarction symptoms or tendency, contraindication of
anticoagulation, consideration of transcatheter thrombolysis, poor
anticoagulation or re-thrombosis.
Surgical methods
VCF placements via puncture of the unaffected
lateral and affected lateral GSV were performed on 10 and 2
(central type) patients, respectively. The selected puncture point
was located at the upper-middle segment of the inner thigh. After
disinfection and local anesthesia, the thigh was ligatured using a
tourniquet to temporarily block venous return and vein dilatation.
Using color Doppler ultrasound positioning, puncture of the GSV was
performed, and the gliding guide wire was placed, from the
saphenous vein valve to the femoral vein and then on to the vena
cava. The remaining surgical steps were the same as with a
traditional filter placement method. The venography was conducted
and once the outlet positions of bilateral renal veins were
determined, the filter was released.
After releasing the filter, transcatheter
thrombolysis in a deep vein by puncturing the jugular vein was
undertaken in the majority of patients (14,15).
For patients with thrombosis in the entirety of their lower
extremities, transcatheter thrombolysis was conducted in the
affected lateral femoral artery. For two patients with central type
DVT, after puncturing the GSV, the catheter was placed directly
into the thrombus for thrombolysis. The puncture wound of the GSV
was treated with pressure bandaging.
Postoperative treatment
After lying in a horizontal position for 6 h
postoperatively, the patients were able to perform out-of-bed
activities, with the exception of 2 cases where there was
catheterization in the GSV. For patients undergoing thrombolytic
and anticoagulant therapies, the coagulation change was monitored,
and oozing ecchymosis at the puncture point and at the
catheterization site was observed every day. The thrombolytic
situation was monitored by venography to enable adjustment of the
catheter position. The catheter was extubated 2 weeks after
thrombolysis; furthermore, the temporary filters may be retrieved
after thrombolysis.
Results
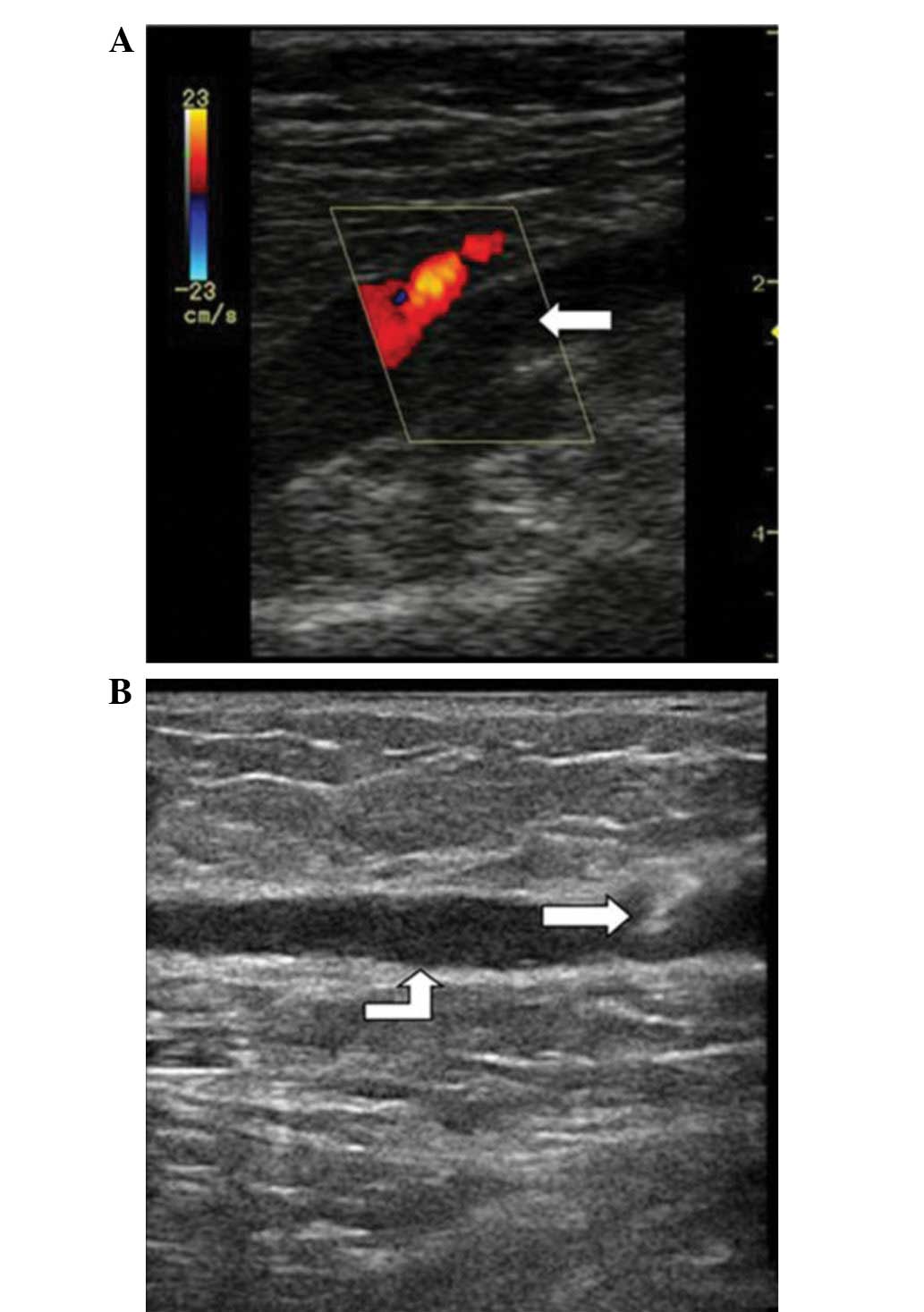
All filters were successfully released, using
accurate ultra-sound positioning. In 6 out of 8 patients with
temporary filter placement, filters were successfully retrieved
within 3 weeks of surgery. A further two patients did not undergo
retrieval due to economic reasons. The ultrasound-guided puncture
was successfully conducted on all patients (Fig. 1). Throughout the perioperative
period, there was no marked hematoma at the puncture point. For
some patients, local petechiae appeared around the puncture point
during the thrombolysis period, which did not require treatment.
