Introduction
The two basic principles in spine and spinal cord
surgery are the complete resection of the intraspinal tumor and the
restoration of spinal stability (1,2).
Multisegment laminectomy is typically performed to achieve complete
exposure and resection of the intradural tumor. However,
intraspinal epidural scar adhesions, spinal instability, kyphosis
and additional complications are usually identified postoperatively
(3,4). Following the introduction of lamina
replantation by Raimondi in 1976 (5), various technologies that assist in
the procedure have been developed (6–9). The
clinical effect of lamina replantation is limited due to a lack of
appropriate internal fixation techniques. Although lamina
replantation with fixation by a mini-plate is more commonly
utilized in cervical treatment, this approach has also been used in
thoracolumbar spinal surgery (10). However, further clinical cases and
studies of the long-term effects of the method are required. The
present study aimed to investigate the clinical effect of lamina
replantation with ARCH plate fixation on patients diagnosed with
thoracic and lumbar intraspinal tumors, following laminectomy.
Materials and methods
Patient data
From February 2009 to June 2010, 13 patients (32
segments) with thoracic and lumbar intraspinal tumors underwent
lamina replantation with fixation using an ARCH plate (Synthes
Inc., Wilmington, DE, USA) following laminectomy (Table I). Following the surgery, the
majority of the patients experienced pain in the thoracic and
lumbar regions during rest or when sleeping, along with lower limb
numbness and weakness. In addition, the patients endured
difficulties associated with urination or defecation. This study
was conducted in accordance with the Declaration of Helsinki, and
with approval from the ethics committee of The Second People’s
Hospital of Changzhou, Nanjing Medical University (Changzhou,
China). Written informed consent was obtained from all
participants.
 | Table I.Clinical data of patients. |
Table I.
Clinical data of patients.
| Case no. | Gender | Age (years) | Diagnosis | Position | Replantation
segments |
|---|
| 1 | Male | 45 | Neurilemmoma | Thoracolumbar
segment | 2 |
| 2 | Female | 40 | Meningioma | Thoracic
vertebra | 2 |
| 3 | Female | 33 | Hemangioma | Thoracic
vertebra | 2 |
| 4 | Female | 46 | Neurilemmoma | Thoracolumbar
segment | 3 |
| 5 | Female | 28 | Astrocytoma | Thoracolumbar
segment | 3 |
| 6 | Male | 42 | Ependymoma | Thoracolumbar
vertebra | 3 |
| 7 | Female | 48 | Meningioma | Thoracic
vertebra | 2 |
| 8 | Male | 38 | Neurilemmoma | Thoracolumbar
segment | 3 |
| 9 | Male | 52 | Meningioma | Lumbar vertebrae | 2 |
| 10 | Male | 46 | Meningioma | Thoracolumbar
segment | 3 |
| 11 | Female | 33 | Meningioma | Thoracolumbar
segment | 2 |
| 12 | Female | 36 | Ependymoma | Lumbar vertebrae | 2 |
| 13 | Female | 42 | Neurilemmoma | Thoracolumbar
segment | 3 |
Surgical technique
The patients were administered general anesthesia
through tracheal intubation, and the surgery was performed with
patients in the prone position. A medial longitudinal incision was
made along the thoracic and lumbar spine, and the bilateral
sacrospinalis were separated to the small joints. Based on the
location of the tumor, which was determined by MRI, the spinous
process and vertebral lamina that required cutting were exposed,
while the supra- and interspinous ligaments remained intact. The
cortex of the lamina was cut (2–3 mm) with a bone drill between the
lateral lamina and the inner small joints, and an osteotome was
then used to cut through the lamina. The supra- and interspinous
ligaments, as well as the ligamentum flavum of the tail were cut in
order to isolate the spinous ligament complex. The spinous ligament
complex was then turned over and fixed in the head end. The tumor
was exposed and removed, which resulted in a reduction in spinal
cord compression. The spinous ligament complex was reset, and the
inter- and supraspinous ligaments were sutured with polydioxane
monofilament synthetic (PDS) II absorbable sutures (DePuy
Orthopaedics, Inc., Warsaw, IN, USA). An ARCH steel plate of the
appropriate size and shape was inserted and fixed bilaterally with
titanium screws, following the resetting of the lamina. The tube
placement was drained, and then the incision was washed and closed
at each layer.
