Introduction
Smoking is one of the leading causes of mortality
worldwide. Over half of long-term smokers succumb to
tobacco-related diseases (1). In
2010, an estimated 28.1% of adults in China (301 million; 52.9%
males and 2.4% females) were current smokers and 91.8% of the
smokers who attempted to quit did not use any method to assist with
smoking cessation (2). Only 2.5%
of males and 3.5% of females were successful at remaining abstinent
for ≥24 months (3). One-third of
the male population in China is likely to succumb to
tobacco-related mortalities if high smoking rates persist (4). There are specific smoking cessation
medications available in China; however, few smokers (5.6%) use
these since there is little concern with regard to the health
effects of smoking (5). Thus, the
identification of an effective method to aid smoking cessation in
China is urgent and cognitive intervention may be useful.
Chronic obstructive pulmonary disease (COPD) is a
global health crisis with smoking as its most causative factor.
Almost 50% of older smokers develop COPD (6). The prevalence of COPD in residents
≥40 years old is 8.2% in China (7). Smoking cessation is the most
significant intervention in COPD management and is recommended by
the Global initiative for Chronic Obstructive Lung Diseases (GOLD)
(8), as it may slow down disease
progression (9).
Studies from developed countries show that cognitive
counseling is a cost-effective treatment for motivation and
behavior-based smoking cessation (10–12).
The effects shown in various groups of individuals remain
ambiguous. Specific individuals consider cognitive counseling to be
more effective in smokers with airway obstruction (13), while others do not consider it to
be effective at all (14). Few
studies concerning individual counseling for smoking cessation have
been conducted in China, particularly in patients with COPD. The
present prospective randomized study evaluated the efficacy of
individual counseling for smoking cessation in COPD patients and
asymptomatic smokers in China.
Materials and methods
Participants
Smoking subjects with or without COPD were recruited
by residential area advertisements or from the pulmonary outpatient
clinic and Physical Examination Center of the Second Xiangya
Hospital (Changsha, China) over a six-month period between March
2010 and September 2010. All subjects underwent standard lung
function tests with measurements of forced vital capacity (FVC) and
forced expiratory volume in 1 sec (FEV1). COPD was
defined according to the GOLD criteria (FEV1/FVC <70%
following bronchodilatation) (8).
Asymptomatic smokers were defined as smokers without respiratory
symptoms (i.e., cough, sputum production or dyspnea) and with
normal lung function. Enrolled subjects were >18 years-old and
had smoked one or more cigarettes/day for a minimum of 100 days.
Subjects with experience of smoking cessation medication and those
with a history of asthma, asbestosis, silicosis, bronchiectasis or
lung cancer were excluded from the study. All subjects provided
informed consent approved by the medical ethics committee of the
Second Xiangya Hospital.
Study design
It is generally accepted that the motivation to quit
is one of the most significant factors associated with smoking
cessation (15). The smokers (COPD
and asymptomatic) were divided into four categories according to
their motivation to quit: No desire to quit, indifference, hoping
to quit and hoping very much to quit. Smokers in each category were
assigned to the intervention or control group according to the
randomized digital table, where the quitting motivations were
comparable between the two groups.
The intervention group was provided with individual
cognitive counseling based on face-to-face individual counseling
(performed at the baseline), self-help materials, as well as nine
telephone calls at weeks 1, 2, 3, 4, 6 and 8 and at months 3, 4 and
5. The face-to-face individual counseling, which lasted for 20 min,
was based on the five ‘A’s’ method. This relates to the harm of
smoking, possible benefits of smoking cessation, methods of
quitting, methods of handling withdrawal symptoms and prevention of
relapses (16). For smokers with
COPD, the counseling content focused on the correlation between
smoking habits and COPD. The self-help materials included specific
smoking cessation handbooks with smoking cessation tips. Each
telephone call lasted for >10 min and was designed to further
promote smoking cessation and help smokers conquer issues that
occurred during smoking cessation. The control group was provided
with smoking cessation advice. All interventions were conducted by
two doctors with experience of professional smoking cessation
treatment.
The main assessments were performed at the baseline,
week 4 and month 6. Nicotine dependence was assessed using the
Fagerström Test for Nicotine Dependence (FTND). The St. George
Respiratory Questionnaire (SGRQ) for measuring health-related
quality of life and exacerbation times during the 6 months was
recorded for COPD patients. An exacerbation was defined according
to the GOLD parameter, specifically associated with acute events
characterized by a worsening of the patient’s respiratory symptoms
beyond normal day-to-day variations, leading to a change in
medication (8). The abstinence was
defined as a self-reported sustained abstinence from week 4 to
month 6. The self-reported abstinence at week 4 and month 6 was
verified by an exhaled carbon monoxide level of <10 ppm.
