Introduction
Pancreaticobiliary maljunction (PBM) is an unusual
congenital anomaly, defined as an anatomical maljunction of the
pancreatic duct and the biliary duct outside of the duodenal wall
(1). PBM has an increased risk of
various complications including cholelithiasis, cholangitis,
pancreatitis and biliary tract malignancy (2). According to a Japanese study group,
PBM may be classified into three different types in which: i) the
common bile duct (CBD) joins the major pancreatic duct (MPD); ii)
the MPD joins the CBD; iii) the fuse union was not seen clearly
(3). Pancreas divisum (PD) is the
most common anatomic variant of the pancreas with dorsal and
ventral pancreatic glands draining separately into the duodenum
(4).The overall endoscopic
detection rate for PD was ~2.9% pooled in a systematic review in
2009, with rates worldwide varying from 2.7 to 22% (5,6).
Furthermore, the coexistence of MPD and PD is extremely rare
clinically, making the complex situation difficult to diagnose and
treat. The present study describes four patients who were
successfully diagnosed with PBM combined with PD and subjected to
endoscopic treatment. Written informed consent was obtained from
each patient.
Case reports
Case 1
An 11-year-old female, complaining of persistent
abdominal pain in the right epigastrium with nausea and vomiting
for two days, was hospitalized in The Second Affiliated Hospital of
Nanjing Medical University (Nanjing, China). Physical examination
revealed right upper abdominal tenderness without jaundice.
Laboratory tests revealed an elevated white blood cell (WBC) count
[WBC, 12.0×109/l; neutrophil (NE), 68.9%] and a high
level of transaminases (alanine transaminase (ALT), 532.1 U/l;
γ-glutamyl transpeptidase (GGT), 152 U/l), while the serum
bilirubin and amylase levels were normal. A computed tomography
(CT) scan demonstrated that the intrahepatic bile duct and upper
CBD of the patient were dilated and a 10×10mm flake shadow with low
density was observed in the distal CBD. No imaging features
indicative of pancreatitis were observed. Magnetic resonance
cholangiopancreatography (MRCP) confirmed the stricture of the
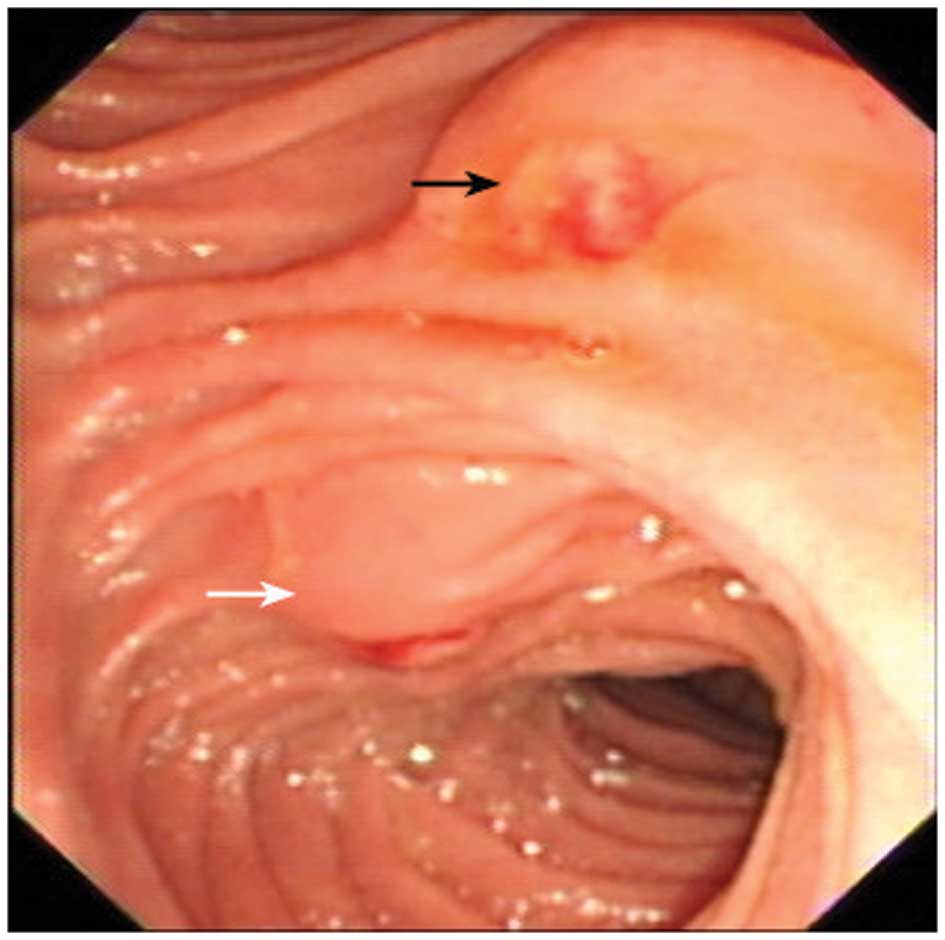
distal CBD. An endoscopic retrograde cholangiopancreatography
(ERCP) was performed, but failed on the first attempt due to
difficult cannulation. In the secondary procedure one week later,