Antibiotics were routinely administered intra- and
postoperatively. On the first day following surgery, the patients
were required to perform back muscle exercises in bed. A girdle
brace was introduced to patients that performed exercise in bed for
three days following the surgery. Two weeks following surgery, the
patients were permitted out of bed with the assistance of a girdle
brace. The waist brace was removed one month following the
surgery.
Therapeutic evaluations
The visual analog scale (VAS) and the Oswestry
Disability Index (ODI) were used for pre- and postoperative
therapeutic evaluation.
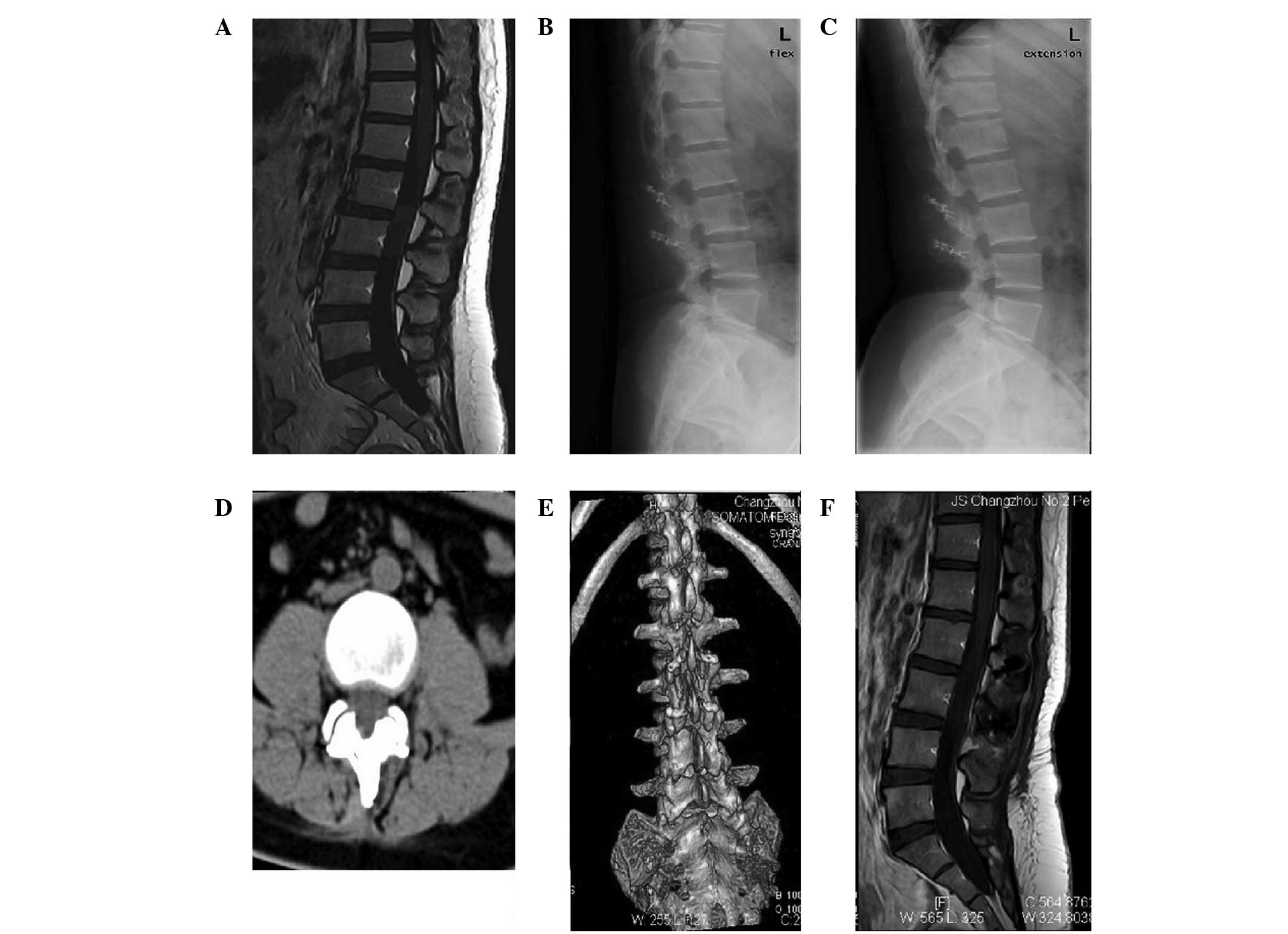
Imaging evaluation
To determine the level of internal fixation and
spinal stability, lumbar spine X-rays were performed in the
posterior-anterior, lateral and flexion-extension positions, one
day prior to the surgery, and at 2 weeks, and 1, 3, 6 and 12 months
following the surgery. A computed tomography (CT) scan was
performed three months following surgery and monthly thereafter,
until the lamina bones had fused. Furthermore, the bone growth of
the regrafted lamina was evaluated. Six months following the
surgery, magnetic resonance imaging (MRI) was performed to detect
tumor recurrence and scar oppression in the spinal canal, and the
repair of the ligaments.
Statistical analysis
The VAS and ODI scores were expressed as the mean ±
standard deviation. A paired t-test was performed using the SPSS
software, version 11.0 (SPSS, Inc., Chicago, IL, USA). P<0.05
and P<0.01 were considered to indicate a statistically
significant difference.
Results
Clinical effects
The thirteen patients in this study underwent
successful surgery and demonstrated primary healing. One patient
with ependymoma who developed postoperative cerebral spinal fluid
(CSF) leakage spontaneously recovered following conservative
treatment. The development of complications following the surgery
did not occur in the other patients. In addition, the thoracolumbar