Statistical analysis
The minimum total sample was 152 participants. The
expected to the success rates were 25% for the intervention group,
compared with 5% for the control group, with a two tailed
significance level of 0.05 and a power of 80%. Statistical analyses
were performed using SPSS 17.0 statistical software (SPSS, Inc.
Chicago, IL, USA). P<0.05 was considered to indicate a
statistically significant difference. The normally distributed
quantitative data was analyzed using t-tests, non-normally
distributed data with Wilcoxon Mann-Whitney U-tests and categorical
variable data with χ2 tests. Predictors of outcome were
analyzed with multinomial logistic regression.
Results
Baseline characteristics
A total of 85 COPD patients and 105 asymptomatic
smokers were included in the study. Twelve smokers (5 COPD and 7
asymptomatic) withdrew during the 6-month period. The most common
reason for withdrawal was attributed to poor compliance. The
withdrawers were regarded as smokers and were included in the
outcome analyses. Table I lists
the baseline characteristics of all subjects. The baseline
characteristics were kept well-balanced between the intervention
and the control groups; they were also balanced between the
intervention and the control group for COPD and asymptomatic
smokers. There were certain significant differences in baseline
characteristics between the COPD patients and asymptomatic smokers.
Age, pack-years and quitting motivations were significantly higher
in COPD patients than in asymptomatic smokers and the educational
level in the COPD patients was lower than that in asymptomatic
smokers. The severity of COPD was classified according to the
predicted FEV1 percentage. The following percentages
were observed in terms of COPD grading: 11% subjects were mild
(FEV1 ≥80% predicted), 46% were moderate
(FEV1 ≥50–80% predicted), 33% were severe
(FEV1 ≥30–50% predicted) and 10% were very severe
(FEV1 <30% predicted). A full representation is shown
in Table II.
 | Table IParticipant characteristics. |
Table I
Participant characteristics.
| | | COPD | Asymptomatic
smokers |
|---|
| | |
|
|
|---|
| Characteristics | Intervention group,
n=94 | Control group,
n=96 | Intervention group,
n=42 | Control group,
n=43 | Intervention group,
n=52 | Control group,
n=53 |
|---|
| Age, years | 50.8±13.9 | 50.3±13.2 | 61.4±8.6 | 61.6±7.7 | 41.7±10.1a | 41.6±9.8b |
| Male:female | 91:3 | 93:3 | 41:1 | 41:2 | 50:2 | 52:1 |
| Pack-years | 31.6±18.8 | 32.6±20.4 | 40.2±18.2 | 44.3±15.9 | 23.7±15.4a | 24.0±19.4b |
| Daily cigarettes | 19.0±10.3 | 20.6±12.7 | 17.5±8.4 | 17.2±9.6 | 22.4±10.6 | 23.6±13.9 |
| Carbon monoxide,
ppm | 15.1±8.2 | 16.1±8.2 | 14.2±7.3 | 14.1±8.5 | 17.5±8.4 | 18.3±9.2 |
| FTND, points | 4.1±2.4 | 4.2±2.3 | 4.0±2.0 | 4.1±2.5 | 4.2±2.1 | 4.3±2.4 |
| Education, n |
| Junior high school
or less | 40 | 34 | 28 | 20 | 12 | 14 |
| Senior high
school | 23 | 23 | 10 | 14 | 13 | 9 |
| College or more | 31 | 39 | 4 | 9 | 27 | 30 |
| Quitting motivation,
n |
| No desire to
quit | 17 | 18 | 3 | 3 | 14 | 15 |
| Indifference | 27 | 26 | 5 | 5 | 22 | 21 |
| Hoping to quit | 37 | 39 | 23 | 24 | 14 | 15 |
| Hoping very much to
quit | 13 | 13 | 11 | 11 | 2 | 2 |
 | Table IIAbstinence rates stratified by
baseline spirometric results. |
Table II
Abstinence rates stratified by
baseline spirometric results.
