Introduction
Heart failure is one of the most serious diseases in
children, and is characterized by a progressive left ventricular
pump dysfunction, leading to cardiac dilatation, thinned walls and
poor contractility (1). Following
numerous investigations, pediatric heart failure has been redefined
as a progressive clinical and pathophysiological syndrome that
occurs due to cardiovascular and non-cardiovascular abnormalities.
These abnormalities result in the characteristic signs and symptoms
of the disease, including edema, respiratory distress, growth
failure and exercise intolerance, accompanied by circulatory,
neurohormonal and molecular disturbances. Cardiomyopathies and
congenital heart disease are the most common causes, and lead to
acute and chronic heart failure, respectively (2–4).
The diagnostic measures of pediatric heart failure
include the Ross criteria (5),
modified Ross criteria (6,7) and the New York University Pediatric
Heart Failure Index (NYU PHFI) (8). Amino-terminal pro-brain natriuretic
peptide (NT-proBNP) is a sensitive biomarker of heart failure, and
is able to improve the accuracy of diagnosis (9–12).
Serum NT-proBNP levels may be used to assist in the differentiation
between dyspnea resulting from respiratory problems and heart
failure (13), and have been
demonstrated to correlate with the severity of left ventricular
(LV) dysfunction and functional status (14). In addition, serum NT-proBNP levels
have been revealed to be predictive of morbidity and mortality
(15), and may be used in the
selection of the therapeutic modality (16). Despite several studies
demonstrating the significance of NT-proBNP as a biomarker for
heart failure, its measurement is not commonly involved in the
routine testing performed in children with cardiac disease, due to
the fact that little is known about its function, accuracy and
validity as a diagnostic test in children (17). The purpose of the current study was
to determine whether plasma NT-proBNP levels in combination with a
modified Ross criteria score constitute suitable diagnostic
criteria for heart failure in children.
Materials and methods
Study population
A total of 240 children were involved in this study.
These included 80 children with heart failure, who were admitted to
the Women and Children’s Health Care Hospital of Shunde (Shunde,
China) from March 2010 to January 2012, 80 children with
non-cardiogenic dyspnea and 80 healthy children. The diagnosis of
pediatric heart failure was made based on the modified Ross
criteria (6,7). Among the 80 children with heart
failure there were 43 males and 37 females, and the average age was
9.5 months (range, 1–18 months). Out of these 80, 36 had acute and
44 had chronic heart failure. Acute heart failure was caused by
pneumonia in 22 children, shock in eight, myocarditis in two,
cardiomyopathy in two, pericardial effusion in one and left atrial
tumor complicated by cardiac tamponade syndrome in one. Chronic
heart failure was due to a variety of congenital heart diseases,
including ventricular septal defect in 22 children, atrial septal
defect in nine, Fallot’s syndrome in five, aortic stenosis in two,
patent ductus arteriosus in four and single-ventricle defects in
two. Among the 80 children with non-cardiogenic dyspnea there were
43 males and 37 females, and the average age was 10.5 months
(range, 1–20 months). The causes of the non-cardiogenic dyspnea
were pneumonia in 73 children, chronic anemia in four, pleural
effusion in two and congenital spina bifida combined with bulbar
myelitis in one. The 80 healthy children included 40 males and 40
females, with an average age of 8.5 months (range, 1–16 months).
The three groups had no significant differences with respect to age
or gender (P>0.05 for each). Informed consent was obtained from
each patient. The study was approved by the Ethics Committee of the
The Women and Children’s Health Care Hospital of Shunde, Shunde,
China.
NT-ProBNP level assay
Prior to and following treatment, 2 ml whole blood
was obtained from each child and stored in a fluid tube containing
EDTA. Following this, 0.75 ml blood was aliquoted to a tube
containing NT-proBNP quantitative buffer, and was mixed thoroughly.
The NT-proBNP level was assayed within 5 min by the Canadian RAMP
heart failure diagnostic instrument method. The testing materials
were provided by the Response Biomedical Corp. (Vancouver, BC,
Canada). The normal adult range of NT-proBNP is 0–300 ng/l, and a
value of ≥450 ng/l is suggestive of heart failure. At present,
there are no clear standards and there is no normal range for
children.