cannulation of the major papilla to biliary duct failed again
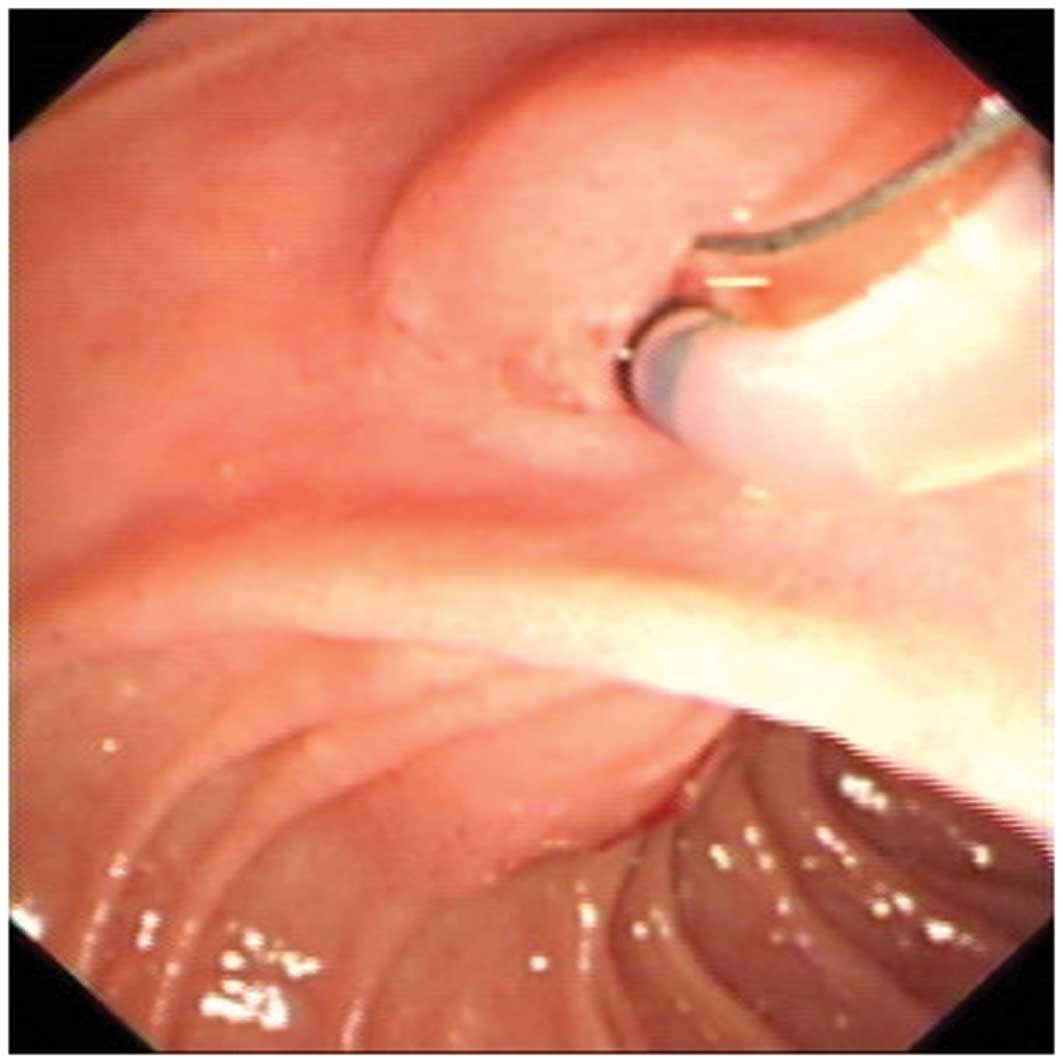
(Figs. 1 and 2). However, cannulation was successful
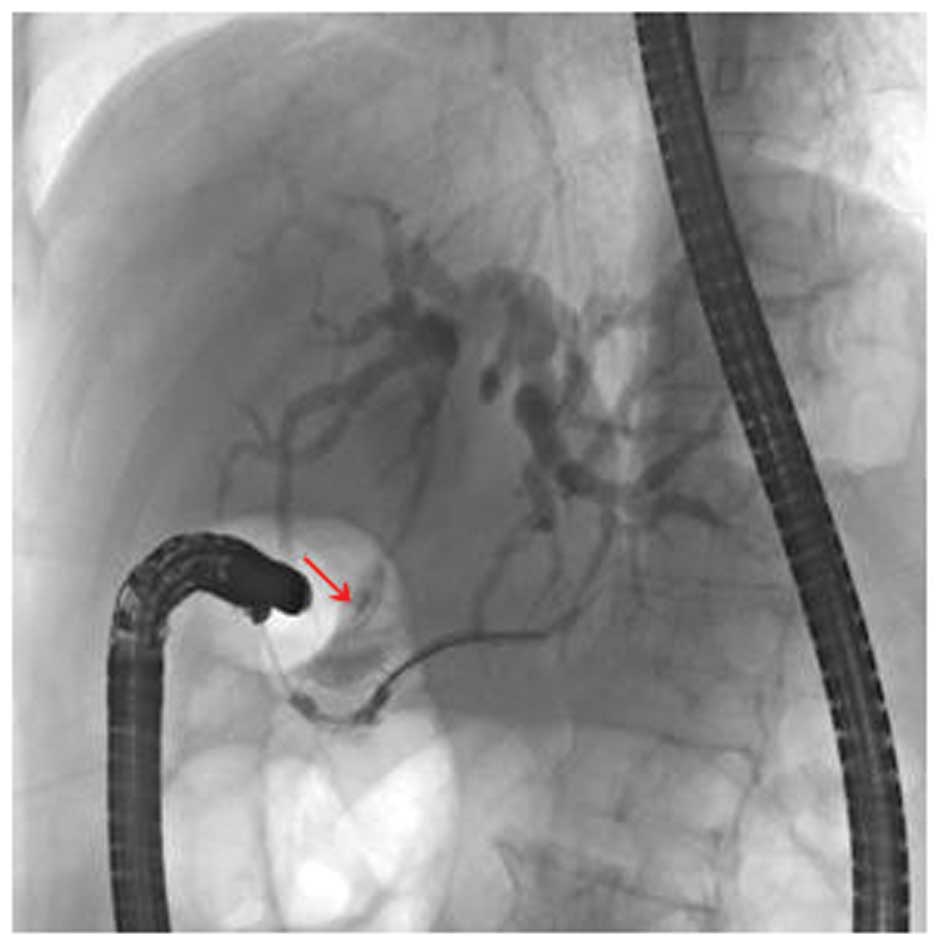
when the minor papilla was used and X-ray imaging revealed that the
guidewire had reached the accessory pancreatic duct. Injection of a
contrast agent into the accessory pancreatic duct revealed intra-
and extra-hepatic bile duct dilation and distal CBD stricture with
its orifice on the accessory pancreatic duct (Fig. 3). After two months, the minor
papilla was cannulated to the biliary duct through the accessory
pancreatic duct and a pigtail plastic pancreatic stent was
implanted into biliary duct following endoscopic sphincterotomy
(EST). The patient’s symptoms were resolved and did not return. The
stent was removed six months later and the patient remained
asymptomatic during the 2 years follow-up.
Case 2
A 57-year-old female presented to our academic
center (Second Affiliated Hospital of Nanjing Medical University)
after experiencing 17 days of paroxysmal upper abdominal cramps and
a fever. Physical examination revealed jaundice, subcostal and
right upper abdominal tenderness and hepatic percussive pain.