| | COPD |
|---|
| |
|
|---|
| Variable | Normal | All | Mild | Moderate | Severe | Very severe |
|---|
| Subjects | 105 | 85 | 9 | 39 | 29 | 8 |
| Abstainers | 7 | 25 | 2 | 10 | 9 | 4 |
| Abstinence rates,
% | 6.7 | 29.4 | 22.2 | 25.6 | 31.0 | 50.0 |
| P-value | <0.001a | 0.540b | | | | |
Smoking cessation outcomes
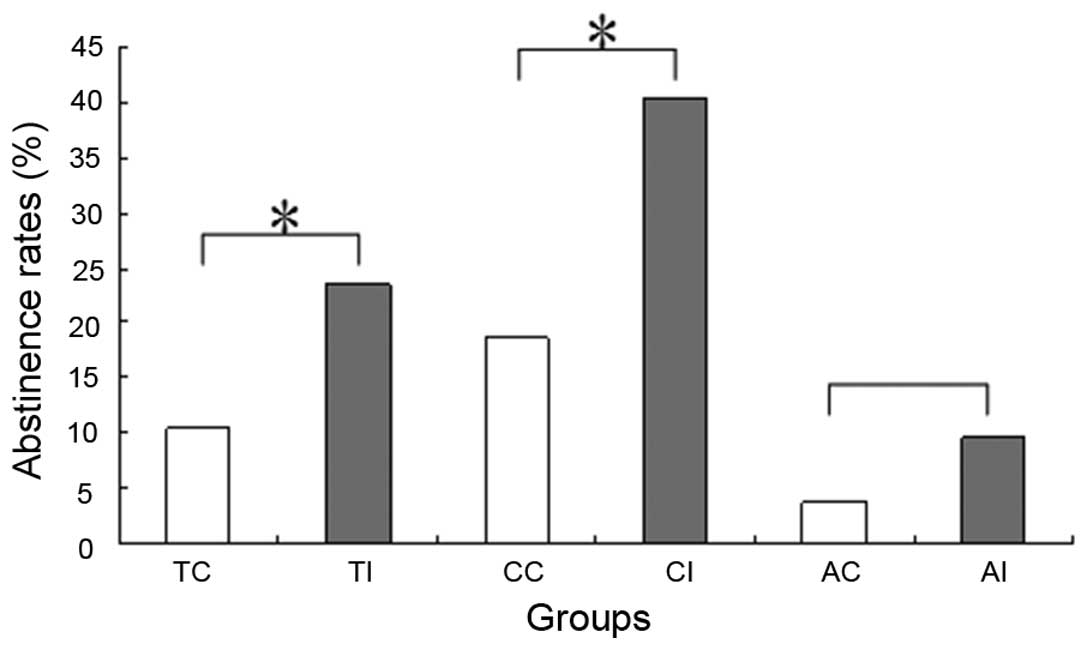
Fig. 1 lists
smoking cessation outcomes. When smokers with and without COPD were
considered together, the abstinence rates were higher in the
intervention group than in the control group (23.4 vs. 10.4%;
P=0.007). The result is similar to that based exclusively on
smokers with COPD (40.5 vs. 18.6%; P=0.027). However, the effect of
individual counseling in asymptomatic smokers was statistically
insignificant (9.6 vs. 3.8%; P=0.230). Table II lists the various abstinence
rates in smokers who have different spirometric results. Smokers
with COPD were more likely to quit smoking (29.4%) than those with
normal spirometry (6.7%; P<0.001). Although higher COPD grades
correlated with a higher abstinence rate, the differences in
abstinence rates among the mild, moderate, severe and very severe
COPD groups were statistically insignificant (22.2, 25.6, 31.0,
50.0%, respectively; P=0.540).
Health outcomes
This analysis was based on the COPD participants.
Only the proportion of patients who had an improvement of four or
more SGRQ score units was used in the calculation, as this group
showed significant clinical changes in the quality of life. Of the
COPD patients who abstained from smoking, 36.0% had significant
improvements in the SGRQ total scores; this was significantly
higher than the 13.3% in patients who failed to stop smoking
(P=0.037). During the six-month period, there was an average of
0.61 exacerbations in the COPD patients who abstained from smoking,
compared with 1.21 exacerbations in the patients who continued to
smoke (Z, −3.32; P<0.001).
Predictors of smoking cessation
outcomes
Multinomial logistic regression was used to analyze
whether the abstinence outcome was associated with various
predictors (Table III).