Data analysis
A receiver operating characteristic (ROC) curve was
created, and the cut-off score for heart failure, based on the
modified Ross criteria, and the diagnostic cut-off level for plasma
NT-proBNP in pediatric heart failure were determined by analyzing
the specificity and sensitivity of the diagnosis. The number of
children with an elevated NT-ProBNP level in the heart failure
group was compared with the number diagnosed with heart failure
according to the modified Ross criteria. A coincidence rate was
obtained by using the following formula: (Nhigh
NT-ProBNP/Nheart failure) × 100. The data were
analyzed using the F-test, and statistical analyses were performed
using SPSS version 13.0 statistical software (SPSS, Inc., Chicago,
IL, USA). P< 0.05 was considered to indicate a statistically
significant difference.
Results
Analysis of the cut-off score for heart
failure in the modified Ross criteria
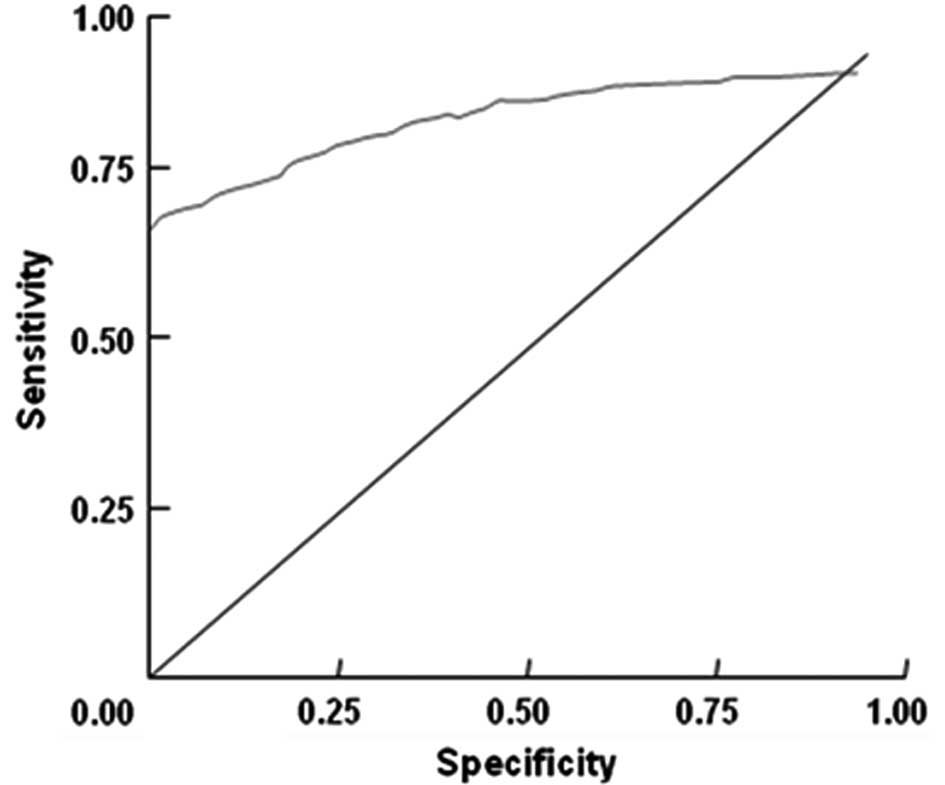
The ROC area under the curve (AUC) of heart failure
in the modified Ross criteria was 0.958 [95% confidence interval
(CI), 0.942–0.993] (Fig. 1). A
diagnostic score of ≥4, according to the ROC curve, exhibited the
highest sensitivity and specificity for heart failure (Table I). However, it was observed that
the specificity and sensitivity were relatively low when the
diagnostic cut-off was ≥3 in the Ross criteria, which readily led
to misdiagnosis.
 | Table I.Sensitivity and specificity of heart
failure diagnosis based on different Ross scores. |
Table I.
