Introduction
An aneurysmal bone cyst (ABC) is a rare skeletal
tumor that accounts for ~1% of all bone tumors. A spinal location
for an ABC is extremely rare. Fibrohistiocytoma is a type of
primary benign bone tumor, which is composed of fusiform
fibroblasts (1,2). It is a rare bone tumor, whose
predilection site is the pelvis. They are more common in male
patients. The combination of two primary bone benign tumors is
quite rare in the clinic. From a diagnostic standpoint,
fibrohistiocytoma and ABCs are widely confused with other
giant-cell-containing tumors of the bone. Among such tumors,
telangiectatic osteosarcoma is widely confused with ABCs,
radiologically and pathologically, and there have been reports of
telangiectatic osteosarcoma that were initially treated as ABCs
with a fatal outcome (3).
Therefore, the differential diagnosis between the two diseases
should be conducted even more cautiously to prevent
misdiagnosis.
Case report
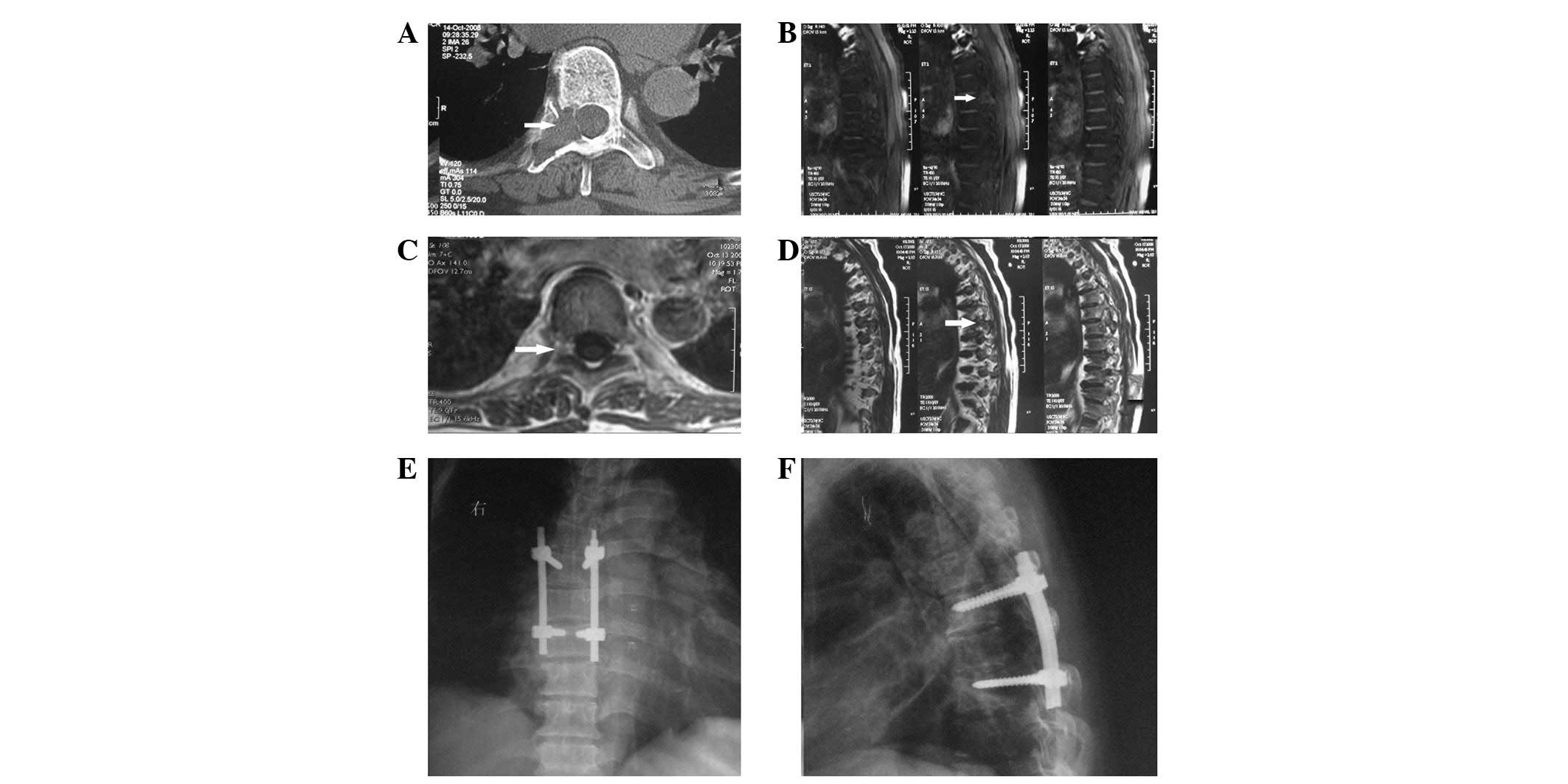
A 63-year-old female complained of back pain, and
numbness and weakness in the lower limbs. Computerized tomography