For all patients, re-examination with a color Doppler ultrasound
revealed unobstructed blood flow in the GSV, with no back flow or
thrombosis. Within 1 year of follow-up there had been no instances
of pulmonary embolism.
Discussion
At present, VCF placement via puncture of a deep
vein (Seldinger’s method) is widely used in a clinical environment.
This method has many advantages, including less trauma and fewer
complications, and it is a simple surgery. However, puncture of a
deep vein, particularly the femoral vein, has the following
disadvantages: i) a hematoma is easily formed in anticoagulant and
thrombolytic conditions, and it is difficult to detect and treat
early due to its deep position. ii) There is a risk of local
thrombosis at the puncture and catheterization site. iii) The
femoral venous valve may be damaged. iv) Puncture is seldom
successful for obese patients. v) The arteries may be mistakenly
punctured, particularly for patients in whom the femoral vein is
located on the dorsal side of the femoral artery. Additionally, the
risk of hematoma and pseudoaneurysm formation will be aggravated
during subsequent anticoagulant and thrombolytic therapy. vi) The
puncture point is near the perineum, leading to problems with
postoperative care (16,17).
However, puncture of the GSV may avoid the risks
listed above. Most regions of the GSV are located at the
superficial fascia layer. It is possible to detect bleeding or
hematoma early and easily, and compression hemostasis is easily
conducted. Due to shielding by the saphenofemoral valve, the inner
wall and valve of the GSV to not readily become detached and enter
the deep vein, even if the injury has induced secondary thrombosis.
Therefore, the probability of deep vein valve injury is very low.
The anatomical location of the GSV is superficial, with no
accompanying artery. The puncture site is relatively flexible when
using ultrasound positioning, and the iliac region may be
avoided.
GSV puncturing has been performed by a number of
physicians. For example, transcatheter thrombolysis and stent
placement through the saphenous vein pathway have been conducted by
interventional physicians with good results. Additionally, filter
placement via GSV incision has also been performed, and the
aforementioned advantages have been confirmed (18–24).
Anatomical data indicate that the full diameter of a normal GSV is
>2 mm and that in the thigh it is 3.2–4.0 mm (25). However, temporarily blocking
superficial venous backflow may cause vein dilatation, enabling the
GSV to accommodate a 6–7 F filter. Therefore, VCF placement via
puncture of the GSV has a theoretical and practical basis, and the
feasibility is demonstrated in the current study.
In this study, as the affected lateral GSV in the
DVT patient is one of the important compensatory lateral branches,
the puncture is conducted on an unaffected lateral GSV. This avoids
injury to the affected lateral GSV and the effect on compensatory
venous backflow. During follow-up, GSV injuries caused by the
puncture, including thrombus formation, valve damage and blood
reflux, have not been observed. Filter placement and transcatheter
thrombolysis via puncture of the GSV were performed on two patients
with central type DVT. The entire procedure was completed with only
one puncture wound on the superficial vein, and it was minimally
invasive with a satisfactory result. However, this method still has
clinical disadvantages, as the filter sheath may cause shedding of
the thrombus, leading to acute pulmonary embolism.
The VCF used in this study, with a 6 F diameter, is
much thinner than other commercially available products.
Furthermore, this filter has advantages such as a simple releasing
procedure, convenient positioning and a higher success rate of
retrieval (retrievable filter) (26–30).