Sensitivity and specificity of heart
failure diagnosis based on different Ross scores.
| Ross score | Sensitivity | Specificity | Sensitivity +
specificity | Sensitivity +
specificity −1 |
|---|
| 0.0 | 1.000 | 0.000 | 1.000 | 0.000 |
| 2.0 | 0.823 | 0.625 | 1.448 | 0.448 |
| 3.0 | 0.886 | 0.798 | 1.684 | 0.684 |
| 4.0 | 0.908 | 0.952 | 1.860 | 0.860 |
| 5.0 | 0.902 | 0.957 | 1.819 | 0.819 |
| 6.0 | 0.906 | 0.936 | 1.842 | 0.842 |
| 7.0 | 0.802 | 1.000 | 1.802 | 0.802 |
| 8.0 | 0.887 | 0.958 | 1.845 | 0.845 |
Analysis of the diagnostic cut-off level
for plasma NT-proBNP in pediatric heart failure
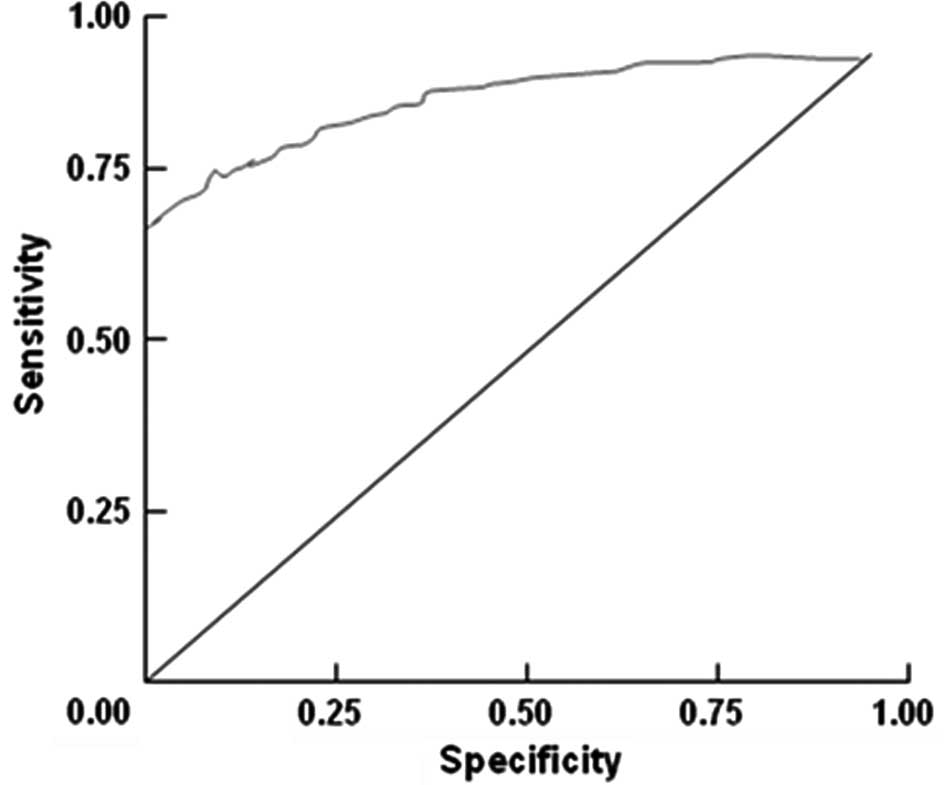
The ROC AUC of plasma NT-proBNP level in pediatric
heart failure was 0.979 (95% CI, 0.948–0.994; Fig. 2). Based on the ROC curve, a value
of ≥598 ng/l was selected as the diagnostic cut-off, as it
exhibited a high sensitivity and specificity for a diagnosis of
pediatric heart failure.
Correlation between a high NT-proBNP
level and a diagnosis of heart failure, according to the modified
Ross criteria
It was observed that the NT-ProBNP level in 76 of
the 80 children in the heart failure group was >598 ng/l. The
correlation with the modified Ross criteria was 95%.