(CT) and magnetic resonance imaging (MRI) (Fig. 1A–D) revealed an expansive, lytic
and unicameral cyst lesion localized at the pedicle and transverse
process of T7. A nuclide bone scan revealed multiple nuclide
aggregation in the costal bone and body of the vertebra. It was
considered that the patient suffered from a metastatic tumor.
However, after a thorough general examination, no sign of a primary
tumor was identified. Then, the patient underwent a positron
emission tomography (PET)-CT scan. Expansive osteoclasia was
observed in the right appendix of T7, similar to a giant cell tumor
of bone. Since the patient had rheumatic heart disease for ~10
years, heart ultrasound (heart shadow enlargement with back flow)
was performed to evaluate heart function (grade II), to ensure the
patient was able to endure surgery. Based on the clinical and
diagnostic imaging findings, plans were made to treat the lesion
with resection. Informed consent was obtained from the patient
regularly. Prior to surgery, a puncture biopsy was performed, which
resulted in the formation of scar tissue. Surgery was subsequently
performed with the use of a general anesthetic, with the patient in
the prone position. The tumor was resected and electrocautery was
used following resection to prevent recurrence. Following
excisional biopsy, segmental instrumented posterior fusion was
performed from T6 to T8 (Fig. 1E and
F). The surgery lasted for ~2.5 h. The blood loss was ~600 ml
and 2 U red blood cells were transfused intraoperatively to
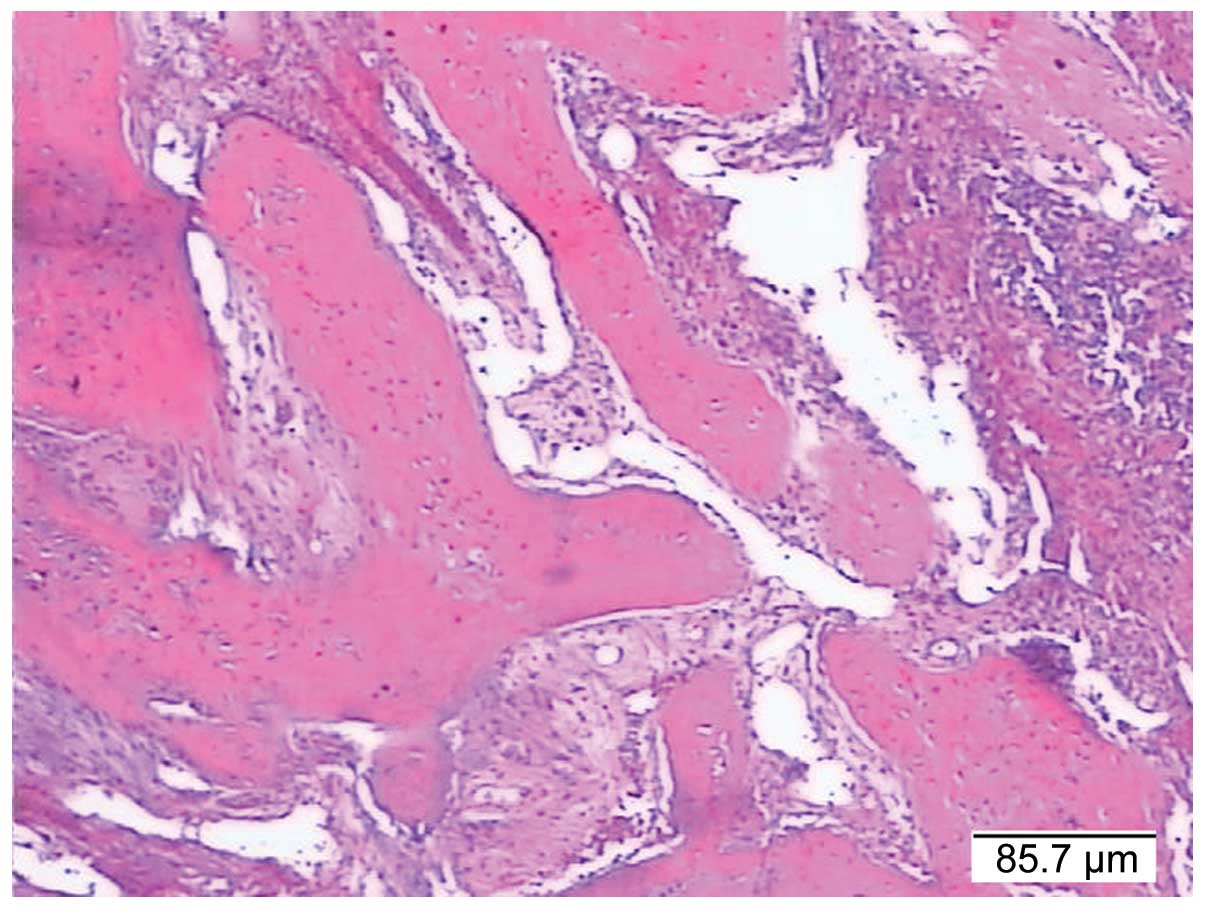
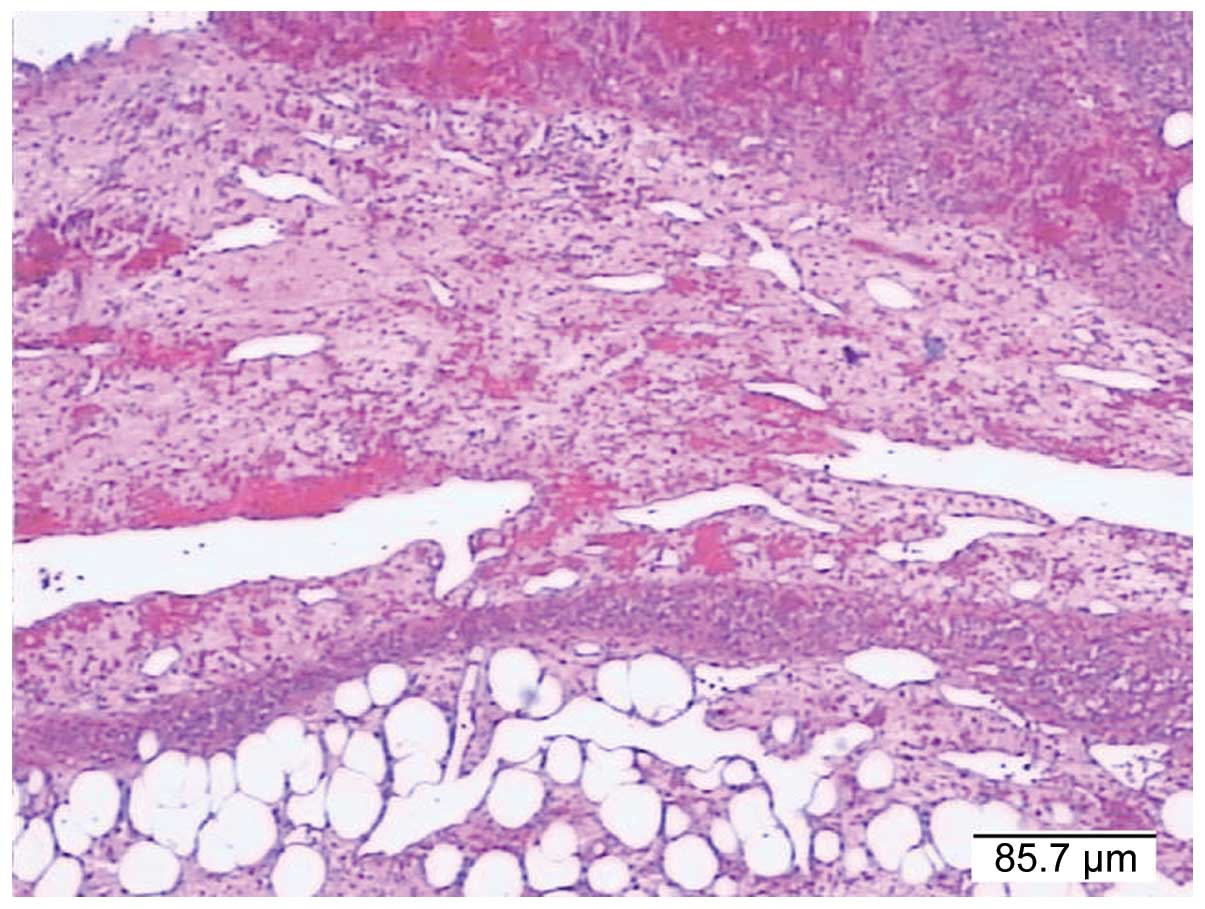
maintain the normal blood volume. The pathological diagnosis was
fibrohistiocytoma combined with an ABC (Figs. 2 and 3). Immunohistochemical analysis was
negative for cytokeratin (CK), epithelial membrane antigen (EMA),
CD34, CD31, desmin (Des), smooth muscle actin (SMA), HMB45,
phosphoglucomutase 1 (PGM1) and S-100. The patient was followed-up
for >2 years. The bone grafts had been incorporated and the
patient was fully rehabilitated and free of any symptoms. Finally,
the patient succumbed 5 years after surgery from epilepsy.
Discussion
ABCs are benign, highly vascular osseous lesions
characterized by cystic, blood-filled spaces surrounded by thin
perimeters of expanded bone. The precise pathogenesis of ABC is
unclear, although theories such as post-traumatic boney alteration,
reactive vascular malformation and genetic predisposition have been
described. The most widely accepted pathogenic mechanism for the
development of ABC involves a hypothetical local circulatory
disturbance that leads to markedly increased venous pressure and
the development of dilated and enlarged vascular elements within
the affected bone (3).
Fibrohistiocytoma is a type of primary benign bone
tumor, which is composed of fusiform fibroblasts accompanied by
multinucleated osteoclast-like giant cells, cystose cells and
chronic inflammatory cell infiltration. There is also likely to be
interstitial substance hemorrhage and hemosiderin deposition. It is
a rare bone tumor and the predilection site is the pelvis. It is
more common in male patients (4).
A combined lesion of two primary benign bone tumors
is quite rare in the clinic (3).