and back pain was significantly relieved or disappeared following
the surgery, while the numbness of the limbs also decreased in
intensity.
One month following the surgery, two of the cases
were lost to follow-up. The follow-up period in the remaining 11
patients was 9–22 months, with a final follow-up period of >3
months. The VAS and ODI scores of the patients are shown in
Table II.
 | Table II.VAS and ODI scores. |
Table II.
VAS and ODI scores.
| Scale | One day prior to
surgery | Two weeks following
surgery | Final follow-up |
|---|
| VAS | 8.8±1.5 | 2.8±1.3a | 1.1±0.4a,b |
| ODI (%) | 89.3±9.2 | 52.8±6.5c | 10.8±2.3a,d |
Biomechanical test results
In the present study, a biomechanical test of the
lumbar lamina replantation with ARCH steel plate fixation was
completed, which showed that following the surgery the vertebral
strain increased by 36–60%, the transverse transposition increased
by 38–49%, the stiffness decreased by 26–57% and the carrying
capacity decreased by 32–45%. In addition, lamina replantation with
plate fixation resulted in similar levels of vertebral strain,
transposition, stiffness and carrying capacity, following surgery,
compared with normal levels (difference, 4–11%; P<0.05).
MRI findings
Following the surgery, no fixation transposition or
fracture, lumbar instability or kyphosis was identified. In
patients with a follow-up period of >6 months, favorable healing
of the vertebral lamina without bone restenosis or intraspinal
epidural scar adhesions was observed (Fig. 1).
Discussion
It has been indicated that a posterior approach to
the spine may provide access to a wider area of the spine during
surgery, and therefore reveal the intraspinal tumor for complete
resection. However, the clinical application of a posterior
approach is limited due to the wide removal of bone and ligaments,
as well as the high risk of peridural adhesions and spinal cord
injury, which are associated with weak bone protection (11,12).