Correlation analysis between the
NT-proBNP level in mild, moderate or severe heart failure and the
modified Ross criteria
The NT-proBNP levels used in the present study to
assess mild (41 cases), moderate (27 cases) and severe heart
failure (12 cases), which were diagnosed according to the modified
Ross criteria, were 1,184.31 (95% CI, 716.61–2,935.35), 3,353.57
(95% CI, 3,008.83–3,699.25) and 16,883.22 (95% CI,
5,718.77–5,000.32 ng/l), respectively. There was no overlap in the
95% CIs (Table II).
 | Table II.Comparison of plasma NT-proBNP levels
and modified Ross criteria scores in mild, moderate and severe
heart failure. |
Table II.
Comparison of plasma NT-proBNP levels
and modified Ross criteria scores in mild, moderate and severe
heart failure.
| Heart failure | n | NT-ProBNP level
(ng/l)
|
|---|
| 406.98–576.05 | 614.38–2935.35 | 3004.17–3699.25 | 5718.77–35000.32 |
|---|
| Mild | 41 | 491.52 (4) | 1774.87 (37) | 0 (0) | 0 (0) |
| Moderate | 27 | 0 (0) | 0 (0) | 3351.71 (27) | 0 (0) |
| Severe | 12 | 0 (0) | 0 (0) | 0 (0) | 20359.55 (12) |
The F-test revealed that there were significant
differences in the NT-proBNP levels among the mild, moderate and
severe heart failure groups [F=29.74, P=0.000 (P<0.001)]
(Table III). The plasma NT-proBNP
level increased with increasing severity of heart failure
[correlation coefficient r= 0.675, P=0.000 (P<0.001)].
 | Table III.Median amino-terminal pro-brain
natriuretic peptide (NT-proBNP) levels in the three study
groups. |
Table III.
Median amino-terminal pro-brain
natriuretic peptide (NT-proBNP) levels in the three study
groups.
| Group | n | NT-proBNP level
(ng/l) | F-statistic | P-value |
|---|
| Heart failure | 80 | 17703.65 | - | - |
| Non-cardiogenic
dyspnea | 80 | 210.23 | - | - |
| Healthy | 80 | 214.27 | 13.65 | 0.000 |
Comparison between the NT-proBNP level in
the heart failure, non-cardiogenic dyspnea and healthy groups
The F-test revealed that the NT-ProBNP levels in the
group with heart failure, the group with non-cardiogenic dyspnea
and the group of healthy children were significantly different
[F=14.90, P=0.000 (P<0.001)] (Table
III). The NT-ProBNP level in the heart failure group was
significantly higher than that in the other two groups (P= 0.001
for each). There was no significant difference between the
NT-ProBNP levels of the group with non-cardiogenic dyspnea and the
group of healthy children (P=0.097).
Combined diagnostic criteria for
pediatric heart failure
The results of the study indicate that the NT-ProBNP
level is a sensitive and reliable biomarker for the diagnosis of
heart failure, and is highly correlated with the modified Ross
criteria. Analysis of the ROC curve revealed that a score of ≥4 in
the modified Ross criteria was notably more effective than a score
of ≥3 for the diagnosis of pediatric heart failure. Furthermore,
the accuracy of the diagnosis greatly improved when the plasma
NT-proBNP level was set at ≥598 ng/l. Based on these data, we
designed combined diagnostic criteria for heart failure (Table IV) and suggest that the score
ranges for non-heart failure and mild, moderate and severe heart
failure be set at 0–4, 5–8, 9–12, and 13–15, respectively.
 | Table IV.Scoring method for a novel combined
diagnostic criteria for heart failure. |
Table IV.