From a diagnostic standpoint, both fibrohistiocytoma and ABC are
widely confused with other giant-cell-containing tumors of bone
(3). Giant cell tumor (GCT), for
instance, is composed of mononuclear cells and osteoclast-like
multinucleated giant cells, with the potential to be locally
aggressive. Histologically, a GCT consists of homogeneous stroma
with giant and mononuclear cells dispersed evenly throughout the
tumor. Giant cell reparative granuloma (GCRG) is an uncommon,
benign, intraosseous reactive lesion for which the roentgenographic
and histological features may overlap with ABCs. Brown tumors or
von Recklinghausen’s disease typically involve the diaphysis of
long bones. The incidence of brown tumors is reported to be
1.5–1.7% of patients with chronic renal deficiency. The
radiographic and histological features of brown tumors, ABCs and
GCRG are often indistinguishable (3). However, brown tumors were recently
reported to have a much more oblated architectural growth pattern
in comparison with ABC and GCRG. Hyperparathyroidism may be ruled
out on the basis of serum calcium, phosphorus and parathyroid
hormone levels.
Telangiectatic osteosarcoma is primarily composed of
multiple dilated multi-cameral capsular cavities that contain
blood, with viable high-grade sarcomatous cells in the peripheral
rim and septae around these spaces. Hence, the lesion is widely
confused with ABCs, radiologically and pathologically, and there
have been reports of telangiectatic osteosarcomas that were
initially treated as ABCs with a fatal outcome. Radiographic
distinction between these lesions is challenging (3). However, the nodular viable high-grade
sarcomatous cells that produce osteoid around these cystic spaces
are demarcated following the administration of contrast material.
The lesion appears as a solid, thick, nodular-enhancing rim of
tissue that contains subtle mineralization when viewed with
radiographs or CT images.
Grossly, an ABC is multiloculated, consisting of
multiple blood-filled cystic spaces separated by thin, tan-white
areas that may represent a solid portion of the ABC or a primary
lesion, if present. Histologically, an ABC is composed of
blood-filled cystic spaces separated by fibrous septae.
Methods for the treatment of an ABC include
resection, curettage, embolization and intralesional injection of a
variety of agents. In the current study, we present a female
patient with thoracic spinal pain, with progressive paresthesias
and muscle weakness of the lower extremities. This case highlights
the importance of considering an ABC in the differential diagnosis
of primary spinal tumors. The differential diagnosis for this
lesion may be challenging, particularly with regard to the
possibility of the presence of osteoid osteoma, osteoblastoma, ABC,
osteochondroma, neurofibroma, eosinophilic granuloma, hemangioma
and other giant-cell-containing tumors of bone, including GCT,
GCRG, brown tumor of hyperparathyroidism and telangiectatic
osteosarcoma. The evaluation of spinal tumors includes a thorough
history assessment, physical examination, imaging and,
occasionally, laboratory evaluation and biopsy when indicated
(1).
Depending on the analysis of radiographic
morphology, location and the age of the patient with ABC and GCT
(5), the following criteria
suggest an ABC with a high positive predictive value: location in
the diaphysis and shaft, patient aged <17 years and growth rate
grade Lodwick-IA. GCT was selected via the following criteria:
epimetaphyseal location and growth rate grade Lodwick-II. However,
in certain cases, differential diagnosis between the two entities
is radiologically impossible.
In patients who develop a bone tumor of the
posterior elements of the spine, careful clinical and radiological
evaluation is necessary to narrow the differential diagnosis.
Treatment options for ABCs are simple curettage with or without
bone grafting, complete excision, embolization, radiation therapy
or a combination of these modalities. Embolization appears to be
the first option for spinal ABC treatment due to having the best
cost-to-benefit ratio. An intact ABC is indicated when no
pathological fracture or neurological involvements are observed
(2). New therapies have recently
been reported. Denosumab is a human monoclonal antibody that
inhibits osteoclast function by blocking the cytokine receptor
activator of the nuclear factor-κB ligand. Satisfactory results
with denosumab in treating GCTs and immunohistochemical
similarities suggest that it may also have positive effects on ABCs
(6). Nevertheless, radical
surgical excision should be the goal of surgery to reduce the
recurrence rate. The recurrence rate is significantly lower in
cases of total excision (7). In
the majority of cases, a complete excision should be performed if
possible. The risk of postlaminectomy kyphosis is high. As such, a
fusion should be considered whenever a laminectomy is performed
(8,9). Prompt detection and treatment with
curettage, decompression and fusion produces a satisfactory result
and prevents spinal cord injury (10). ABCs are hypervascularized lesions.