Previous short-term follow-up studies on the
laminectomy procedure demonstrated a high degree of satisfaction
and spinal stability (13,14). However, in long-term studies, the
satisfaction rate decreased to <60%, as lumbar instability
resulted in chronic lower back pain (15,16).
A long-term study by Mullin et al (17) identified that 54% of patients with
dynamic lumbar instability had previously undergone total
laminectomy. In addition, Papagelopoulos et al (14) revealed that 28% of young patients
(≤30 years) treated with thoracolumbar multisegment laminectomy
exhibited spinal deformity. Iida et al (11) demonstrated that extensive
laminectomy induced intervertebral instability. Moreover, a
posterior structure resection was more likely than nucleus pulposus
removal to cause postoperative spinal instability. However, Tsuji
et al (18) demonstrated
that lower back pain and sensory disturbance were marginally
improved following laminectomy.
Laminoplasty is considered to be important for young
patients with benign tumors, so as to avoid postoperative
complications associated with laminectomy, such as refractory back
pain and spinal deformity (5,19).
Two-stage antero-posterior spinal fusion and internal fixation may
provide favorable clinical outcomes compared with laminectomy;
single-stage extensive laminectomy may cause posterior bone
deficiency (12). In China,
single-stage laminectomy, nail-stick system fixation and bone
fusion surgery have been used to achieve immediate spinal
stability. These procedures have resulted in a large surgical
field, segment movement disorder and peripheral segment
degeneration (20).
The long-term postoperative complications have not
been increased; however, numerous scholars have adopted various
techniques in order to treat thoracic and lumbar intraspinal tumors
(2,6–9,13,21,22).
Menku et al proposed the application of a mini-plate in
thoracic and lumbar laminoplasty, as opposed to its traditional
usage in the cervix, to fix the replanted lamina, and to provide
immediate stability and a smaller surgical incision (10).
Results of biomechanical tests showed that the
technique of lamina replantation with ARCH plate fixation was able
to improve spinal stability, compressive resistance and
anti-bending, -shearing and -rotation abilities.
Numerous studies that aimed to prevent postoperative
epidural adhesion, such as by the use of adipose tissue, amniotic
membranes, silicon films and silicon rubber sheets, and hormone and
anti-inflammatory drug instillation, have not been successful
(11,12,24–26).
However, we propose that the vertebral plate is an effective and
safe isolation method that prevents scar adhesion in lamina
replantation fixation.
A previous study revealed that supra- and
interspinal ligaments were well innervated, and that this
innervation may form the basis of neurological feedback mechanisms
for the protection and stability of the spine (27). Studies by Hotta (28) and Newman (29) demonstrated the importance of the
supraand interspinal ligaments in the enhancement of spinal flexion
stability. In addition, Sano et al (30) and Joson et al (31) proposed methods of conserving the
supraspinous ligament during laminectomy. Hirofuji et al
(32) suggested reconstruction of
the supra- and interspinous ligaments using artificial ligaments.
In the present study, unilateral supra- and interspinous ligaments
were cut, reversely rotated with the spinous process and the
lamina, and repaired with PDS II absorbable sutures following tumor
removal and lamina replantation.
Lamina replantation with ARCH plate fixation and
ligament repair were adopted in the current study, as the technique
allows for smaller surgical incisions, allows bone protecting the
spinal cord to be conserved, prevents spinal instability and
kyphosis, and preserves the spinous process during lamina
replantation, resulting in a favorable appearance. In addition, the
restoration of the ligament-nerve-muscle reflex system of the
supra- and interspinous ligaments aids lower back movement.