Routine blood tests revealed normal hematological results, while
the liver biochemistry function test suggested cholestasis (ALT,
201 U/l; aspartate transaminase (AST), 90 U/l; total bilirubin
(TBIL), 77 μmol/l; indirect bilirubin (IBIL), 51.1 μmol/l; alkaline
phosphatase (ALP), 251 U/l; GGT, 198 U/l). The levels of amylase
were normal. B-mode ultrasound revealed cystic dilation of the
average-upper CBD, partial intrahepatic bile ducts and
choledocholithiasis. MRCP revealed dilation of the upper CBD (25 mm
in diameter) with a rat-tailed stricture in the lower CBD. The
first ERCP failed due to difficult cannulation from the major
papilla, despite the fact that a precut sphincterotomy had been
performed. When withdrawing the endoscope, bile was observed to be
draining from the minor papilla. The minor papilla was cannulated
and the ERCP was successful. Captured images showed the normal
accessory pancreatic duct and the distal CBD joining the pancreatic
dorsal duct. The patient was transferred to the surgical department
and received cholecystectomy and biliary-enteric Roux-en-Y
anastomosis. The surgery confirmed the diagnostic accuracy of ERCP.
During the next 4 years follow-up, the patient lived
non-eventfully.
Case 3
A 26-year-old female, who had undergone a
cholecystectomy and CBD exploration, was admitted having
experienced abdominal pain in the right upper quadrant for ~2
months. T-tube imaging showed that the distal CBD of the patient
was narrow and tortile so that the contrast agent (Iohexol; YZJ
group, Taizhou, China) was unable to discharge into the duodenal
lumen. Duodenoscopy revealed a normal structure of the major
papilla but it was not possible to perform ERCP due to complex
cannulation. Subsequently, the patient received percutaneous
choledochoscopy (PTC) and imaging demonstrated that an orifice
existed at the distal end of the CBD, but the contrast agent was
unable to access the duodenal lumen. In order to determine whether
a malignant obstruction was present, ERCP was performed on the
patient one month later. The endoscopic procedure was successful
when cannulation from the minor papilla was carried out. Following
dilation of the distal CBD with a balloon, a contrast agent was
injected into CBD and an X-ray revealed a cystic dilation at the
distal CBD. Following further dilation of the minor papilla with a
balloon, biliary and pancreatic juice was observed to discharge
into the duodenal lumen. Finally a plastic pancreatic stent was
placed for drainage. Subsequently, stent replacement was conducted
every 3–6 months and no further procedural complications were
encountered.
Case 4
A 70-year-old female presented with a three year
history of recurrent episodes of abdominal pain in the right upper
quadrant and two months of exacerbation. The patient’s amylase
levels were normal. However, B-mode ultrasound had revealed
cholelithiasis; therefore, the patient received a cholecystectomy
two months prior to presentation. However, the symptoms reappeared