At present, retrievable filters are more likely to be used in a
clinical setting, for the following reasons: firstly, the
indications for filter placement are controversial, and previously
reported results of long-term efficacy and complications differ
(31–34); and secondly, in younger patients
with DVT, a permanent filter would not be suitable.
In the current study, VCF placement via puncture of
the GSV has not provided optimal results. The injury risk of GSV
puncture remains and, most notably, commercially available filters
have not provided the ideal minimally invasive result. In our
hospital, GSV radiofrequency laser closure surgery has been
conducted on >500 patients and as such we have accumulated a
large amount of experience. Puncture of the GSV on the upper medial
malleolus has been conducted successfully in the majority of
patients, with the placement of a 6–8 F sheath. The advantages of
puncture at this position are as follows: i) The surgery is simple.
For the majority of patients ultrasound positioning is not
required, and a trocar may been placed under direct vision. It is
possible to complete the puncture using a small guide wire
(diameter, 0.018 inch). ii) As the GSV is located at the surface of
the medial malleolus, it is easier to conduct the compression
hemostasis, and wound oozing is easily observed. However, due to
the shorter length of the filter, it is not possible to further
attempt these measures at present.
In conclusion, VCF placement via percutaneous
puncture of the GSV is a new filter placement method. The
feasibility and safety of this method for the prevention of
pulmonary embolism has been demonstrated in a small set of sample
cases.
References
|
1.
|
Imberti D, Ageno W, Manfredini R, et al:
Interventional treatment of venous thromboembolism: a review.
Thromb Res. 129:418–425. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
White RH: The epidemiology of venous
thromboembolism. Circulation. 107:I4–I8. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Kearon C, Kahn SR, Agnelli G, Goldhaber S,
Raskob GE and Comerota AJ; American College of Chest Physicians:
Antithrombotic therapy for venous thromboembolic disease: American
College of Chest Physicians evidence-based clinical practice
guidelines (8th Edition). Chest. 133(6 Suppl): 454S–545S. 2008.
View Article : Google Scholar
|
|
4.
|
Decousus H, Leizorovicz A, Parent F, et
al: A clinical trial of vena caval filters in the prevention of
pulmonary embolism in patients with proximal deep-vein thrombosis.
Prevention du Risque d’Embolie Pulmonaire par Interruption Cave
Study Group. N Engl J Med. 338:409–415. 1998.
|
|
5.
|
Young T, Tang H and Hughes R: Vena caval
filters for the prevention of pulmonary embolism. Cochrane Database
Syst Rev. 2:CD0062122010.
|
|
6.
|
Athanasoulis CA, Kaufman JA, Halpern EF,
Waltman AC, Geller SC and Fan CM: Inferior vena caval filters:
review of a 26-year single-center clinical experience. Radiology.
216:54–66. 2000.PubMed/NCBI
|
|
7.
|
Luke HA: Angiography of the aorta and
great vessels; Seldinger’s technique of arterial catheterization.
Clin Rep. 8:31–54
|
|
8.
|
Taber SW and Bergamini TM: Long-term
venous access: indications and choice of site and catheter. Semin
Vasc Surg. 10:130–134. 1997.PubMed/NCBI
|
|
9.
|
Tadavarthy SM, Castaneda-Zuniga W,
Salomonowitz E, et al: Kimray-Greenfield vena cava filter:
percutaneous introduction. Radiology. 151:525–526. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
McCowan TC, Ferris EJ, Carver DK and
Harshfield DL: Use of external jugular vein as a route for
percutaneous inferior vena caval filter placement. Radiology.
176:527–530. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Théry C, Asseman P, Becquart J, Bauchart
JJ, Jabinet JL and Marache P: Temporary caval filter allowing
diagnosis and fibrinolytic therapy in patients suspect of massive
pulmonary embolism. Arch Mal Coeur Vaiss. 84:525–530. 1991.(In
French).
|
|
12.
|
Adelman S: An emergency intravenous route
for the pediatric patient. JACEP. 5:596–598. 1976. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Beitzke A, Gamillscheg A, Nagel B and
Koestenberger M: Femoral vein access by contrast-guided puncture in
cardiac catheterization in patients under one year of age. Pediatr
Cardiol. 30:768–770. 2009.PubMed/NCBI
|
|
14.
|
Baekgaard N, Broholm R, Just S, Jørgensen
M and Jensen LP: Long-term results using catheter-directed
thrombolysis in 103 lower limbs with acute iliofemoral venous
thrombosis. Eur J Vasc Endovasc Surg. 39:112–117. 2010. View Article : Google Scholar
|
|
15.
|
Sillesen H, Just S, Jørgensen M and
Baekgaard N: Catheter directed thrombolysis for treatment of
ilio-femoral deep venous thrombosis is durable, preserves venous
valve function and may prevent chronic venous insufficiency. Eur J
Vasc Endovasc Surg. 30:556–562. 2005. View Article : Google Scholar
|
|
16.