Furthermore, the technique prevents epidural adhesion following
laminectomy. Moreover, a second surgical procedure is then safer
and simpler, as the posterior bony structure is preserved. Lamina
replantation enables muscle and soft tissue attachment, increasing
postoperative perispinal muscle function. Additionally, the
biomechanical environment of the surgical segments is recovered,
which prevents movement loss and peripheral segment
degeneration.
Thoracolumbar laminoplasty using the posterior
approach is beneficial, as it retains the posterior spinal
structures and prevents postoperative bleeding, scar adhesions,
instability, subluxation and kyphosis. In addition, it provides
uncomplicated access when further surgery is required. Lamina
replantation with titanium plate fixation has been demonstrated to
be a favorable surgical procedure that is not limited by the
patient’s age, the surgical site or the number of impaired
segments.
Acknowledgements
This study was supported by the
Changzhou Science and Technology Bureau Project (grant no.
CJ20112017) and the key project of Changzhou city Health Bureau
(grant no. ZD201103).
References
|
1.
|
Love JG: Laminectomy for the removal of
spinal cord tumors. J Neurosurg. 25:116–121. 1966. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Wiedemayer H, Sandalcioglu IE, Aalders M,
Wiedemayer H, Floerke M and Stolke D: Reconstruction of the laminar
roof with miniplates for a posterior approach in intraspinal
surgery: technical considerations and critical evaluation of
follow-up results. Spine (Phila Pa 1976). 29:E333–E342. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Jönsson B, Annertz M, Sjöberg C and
Strömqvist B: A prospective and consecutive study of surgically
treated lumbar spinal stenosis. Part II: Five years follow-up by an
independent observer. Spine (Phila Pa 1976). 22:2938–2944.
1997.PubMed/NCBI
|
|
4.
|
Kondo E and Yamada K: Osteoplastic
laminectomy for lumbar disc protrusion. Arch Jap Chir. 23:287–294.
1954.
|
|
5.
|
Raimondi AJ, Gutierrez FA and Di Rocco C:
Laminotomy and total reconstruction of the posterior spinal arch
for spinal canal surgery in childhood. J Neurosurg. 45:555–569.
1976. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Fidler MW and Bongartz EB: Laminar removal
and replacement: a technique for the removal of epidural tumor.
Spine (Phila Pa 1976). 13:218–220. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Goel A and Deogaonkar M: Thoracic
laminoplasty using spinous processes - technical note. Neurol Med
Chir. 36:659–661. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Matsui H, Kanamori M and Miaki K:
Expansive laminoplasty for lumbar intradural lipoma. Int Orthop.
21:185–187. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Mimatsu K: New laminoplasty after thoracic
and lumbar laminectomy. J Spinal Disord. 10:20–26. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Menku A, Koc RK, Oktem IS, Tucer B and
Kurtsoy A: Laminoplasty with miniplates for posterior approach in
thoracic and lumbar intraspinal surgery. Turk Neurosurg. 20:27–32.
2010.PubMed/NCBI
|
|
11.
|
Iida Y, Kataoka O, Sho T, Sumi M, Hirose
T, Bessho Y and Kobayashi D: Postoperative lumbar spinal
instability occurring or progressing secondary to laminectomy.
Spine (Phila Pa 1976). 15:1186–1189. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Lonstein JE: Postlaminectomy spinal
deformity. Moe’s Textbook of Scoliosis and Other Spinal
Deformities. Lonstein JE, Bradford DS, Winter RB and Ogilvie JW:
3rd edition. WB Saunders; Philadelphia: pp. 506–515. 1995
|
|
13.
|
Airaksinen O, Herno A, Turunen V, Saari T
and Suomlainen O: Surgical outcome of 438 patients treated
surgically for lumbar spinal stenosis. Spine (Phila Pa 1976).
