Introduction
In 2013, lung cancer was responsible for the
majority of cancer deaths at a rate of 37.2/100,000 men (1). Numerous treatment modalities,
including surgery, conventional radiotherapy and chemotherapy have
been used to provide local control and maximize survival time. When
non-small-cell lung cancer (NSCLC) is diagnosed early, for
medically suitable patients, the current standard of treatment is
surgical resection (2). However,
due to comorbid conditions, the majority of patients are considered
to be medically inoperable. For these patients who are medically
inoperable or unwilling to tolerate surgery, the primary option for
treatment is conventional radiotherapy with cumulative doses of ≥60
Gy which are delivered in daily fractions over six or more weeks.
However, the five-year survival rate of conventional radiation
therapy for these patients is only ~15% and the crude local failure
rates is relatively high at 19–70% (3,4).
Conventional radiation therapy is only able to improve median
overall survival by less than 21 months compared with that for
observation alone (5).
With substantial improvements in radiotherapy
technology, stereotactic body radiation therapy (SBRT) and
dose-intensification has led to promising treatment outcomes.
CyberKnife, the robotic stereotactic radiosurgery (SRS) system,
which is able to precisely deliver a high dose of radiation, has
unique advantages that make it particularly suited for the
stereotactic radiotherapy of lung tumors that move with breathing
(6). The CyberKnife system
sustains accurate and precise radiation delivery by image-guided
localization with a compact robotically positioned linear
accelerator. The high degree of automated image guidance of
CyberKnife enables the successful management of breathing-induced
motion and the dynamic tracking of treatment targets without the
use of conventional methods (respiratory manipulation and
respiratory gating); this is a critical feature that differentiates
CyberKnife from other image-guided platforms (7). High tumor control rates in NSCLCs
have previously been demonstrated using this novel technique
(8). However, the complete
response of early non-small cell lung tumors with multiple lesions
after CyberKnife therapy has been rarely discussed. We report a
case of a stage III lung tumor with 15 lesions that was inoperable
due to the advanced age of the patient. The tumor was treated with
CyberKnife radiosurgery and a successful response to the new
therapy was observed.
Case report
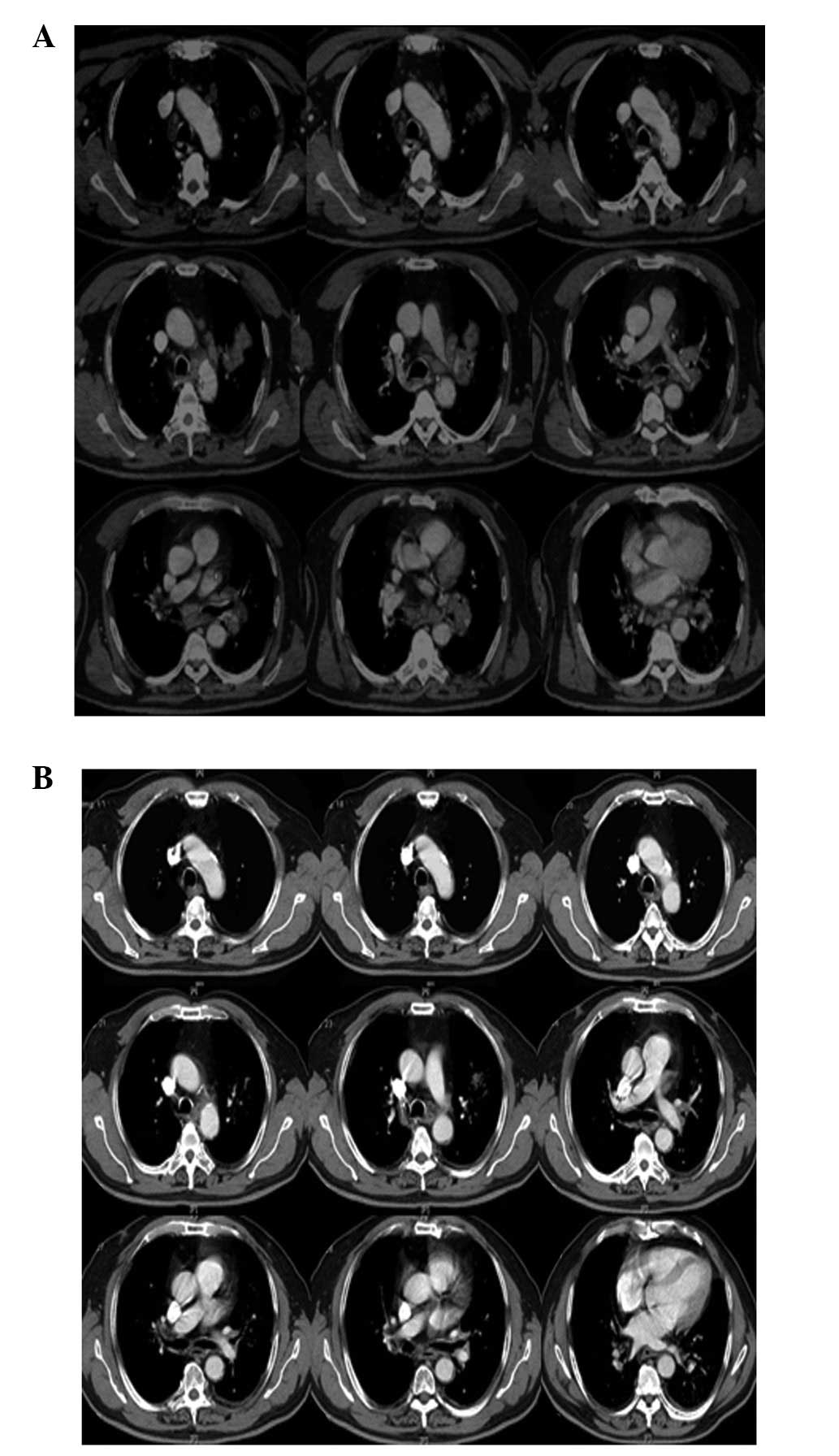
A 72-year-old male presented with paroxysmal cough,