|
Grassi CJ, Swan TL, Cardella JF, et al:
Quality improvement guidelines for percutaneous permanent inferior
vena cava filter placement for the prevention of pulmonary
embolism. SCVIR Standards of Practice Committee. J Vasc Interv
Radiol. 12:137–141. 2001. View Article : Google Scholar
|
|
17.
|
Blebea J, Wilson R, Waybill P, et al: Deep
venous thrombosis after percutaneous insertion of vena caval
filters. J Vasc Surg. 30:821–828. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Li Z, Lu W, Zhao Y, Yu Y, Yang D and Liu
Q: The stent treatment of vena iliaca through great saphenous vein
in Cockett syndrome. Chin J Surg. 48:1896–1897. 2010.
|
|
19.
|
Su H-B, Gu J-P, Lou W-S, et al:
Catheter-directed thrombolysis for acute iliofemorai deep vein
thrombosis via the ipsilateral great saphenous vein approach: a
comparative clinical study. Chin J Radiol. 45:1185–1189. 2011.
|
|
20.
|
Li X, Liu W and Zhang C: The analysis of 7
cases: thrombolysis catheter treatment of cohort superficial vein
through great saphenous vein in patients with acute legs deep
venous thrombosis. Chin J Trauma Disabil Med. 20:76–77. 2012.
|
|
21.
|
Ye B, Xia L, Xie Y and Deng X: The
intracavitary therapy of Cockett syndrome thtough left great
saphenous vein. J Gannan Med Univ. 26:384–385. 2006.
|
|
22.
|
Chen G, Gu J, Su H, et al: Application of
venography of lower extremity via a percutaneous great saphenous
vein access. J Clin Radiol. 27:514–517. 2008.
|
|
23.
|
Zhang Y, Zhang Q, Lou R, Meng L and Wang
X: Filter insertion treatment of small incision through the
saphenous vein of inferior vena cava: 30 cases of clinical
observation. Chin J Gen Surg. 17:610. 2002.
|
|
24.
|
Zhang Y, Zhang Q, Lou Y, et al: Clinical
appficafion of inferior vena cava filter placement through great
saphenous vein. Zhejiang Med J. 28:264–266. 3202006.
|
|
25.
|
Spivack DE, Kelly P, Gaughan JP and van
Bemmelen PS: Mapping of superficial extremity veins: normal
diameters and trends in a vascular patient-population. Ultrasound
Med Biol. 38:190–194. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
26.
|
Oliva VL, Szatmari F, Giroux MF, Flemming
BK, Cohen SA and Soulez G: The Jonas study: evaluation of the
retrievability of the Cordis OptEase inferior vena cava filter. J
Vasc Interv Radiol. 16:1439–1445. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
27.
|
Rosenthal D, Swischuk JL, Cohen SA and
Wellons ED: OptEase retrievable inferior vena cava filter: initial
multicenter experience. Vascular. 13:286–289. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
28.
|
Ziegler JW, Dietrich GJ, Cohen SA,
Sterling K, Duncan J and Samotowka M: PROOF trial: protection from
pulmonary embolism with the OptEase filter. J Vasc Interv Radiol.
19:1165–1170. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
29.
|
Onat L, Ganiyusufoglu AK, Mutlu A, et al:
OptEase and TrapEase vena cava filters: a single-center experience
in 258 patients. Cardiovasc Intervent Radiol. 32:992–997. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
30.
|
Kalva SP, Marentis TC, Yeddula K,
Somarouthu B, Wicky S and Stecker MS: Long-term safety and
effectiveness of the “OptEase” vena cava filter. Cardiovasc
Intervent Radiol. 34:331–337. 2011.
|
|
31.
|
Millward SF, Grassi CJ, Kinney TB, et al:
Reporting standards for inferior vena caval filter placement and
patient follow-up: supplement for temporary and
retrievable/optional filters. J Vasc Interv Radiol. 16:441–443.
2005. View Article : Google Scholar
|
|
32.
|
Imberti D, Ageno W and Carpenedo M:
Retrievable vena cava filters: a review. Curr Opin Hematol.
13:351–356. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
33.
|
Nicholson W, Nicholson WJ, Tolerico P, et
al: Prevalence of fracture and fragment embolization of Bard
retrievable vena cava filters and clinical implications including
cardiac perforation and tamponade. Arch Intern Med. 170:1827–1831.
2010. View Article : Google Scholar
|
|
34.
|
Redberg RF: Medical devices and the FDA
approval process: balancing safety and innovation; comment on
“prevalence of fracture and fragment embolization of bard
retrievable vena cava filters and clinical implications including
cardiac perforation and tamponade”. Arch Intern Med. 170:1831–1833.
2010.PubMed/NCBI
|