Pre-operative selective arterial embolization of the lesion may
have some value (11). Selective
arterial embolization should be used as a preoperative adjunct to
surgery for ABC of the spine to reduce intraoperative blood loss
and the need for blood transfusions. Spinal fusion with titanium
instruments (12) is strongly
recommended if more than two facets (more than one on each side, or
more than two full facets) are violated during the excision of the
ABC.
References
|
1.
|
Thakur NA, Daniels AH, Schiller J, Valdes
MA, Czerwein JK, Schiller A, Esmende S and Terek RM: Benign tumors
of the spine. J Am Acad Orthop Surg. 20:715–724. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Amendola L, Simonetti L, Simoes CE,
Bandiera S, De Iure F and Boriani S: Aneurysmal bone cyst of the
mobile spine: the therapeutic role of embolization. Eur Spine J.
22:533–541. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Iltar S, Alemdaroğlu KB, Karalezli N,
Irgit K, Caydere M and Aydoğan NH: A case of an aneurysmal bone
cyst of a metatarsal: review of the differential diagnosis and
treatment options. J Foot Ankle Surg. 48:74–79. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Macdonald D, Fornasier V and Holtby R:
Benign fibrohistiocytoma (xanthomatous variant) of the acromion. A
case report and review of the literature. Arch Pathol Lab Med.
126:599–601. 2002.PubMed/NCBI
|
|
5.
|
Rosales-Olivares LM, Baena-Ocampo Ldel C,
Miramontes-Martínez VP, Alpízar-Aguirre A and Reyes-Sánchez:
Aneurysmal bone cyst of the spine. Case report. Cir Cir.
74:377–380. 2006.(In Spanish).
|
|
6.
|
Lange T, Stehling C, Fröhlich B,
Klingenhöfer M, et al: Denosumab: a potential new and innovative
treatment option for aneurysmal bone cysts. Eur Spine J.
22:1417–1422. 2013. View Article : Google Scholar
|
|
7.
|
Zileli M, Isik HS, Ogut FE, Is M, Cagli S
and Calli C: Aneurysmal bone cysts of the spine. Eur Spine J.
22:593–601. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Gurjar HK, Sarkari A and Chandra PS:
Surgical management of giant multilevel aneurysmal bone cyst of
cervical spine in a 10-year-old boy: case report with review of
literature. Evid Based Spine Care J. 3:55–59. 2012.
|
|
9.
|
Tasca L and Reinke T: Aneurysmal bone cyst
in a 21-year-old woman presenting with chronic low back pain in a
chiropractic office: A case report. J Altern Complement Med. Feb
25–2013.(Epub ahead of print).
|
|
10.
|
Levin DA, Hensinger RN and Graziano GP:
Aneurysmal bone cyst of the second cervical vertebrae causing
multilevel upper cervical instability. J Spinal Disord Tech.
19:73–75. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Vale BP, Alencar FJ, de Aguiar GB and de
Almeida BR: Vertebral aneurysmatic bone cyst: study of three cases.
Arq Neuropsiquiatr. 63:1079–1083. 2005.(In Portuguese).
|
|
12.
|
Garg S, Mehta S and Dormans JP: Modern
surgical treatment of primary aneurysmal bone cyst of the spine in
children and adolescents. J Pediatr Orthop. 25:387–392. 2005.
View Article : Google Scholar : PubMed/NCBI
|