blood-stained sputum for 1 year and syncope for 5 days prior to
hospital admission on January 28, 2011. On admission, a computed
tomography (CT) scan demonstrated a 4.4×3.5 cm ring-enhancing
lesion on superior posterior segments of the upper lobe of the left
lung with a coarse boundary and multiple swollen lymph nodes in the
mediastinum as shown in Fig. 1A.
The pathology reports confirmed the diagnosis of adenocarcinoma of
the lung. Due to the advanced age of the patient, poor body
condition and multiple tumor lesions, SRS with CyberKnife was the
selected mode of treatment.
The CyberKnife therapy was administered between
January 30 and February 17, 2011. The fiducial markers were
implanted by conventional bronchoscopy within or adjacent to tumors
to serve as targeting references. The two target areas, including
15 lesions, were treated with prescribed doses of 30 and 35 Gy,
respectively, to the gross tumor volume (GTV) in 5 fractions. The
isodose line covered 85–95% of planning tumor volume (PVT, the
precise target of cancer therapy) with 75–85% of the prescription
dose. The modified conformity index was 1.41. Clinical examination
and CT imaging were performed 42 days after the completion of
CyberKnife therapy. A follow-up lung CT scan on March 11, 2011
revealed that no evident lesions were present and the tumor had
completely disappeared (Fig. 1B).
During routine follow-up, no side-effects due to the radiation were
observed. The paroxysmal cough and blood-stained sputum were slowly
relieved. CT revealed that tumors had disappeared following
CyberKnife treatment (Fig. 1).
Written informed consent was obtained from the patient. The study
was approved by the Ethics Committee of the People’s Liberation
Army 107th Hospital affiliated to Binzhou Medical College (Yantai,
China).
Discussion
Surgical resection is the most effective treatment
for patients with early NSCLC. However, for patients who are not
able to tolerate surgery, minimally-invasive and effective
treatments are required. Among the presently existing radiation
treatments, conventional radiotherapy usually leads to severe lung
damage due to its low tolerated dose. The total dose of
conventional fractionation radiotherapy for early NSCLC is usually
45–66 Gy (9). Dose escalation is
one possible strategy for improving the local control rate and
enhancing the effect. However, when the dose in 3D conformal
radiation therapy (CRT) is increased, the radiation damage of
normal tissue is increased. In addition, in order to create a
sufficient dosage, the traditional irradiation is prolonged for l0
weeks, which leads to a reduction of local tumor control (10,11).