Scoring method for a novel combined
diagnostic criteria for heart failure.
| Item | 0 score | +1 score | +2 score | +3 score |
|---|
| Sweating | Head only | Head and torso during
activities | Head and torso at
rest | |
| Shortness of
breath | Absent | Present during
activities | Present at rest | |
| Concave disorder | Absent | Present-mild | Present-severe | |
| Respiration rate
(breaths/min) | | | | |
| 0–1 years of
age | <50 | 50–60 | >60 | |
| 2–6 years of
age | <35 | 35–45 | >45 | |
| 7–10 years of
age | <25 | 25–35 | >35 | |
| 11–14 years of
age | <18 | 18–28 | >28 | |
| Heart rate
(beats/min) | | | | |
| 0–1 years of
age | <160 | 160–170 | >170 | |
| 2–6 years of
age | <105 | 105–115 | >115 | |
| 7–10 years of
age | <90 | 90–100 | >100 | |
| 11–14 years of
age | <80 | 80–90 | >90 | |
| Liver enlargement
(cm) | <2 | 2–3 | >3 | |
| NT-ProBNP index | <598 | 598–3000 | >3000–5000 | >5000 |
Discussion
The importance of the NT-proBNP level in the
diagnosis and evaluation of heart failure has been widely accepted
(9–11). BNP acts on several organs and
facilitates sodium transfer, increases urine production, dilates
vessels and inhibits the renin-angiotensin-aldosterone system and
sympathetic nerves. The NT-proBNP level has been observed to
increase with the abnormally high intraventricular pressure that is
associated with heart failure (9),
and the level is positively correlated with the severity of heart
failure. The possibility of heart failure is low when the NT-proBNP
level is <400 ng/l, with a negative predictive value of ∼90%.
However, heart failure is likely when the level is >450 ng/l,
when the positive predictive value is also ∼90% (12). The results of the current study
indicate that a NT-proBNP level >598 ng/l was predictive of a
diagnosis of pediatric heart failure. In the current study, an
increased NT-proBNP level was present in 95% of the 80 children who
were diagnosed with heart failure according to the modified Ross
criteria. Moreover, there were also significant differences in the
NT-proBNP levels among cases of mild, moderate and severe heart
failure.
The commonly utilized criteria of heart failure
include the international Ross criteria, the modified Ross criteria
and the NYU PHFI score. All of these, with the exception of the NYU
PHFI score, are based on clinical signs and symptoms. In 1987,
based on the classification of heart failure for adults, designed
by the New York Heart Association, Ross proposed a novel pediatric
classification for babies aged <6 months (5). This was subsequently modified by
Reithmann et al (6) and
Läer et al (7) to be
suitable for children between 0 and 14 years of age, and is
currently widely used in the diagnosis of pediatric heart failure
(18). Although the modified Ross
criteria are widely applied, they are based on clinical symptoms
and signs, and possess a certain degree of subjectivity. Therefore,
the diagnosis is likely to have an enhanced accuracy and
sensitivity with the addition of an objective diagnostic parameter
to the criteria. It was observed in the present study that the rate
of misdiagnosis was high when a modified Ross criteria score of ≥3
was used as the diagnostic cut-off. By analyzing the specificity
and sensitivity of the ROC curve, it was revealed that a score of
≥4 demonstrated an enhanced efficacy for the diagnosis of pediatric
heart failure.
Aside from the score parameters in the modified Ross
criteria, the NYU PHFI score (8)
also includes the results of echocardiography and chest radiography
examinations, and scores for drug therapy. Although the NYU PHFI
score is more sensitive and specific than the modified Ross
criteria, it is not commonly used. This is because the score
involves a large number of parameters, and certain parameters are
particularly complicated.
The combined diagnostic criteria for heart failure
proposed in the present study were based on the modified Ross
criteria, and introduced an objective diagnostic parameter, the
NT-proBNP level. The results of this study demonstrated that the
diagnosis of pediatric heart failure according to the modified Ross
criteria and the NT-proBNP level was 95% accurate. It was observed
that ∼93% of children with mild and 100% of children with severe
heart failure were included in the 95% CI. In addition, there was
no overlap in the 95% CIs of mild, moderate and severe heart
failure, and the NT-proBNP level was observed to increase with
increasing modified Ross criteria scores. Therefore, the modified
Ross criteria and the NT-proBNP level were included in the combined
diagnostic criteria for heart failure, in order to achieve a
greater accuracy of diagnosis. Moreover, the measurement of the
NT-proBNP level is easy, fast, accurate and inexpensive.
Acknowledgements
This study was supported by the
Department of Science and Technology of Guangdong, and the Bureau
of Science and Technology of Foshan, China.