Individual counseling, COPD and quitting motivation were found to
be independent predictors of abstinence, where COPD was the most
significant (odds ratio, 4.215; 95% confidence interval,
2.215–7.865). Other factors, including age, gender, daily
cigarettes, pack-years, FTND, educational background and SGRQ, were
included in the initial regression model. However, they were not
found to have a statistically significant association with
abstinence.
 | Table IIIPredictors of smoking cessation in
the logistic regression model. |
Table III
Predictors of smoking cessation in
the logistic regression model.
| Predictors | B | P-value | OR | 95% CI |
|---|
| Airway
obstruction | 1.652 | 0.000 | 4.217 | 2.215–7.865 |
| Individual
counseling | 1.133 | 0.007 | 3.104 | 1.369–7.042 |
| Quitting
motivation | 1.146 | 0.000 | 3.145 | 1.780–5.557 |
Discussion
The present study is, to the best of our knowledge,
the first randomized controlled trial in China that has
demonstrated the efficacy of individual counseling for smoking
cessation in smokers with COPD and asymptomatic smokers. The most
significant observation was that individual counseling was an
effective method for smoking cessation. This was particularly true
in smokers with COPD.
The results of the present study correlated with
previous studies evaluating the efficiency of individual counseling
for smoking cessation in developed countries. Bednarek et al
(13), in Poland, recruited 4,494
smokers; all these smokers received simple smoking cessation advice
while 1,177 subjects with airway obstruction were informed that
they had COPD and that smoking cessation would halt the lung
disease progression. One year later, the sustained smoking
cessation rate in those with airway obstruction was 16.3%, compared
with 12.0% in those with normal spirometric parameters (P=0.0003)
(12). Stratelis et al
(17), in Sweden, obtained a
similar result. In this study, 512 smokers enrolled and received
annual spirometry and brief smoking cessation advice, followed up
by a personal letter from a physician. Three years later, 25% of
smokers with COPD were smoke-free for ≥1 year, compared with 7% of
smokers with normal lung function (P<0.001). These studies and
the results of the present study indicate that individual
counseling is efficacious in helping smokers to quit and its
efficiency in COPD patients was more marked. However, a study by
Willemse et al (14) in the
Netherlands used group meetings for smoking cessation and reported
a 42% (16/38) abstinence rate in COPD patient smokers, in
comparison to a 68% (17/25) abstinence rate in healthy smokers. The
authors did not offer the statistical analysis for these results.
One explanation may be that the healthy smokers that were recruited
had a higher motivation for smoking cessation. The authors did not
assess the motivation of their subjects. Toljamo et al
(15), in Finland, enrolled 584
smokers; the study provided individual counseling to all
individuals. The study reported a 5.4% sustained abstinence rate in
smokers without COPD, compared with 10.6% in patients with COPD
(P=0.125); success in quitting was not identified to be associated
with airway obstruction. However, there was a clear difference
between their study and the present study. Spirometry was conducted
at the end of their study. Therefore, the COPD patients were not
informed of their illness. In comparison, the patients in the
present study, who received counseling, found that an awareness of
the correlation between smoking habits and COPD may be useful for
smoking cessation.
Improved cessation rates were found in smokers who
had COPD. The factors leading to this result included several
components. First, the quitting motivations were higher in COPD
patients than in general smokers. The majority of patients with
COPD suffered from a cough and dyspnea, which are widely considered
to be harmful effects of smoking. Concern for personal health was
the most popular reason for considering smoking cessation in China
(5). Secondly, positive
spirometric results and a COPD diagnosis show patients the harmful
effects of smoking and the necessity of smoking cessation. The
United States National Lung Health Education Program previously
recommended spirometric testing for increasing the motivation of
smokers to quit (18). Parkes
et al (19) used ‘lung
age’, according to spirometric results, in order to encourage
smoking cessation; their study reported that independently verified
rates of quitting at 12 months in the intervention and control
groups were 13.6 and 6.4% (P=0.005), respectively. In addition,
smoking is a social behavior in China. Individuals often share
cigarettes with each other, making it difficult for asymptomatic
smokers to stop smoking. Smokers with COPD may reject cigarettes
offered to them due to their disease.
The goals of clinical control for COPD patients
included improvement of exercise tolerance, emotional function,
prevention of disease progression and minimization of symptoms, all
of which may lead to an increased quality of life (8). Despite continuous airway inflammation
in ex-smokers with COPD (20),
smoking cessation is an effective method of reducing the progress
of the disease by slowing down the annual FEV1 decline
rate (9) and it may result in an
increase of quality-adjusted life-years for COPD patients (10). The dyspnea and cough symptoms that
COPD patients often experience may be improved following smoking
cessation (21). The health
outcomes in the present study demonstrate statistically significant
improvements in SGRQ total scores and COPD exacerbations in
patients with COPD who abstained from smoking, demonstrating that
smoking cessation may result in increased health benefits for COPD
patients.