In 2003, Whyte et al treated primary and
transfer lung tumors (maximum diameter 1–5 cm) with CyberKnife for
the first time and confirmed the feasibility, efficacy and safety
of CyberKnife in the treatment of lung cancer (12). The CyberKnife is an image-guided,
frameless, real-time robotic radiosurgery system. The benefits of
the CyberKnife include more accurate target localization and
improved dose delivery for the management of lung tumors.
Currently, CyberKnife is widely used for inoperable early lung
cancer patients. With a high energy, large dose and narrow beam,
CyberKnife is able to focus accurately on the target. CyberKnife
treatment has contributed to the optimization of radiotherapy
dosing and scheduling, and has improved the efficacy and safety of
the radiosurgery treatment. X-rays and γ-rays are able to provide
favorable clinical curative effects, but continue to have critical
deficiencies due to fixed mounts. By contrast, CyberKnife uses an
infrared sensor to track breathing without a frame. CyberKnife is
currently the most widely used body SRS technique with controlled
synchronous movement of the light beam. Therefore, it is possible
to refrain from increasing the irradiation dose due to the mobility
of the X-ray beam around the tumor. The equipment also decreases
the unnecessary radiation damage to the surrounding normal tissue,
which significantly reduces complications. Dynamic target tracking
is an integral part of treating tumors that move with respiration
using the CyberKnife. This process requires the implantation of
metallic fiducial markers in or around the tumor for image-guided
tracking. CyberKnife achieves dynamic target tracking using a
synchronized respiratory tracking system, and therefore, eliminates
the effects of respiratory motion during the treatment process. The
implantation of metallic fiducial markers is a key procedure that
enables the CyberKnife to realize dynamic target tracking. CT with
thin cuts (1.25 mm), which produces high-resolution digitally
reconstructed radiographs for optimal position and motion
compensation, is used for target delineation and treatment planning
(13).
SRS uses multiple convergent beams to deliver a
single large dose of radiation to a discrete target volume and is
an alternative treatment for patients with advanced lung tumors
that are surgically unresectable (8). SRS has been demonstrated to be an
effective alternative and noninvasive treatment for advanced lung
tumors. Fractionated modality has been considered for the control
of larger tumors. The CyberKnife system has been shown to be
effective and feasible for use in tackling certain technical
challenges involved in these inoperable complex treatments. For
smaller, peripheral tumors, high dose radiation therapy (e.g. 60 Gy
in 3 fractions) have produced excellent local control results
(13). A median 18-month (range,
2–41 months) follow-up study observed that total doses ranging from
5 to 60 Gy delivered in one to four fractions to 35 patients with
lung cancer, achieved 71% local control and a survival rate of 77%
(14). A multicenter retrospective
study analyzed the data of 56 clinical patients treated with
CyberKnife. It was observed that the actuarial 2-year local tumor
control of patients who received a biologically effective dose
>100 Gy was 85%, and the 3-year cancer-specific survival of
NSCLC patients was 80% (15).
Additional studies are required to optimize the dose for large and
centrally located tumors.
In the present case, there was no recurrence of lung
tumors following CyberKnife therapy during the follow-up
lung-imaging studies. Following CyberKnife radiosurgery with
radiation doses of 30 Gy and 35 Gy, the two tumor target areas,
which including 15 lesions, were completely resolved within 42
days. During the routine follow-up, no side-effects were observed.
In conclusion, the image-guided SRS is particularly useful for
lesions it is not possible to treat conventionally, such as lesions
that have received the maximal radiation dose using conventional
radiotherapy or post-operative residual lesions. The complete
response of advanced lung tumors with multiple lesions may also be
achieved within a few months after CyberKnife radiosurgery, as
shown by the current case study. Despite encouraging preliminary
results, longer term follow-up and further clinical trials are
required.
Acknowledgements
This study was supported by grants from the National
Special Issue of the Ministry of Health of China (no.
2009BX042).