References
|
1.
|
Mann DL and Bristow MR: Mechanisms and
models in heart failure: the biomechanical model and beyond.
Circulation. 111:2837–2849. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Massin MM, Astadicko I and Dessy H:
Epidemiology of heart failure in a tertiary pediatric center. Clin
Cardiol. 31:388–391. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Lipshultz SE, Sleeper LA, Towbin JA, et
al: The incidence of pediatric cardiomyopathy in two regions of the
United States. N Engl J Med. 348:1647–1655. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Nugent AW, Daubeney PE, Chondros P, et al:
The epidemiology of childhood cardiomyopathy in Australia. N Engl J
Med. 348:1639–1646. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Ross RD, Bollinger RO and Pinsky WW:
Grading the severity of congestive heart failure in infants.
Pediatr Cardiol. 13:72–75. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Reithmann C, Reber D, Kozlik-Feldmann R,
et al: A post-receptor defect of adenylyl cyclase in severely
failing myocardium from chidren with congenital heart disease. Eur
J Pharmacol. 330:79–86. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Läer S, Mir TS, Behn F, et al: Carvedilol
therapy in pediatric patients with congestive heart failure: a
study investigating clinical and pharmacokinetic parameters. Am
Heart J. 143:916–922. 2002.PubMed/NCBI
|
|
8.
|
Connolly D, Rutkowski M, Auslender M and
Artman M: The New York University Pediatric Heart Failure Index: a
new method of quantifying chronic heart failure severity in
children. J Pediatr. 138:644–648. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Rusconi P, Ludwig DA, Ratnasamy C, et al:
Serial measurements of serum NT-proBNP as markers of left
ventricular systolic function and remodeling in children with heart
failure. Am Heart J. 160:776–783. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Xue Y, Chan J, Sakariya S and Maisel A:
Biomarker-guided treatment of congestive heart failure. Congest
Heart Fail. 16(Suppl 1): S62–S67. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Haapio M, House AA, de Cal M, et al:
Heart-kidney biomarkers in patients undergoing cardiac stress
testing. Int J Nephrol. 2011:4259232011.PubMed/NCBI
|
|
12.
|
Sugimoto M, Manabe H, Nakau K, et al: The
role of N-terminal pro-B-type natriuretic peptide in the diagnosis
of congestive heart failure in children. Correlation with the heart
failure score and comparison with B-type natriuretic peptide. Circ
J. 74:998–1005. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Maisel AS, Krishnaswamy P, Nowak RM, et al
Breathing Not Properly Multinational Study Investigators: Rapid
measurement of B-type natriuretic peptide in the emergency
diagnosis of heart failure. N Engl J Med. 347:161–167. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Richards AM, Nicholls MG, Espiner EA, et
al: B-type natriuretic peptides and ejection fraction for prognosis
after myocardial infarction. Circulation. 107:2786–2792. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
Stanton E, Hansen M, Wijeysundera HC, et
al PRAISE-2 study investigators: A direct comparison of the
natriuretic peptides and their relationship to survival in chronic
heart failure of a presumed non-ischaemic origin. Eur J Heart Fail.
7:557–565. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Jourdain P, Jondeau G, Funck F, et al:
Plasma brain natriuretic peptide-guided therapy to improve outcome
in heart failure: the STARS-BNP Multicenter Study. J Am Coll
Cardiol. 49:1733–1739. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Law YM, Hoyer AW, Reller MD and Silberbach
M: Accuracy of plasma B-type natriuretic peptide to diagnose
significant cardiovascular disease in children: the Better Not Pout
Children! Study. J Am Coll Cardiol. 54:1467–1475. 2009.PubMed/NCBI
|
|
18.
|
Di Serio F, Ruggieri V, Varraso L, De
Sario R, Mastrorilli A and Pansini N: Analytical evaluation of the
Dade Behring Dimension RxL automated N-terminal proBNP (NT-proBNP)
method and comparison with the Roche Elecsys 2010. Clin Chem Lab
Med. 43:1263–1273. 2005.PubMed/NCBI
|