and a second B-mode ultrasound conducted one month prior to
presentation revealed right intrahepatic bile duct stones. CT and
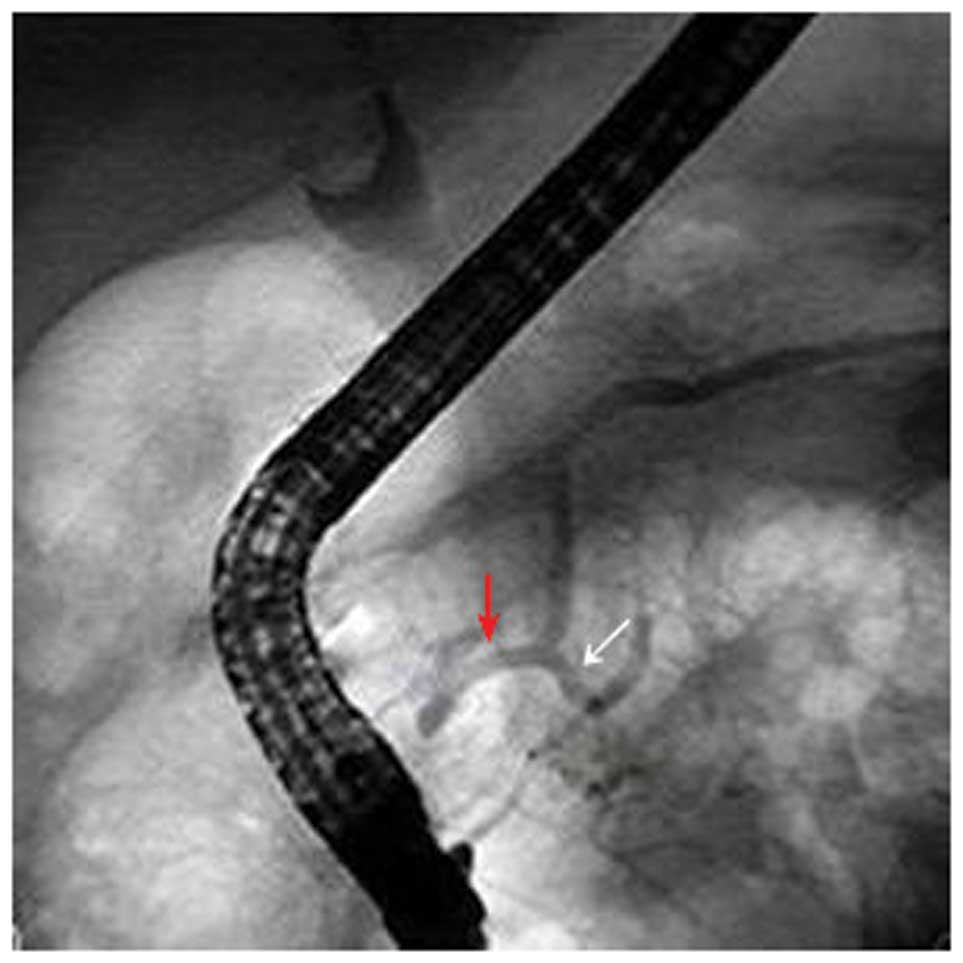
MRCP revealed that the distal CBD was dilated; therefore, ERCP was
performed. Following the failure of cannulation from the major
papilla, cannulation from the minor papilla was successfully
achieved. An X-ray revealed that the distal CBD had joined the
pancreatic dorsal duct and subsequently a plastic biliary stent was
placed for drainage (Fig. 4).
According to the wishes of the patient’s relatives, the patient was
discharged after seven days of ERCP treatment when the abdominal
pain had ceased. The patient was unavailable for follow-up.
Discussion
In patients with PBM, the anatomical maljunction of
the pancreatic duct and the biliary duct is located outside of the
duodenal wall so that the sphincter of Oddi does not directly
affect the junction. As the hydropressure in the pancreatic duct is
higher than that in biliary duct, pancreatic juice frequently
refluxes into the biliary duct in PBM (7), which usually causes lithogenesis,
recurrent pancreatitis or intermittent upper abdominal pain with
elevation of amylase levels and liver damage (8). PD is a congenital anomaly in which
the dorsal and ventral pancreatic ducts drain separately into the
duodenum. The main drainage duct of the dorsal pancreatic bud is
the accessory pancreatic duct and, in the embryo, it drains bile
into the duodenum from the minor duodenal papilla in the embryo. As
the body grows, the duct of the dorsal bud atrophies, losing its
drainage function (9). Whether PD
causes pancreatitis or other complications remains controversial.
In the current study, all four cases exhibited both congenital
anomalies.
McMahon et al reported an anomalous
communication between the dorsal pancreatic duct and the CBD via a
small ventral pancreatic duct branch. The patient presented with a
distal biliary stricture, but the MRCP did not reveal the anomaly.
The disease was confirmed by MRCP with intravenous secretin
administration, and the patient received a Whipple
pancreaticoduodenectomy (10).
Terui et al studied 78 children with PBM and PD, and
concluded that PD rarely combines with PBM and does not cause
pancreatitis due to the fact that the incidence of pancreatitis in
PD combined with PBM is commensurate with that of isolated PD
(11). However, cases where the
CBD joins the dorsal pancreatic duct have rarely been reported.
The majority of PD patients remain asymptomatic
throughout their lives. However, once symptoms such as jaundice or
upper abdominal pain appear, MRCP is the first choice for
diagnosis, rather than ERCP, as it is non-invasive. However, MRCP
is incapable of revealing the variant anatomy due to the absence of
fluid in the CBD or the pancreatic duct, even when secretin is used
(13). Diagnostic accuracy may be
increased using three-dimensional or dynamic MRCP with secretin
stimulation (12). For patients
with anatomical maljunction, ERCP remains the gold standard
procedure.