22:2278–2282. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Papagelopoulos PJ, Peterson HA, Ebersold
MJ, Emmanuel PR, Choudhury SN and Quast LM: Spinal column deformity
and instability after lumbar or thoracolumbar laminectomy for
intraspinal tumors in children and young adults. Spine (Phila Pa
1976). 22:442–451. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
Katz JN, Lipson SJ, Chang LC, Levine SA,
Fossel AH and Liang MH: Seven- to 10-year outcome of decompressive
surgery for degenerative lumbar spinal stenosis. Spine (Phila Pa
1976). 21:92–98. 1996.PubMed/NCBI
|
|
16.
|
Scholz M, Firsching R and Lanksch WR: Long
term follow-up in lumbar spinal stenosis. Spinal Cord. 36:200–204.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Mullin BB, Rea GL, Irsik R, Catton M and
Miner ME: The effect of postlaminectomy spinal instability on the
outcome of lumbar spinal stenosis patients. J Spinal Disord.
9:107–116. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Tsuji M, Kurihara A, Urtsuji Y, Shoda E
and Mizuno T: The results of surgical treatment for degenerative
spondylolisthetic stenosis. Clin Orthop Surg. 25:455–461. 1990.
|
|
19.
|
Shikata J, Yamamuro T, Shimizu K and Saito
T: Combined laminoplasty and posterolateral fusion for spinal canal
surgery in children and adolescents. Clin Orthop Relat Res.
259:92–99. 1990.PubMed/NCBI
|
|
20.
|
Lin B, Huang ZZ, Guo ZM, Liu H and Sha M:
Surgical treatment for multisegmental intraspinal tumors of the
spine. J Clin Orthop. 13:365–368. 2010.(In Chinese).
|
|
21.
|
Hara M, Takayasu M, Takagi T and Yoshida
J: En bloc laminoplasty performed with threadwire saw.
Neurosurgery. 48:235–239. 2001.PubMed/NCBI
|
|
22.
|
Kawahara N, Tomita K, Shinya Y, et al:
Recapping T-saw laminoplasty for spinal cord tumors. Spine (Phila
Pa 1976). 24:1363–1370. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
23.
|
Murakami H, Mamune N, Isaki H, Asazuma T
and Yamagishi M: A case report of giant cauda equina tumor
presented with minor symptoms. Sekituisekizui. 11:53–56. 1998.
|
|
24.
|
La Rocca H and Macnab I: The laminectomy
membrane. Studies in its evolution, characteristics, effects and
prophylaxis in dogs. J Bone Joint Surg Br. 56B:545–550.
1974.PubMed/NCBI
|
|
25.
|
Winter RB and Hall JE: Kyphosis in
childhood and adolescence. Spine (Phila Pa 1976). 3:285–308. 1978.
View Article : Google Scholar : PubMed/NCBI
|
|
26.
|
Yasuoka S, Peterson HA and MacCarty CS:
Incidence of spinal column deformity after multilevel laminectomy
in children and adults. J Neurosurg. 57:441–445. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
27.
|
Jiang H, Russell IG, Raso VJ, Moreau MJ,
Hill DL and Bagnall KM: The nature and distribution of the
innervation of human supraspinal and interspinal ligaments. Spine
(Phila Pa 1976). 20:869–876. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
28.
|
Hotta H: An experimental study on
stability of human spine, especially the role of the lumbar
ligaments. J Jpn OrthopAssoc. 50:1–14. 1976.
|
|
29.
|
Newman PH: Sprung back. J Bone Joint Surg
Br. 34B:30–37. 1952.PubMed/NCBI
|
|
30.
|
Sano S, Masuda A, Kabata K, Mitsui H and
Kunoki J: Laminectomy with spinous process reattachment -
preliminary report. Orthop Surg Traumatol. 26:1227–1230. 1983.
|
|
31.
|
Joson RM and McCormik KJ: Preservation of
the supraspinous ligament for spinal stenosis: a technical note.
Neurosurgery. 21:420–422. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
32.
|
Hirofuji E, Tanaka K and Nakano A:
Ligamentous reconstruction with artificial ligament to prevent the
unstable lumbar spine. Clin Orthop Surg. 25:501–506. 1990.
|