References
|
1
|
Malvezzi M, Bertuccio P, Levi F, La
Vecchia C and Negri E: European cancer mortality predictions for
the year 2013. Ann Oncol. 24:792–800. 2013.PubMed/NCBI
|
|
2
|
Swangsilpa T, Yongvithisatid P, Pairat K,
Dechsupa P, Dhanachai M, Dangprasert S, Narkwong L, Sitathanee C,
Puataweepong P, Puddhikarant P, Jiarpinitnun C, Witoonpanich P,
Ukhumpun T and Khaophong J: Preliminary experience of CyberKnife
treatment of primary non-small cell lung cancer. J Med Assoc Thai.
95:1335–1343. 2012.PubMed/NCBI
|
|
3
|
Goldsmith C and Gaya A: Stereotactic
ablative body radiotherapy (SABR) for primary and secondary lung
tumours. Cancer Imaging. 12:351–60. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Qiao X, Tullgren O, Lax I, Sirzén F and
Lewensohn R: The role of radiotherapy in treatment of stage I
non-small cell lung cancer. Lung Cancer. 41:1–11. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Wisnivesky JP, Bonomi M, Henschke C,
Iannuzzi M and McGinn T: Radiation therapy for the treatment of
unresected stage I-II non-small cell lung cancer. Chest.
128:1461–7. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hong JC, Yu Y, Rao AK, Dieterich S, Maxim
PG, Le QT, Diehn M, Sze DY, Kothary N and Loo BW Jr: High retention
and safety of percutaneously implanted endovascular embolization
coils as fiducial markers for image-guided stereotactic ablative
radiotherapy of pulmonary tumors. Int J Radiat Oncol Biol Phys.
81:85–90. 2011. View Article : Google Scholar
|
|
7
|
Brown WT, Wu X, Fayad F, Fowler JF,
Amendola BE, García S, Han H, de la Zerda A, Bossart E, Huang Z and
Schwade JG: CyberKnife radiosurgery for stage I lung cancer:
results at 36 months. Clin Lung Cancer. 8:488–492. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Wang YY, Wang YS, Liu T, Yang K, Yang GQ,
Liu HC, Wang SS and Yang JL: Efficacy study of CyberKnife
stereotactic radiosurgery combined with CIK cell immunotherapy for
advanced refractory lung cancer. Exp Ther Med. 5:453–456.
2013.PubMed/NCBI
|
|
9
|
Kaskowitz L, Graham MV, Emami B, Halverson
KJ and Rush C: Radiation therapy alone for stage I non-small cell
lung cancer. Int J Radiat Oncol Biol Phys. 27:517–523. 1993.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Dosoretz DE, Katin MJ, Blitzer PH,
Rubenstein JH, Salenius S, Rashid M, Dosani RA, Mestas G, Siegel AD
and Chadha TT: Radiation therapy in the management of medically
inoperable carcinoma of the lung: results and implications for
future treatment strategies. Int J Radiat Oncol Biol Phys. 24:3–9.
1992. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Timmerman RD, Kavanagh BD, Cho LC, Papiez
L and Xing L: Stereotactic body radiation therapy in multiple organ
sites. J Clin Oncol. 25:947–52. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Whyte RI, Crownover R, Mushy MJ, et al:
Stereotactic radiosurgery for lung tumors: preliminary report of a
phase 1 trial. Ann Thorac Surg. 75:1097–1101. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Gibbs IC and Loo BW Jr: CyberKnife
stereotactic ablative radiotherapy for lung tumors. Technol Cancer
Res Treat. 9:589–596. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Brown WT, Wu X, Fowler JF, García S, Fayad
F, Amendola BE, de la Zerda A and Schwade JG: Lung metastases
treated by CyberKnife image-guided robotic stereotactic
radiosurgery at 41 months. South Med J. 101:376–82. 2008.
View Article : Google Scholar
|
|
15
|
Nuyttens JJ, van der Voort van Zyp NC,
Praag J, Aluwini S, van Klaveren RJ, Verhoef C, Pattynama PM and
Hoogeman MS: Outcome of four-dimensional stereotactic radiotherapy
for centrally located lung tumors. Radiother Oncol. 102:383–387.
2012. View Article : Google Scholar : PubMed/NCBI
|