Therapeutic options for a patient suffering from PD
combined with PBM include open surgery and ERCP, for removal of the
stones or the implantation of a stent across the stricture.
However, patients are likely to be confronted with the failure of
cannulation during ERCP therapy. With dilating CBD images and
difficult cannulation during ERCP, many endoscopists tend to select
precut sphincterectom. However, the lack of a patient’s medical
history, inexperience of the endoscopist, repeated cannulation and
precut sphincterotomy may increase the risk of perforation,
bleeding and other complications. The existence of an anatomical
maljunction is also a risk factor of failure for a precut
sphincterectomy, and requires caution. To date, there are no
guidelines showing the exact indications for precut sphincterotomy
or cannulation of the minor papilla when performing ERCP. Kouchi
et al support cannulation of the minor papilla when the main
pancreatic duct is undetected following cannulation of the major
papilla alone, in children with choledochal cysts (14).
Considering the anomalous fusion position of the CBD
and the pancreatic duct, a tentative minor papilla cannulation is
recommended when repeated cannulation to the major papilla fails
for patients with distal biliary stricture, even if the patient’s
MRCP does not reveal a pancreatobiliary anomaly.
References
|
1
|
Ono S, Fumino S and Iwai N: Diagnosis and
treatment of pancreaticobiliary maljunction in children. Surg
Today. 41:601–605. 2011. View Article : Google Scholar
|
|
2
|
Sugiyama M, Atomi Y and Kuroda A:
Pancreatic disorders associated with anomalous pancreaticobiliary
junction. Surgery. 126:492–497. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Babbitt DP: Congenital choledochal cysts:
new etiological concept based on anomalous relationships of the
common bile duct and pancreatic bulb. Ann Radiol (Paris).
12:231–240. 1969.(In multiple languages).
|
|
4
|
Liao Z, Gao R, Wang W, Ye Z, Lai XW, Wang
XT, Hu LH and Li ZS: A systematic review on endoscopic detection
rate, endotherapy, and surgery for pancreas divisum. Endoscopy.
41:439–444. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Alempijevic T, Stimec B and Kovacevic N:
Anatomical features of the minor duodenal papilla in pancreas
divisum. Surg Radiol Anat. 28:620–624. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kin T, Shapiro AM and Lakey JR: Pancreas
divisum: a study of the cadaveric donor pancreas for islet
isolation. Pancreas. 30:325–327. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Csendes A, Kruse A, Funch-Jensen P, Oster
MJ, Ornsholt J and Amdrup E: Pressure measurements in the biliary
and pancreatic duct system in controls and patients with
gallstones, previous cholecystectomy, or common bile duct stones.
Gastroenterology. 77:1203–1210. 1979.PubMed/NCBI
|
|
8
|
Gonoi W, Akai H, Hagiwara K, et al:
Pancreas divisum as a predisposing factor for chronic and recurrent
idiopathic pancreatitis: initial in vivo survey. Gut. 60:1103–1108.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Quest L and Lombard M: Pancreas divisum:
opinio divisa. Gut. 47:317–319. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
McMahon CJ, Vollmer CM Jr, Goldsmith J,
Brown A, Pleskow D and Pedrosa I: An unusual variant of anomalous
pancreaticobiliary junction in a patient with pancreas divisum
diagnosed with secretin-magnetic resonance
cholangiopancreatography. Pancreas. 39:101–104. 2010. View Article : Google Scholar
|
|
11
|
Terui K, Hishiki T, Saito T, et al:
Pancreas divisum in pancreaticobiliary maljunction in children.
Pediatr Surg Int. 26:419–422. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kamisawa T, Tu Y, Egawa N, Tsuruta K,
Okamoto A and Kamata N: MRCP of congenital pancreaticobiliary
malformation. Abdom Imaging. 32:129–133. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Carnes ML, Romagnuolo J and Cotton PB:
Miss rate of pancreas divisum by magnetic resonance
cholangiopancreatography in clinical practice. Pancreas.
37:151–153. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kouchi K, Yoshida H, Matsunaga T, Kuroda
H, Hishiki T, Saito T, Matsuura G, Komatsu S and Ohnuma N: Efficacy
of ERCP via the accessory papilla in children with choledochal
cysts. Gastrointest Endosc. 59:119–123. 2004. View Article : Google Scholar : PubMed/NCBI
|