A number of factors are involved in smoking
cessation. Studies from Western countries have shown that health
status and economic reasons are the most commonly associated
factors (22,23). In addition, smoking abstinence is
associated with old age, male gender, high income, high levels of
education, low nicotine dependence and smoke-free family policies
(15,24). A study from South Africa showed
that clinical interventions and smoke-free family policies may
increase the rate of smoking cessation (25). Previous studies in China observed
that the interest in quitting among smokers is affected by past
quitting experiences, nicotine dependence, health concerns and
attitudes towards smoking (26,27).
The observations of the present study confirmed previous
observations showing that motivation and health status were the
most significant factors affecting the result of smoking cessation.
It was found that individual counseling was another significant
factor. Demographic characteristics and nicotine dependence were
not identified to be independent factors for smoking cessation,
possibly owing to the small sample size.
There are several limitations in the present study.
The majority of COPD patients were recruited from the outpatient
clinic and therefore possibly had more severe clinical symptoms
than the typical patient with COPD. Thus, the patients may be more
motivated to quit smoking. In addition, the majority of the
subjects in this study were from Hunan Province in China. Hence,
the study population may not be a true representation of all
smokers in China.
In conclusion, individual smoking cessation
counseling is an effective method for helping COPD patients to quit
and may result in increased health benefits. Health professionals
should provide cognitive counseling to smokers to help them quit
smoking. Quitting motivation, healthy status factors and individual
counseling are significant factors associated with smoking
cessation results. The individual counseling efficiency for
asymptomatic smokers remains uncertain and further nationwide
multicenter studies are required to investigate this further in the
future.
Acknowledgements
This study was supported by grants from the Chinese
National Natural Science Foundation (nos. 81070039 and 81270100)
and the Chronic Respiratory Diseases Research Fund of the Chinese
Medical Association (no. 08020520130).
References
|
1
|
World Health Organization. WHO Report on
the Global Tobacco Epidemic. 2008, http://www.who.int/tobacco/mpower/mpower_report_full_2008.pdfuri.
Accessed March 31, 2010
|
|
2
|
Li Q, Hsia J and Yang G: Prevalence of
smoking in China in 2010. N Engl J Med. 364:2469–2470. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Qian J, Cai M, Gao J, Tang S, Xu L and
Critchley JA: Trends in smoking and quitting in China from 1993 to
2003: National Health Service Survey data. Bull World Health Organ.
88:769–776. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Dobson R: One third of Chinese men will be
killed by tobacco if high smoking rates persist. BMJ. 338:b3022009.
View Article : Google Scholar
|
|
5
|
Jiang Y, Elton-Marshall T, Fong GT and Li
Q: Quitting smoking in China: findings from the ITC China Survey.
Tob Control. 19(Suppl 2): i12–i17. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Lundbäck B, Lindberg A, Lindstrõm M, et
al; Obstructive Lung Disease in Northern Sweden Studies. Not 15 but
50% of smokers develop COPD? - Report from the Obstructive Lung
Disease in Northern Sweden Studies. Respir Med. 97:115–122.
2003.
|
|
7
|
Zhong N, Wang C, Yao W, et al: Prevalence
of chronic obstructive pulmonary disease in China: a large,
population-based survey. Am J Respir Crit Care Med. 176:753–760.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Global Initiative for Chronic Obstructive
Lung Disease (GOLD). Global Strategy for the Diagnosis, Management
and Prevention of COPD. 2010, http://www.goldcopd.org/uploads/users/files/GOLD_Pocket_2010Mar31.pdfuri.
Accessed March 31, 2010
|
|
9
|
Lee PN and Fry JS: Systematic review of
the evidence relating FEV1 decline to giving up smoking. BMC Med.
8:842010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Atsou K, Chouaid C and Hejblum G:
Simulation-based estimates of effectiveness and cost-effectiveness
of smoking cessation in patients with chronic obstructive pulmonary
disease. PLoS One. 6:e248702011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bao Y, Duan N and Fox SA: Is some provider
advice on smoking cessation better than no advice? An instrumental
variable analysis of the 2001 National Health Interview Survey.
Health Serv Res. 41:2114–2135. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Schuck K, Otten R, Kleinjan M, Bricker JB
and Engels RC: Effectiveness of proactive telephone counselling for
smoking cessation in parents: study protocol of a randomized
controlled trial. BMC Public Health. 11:7322011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Bednarek M, Gorecka D, Wielgomas J, et al:
Smokers with airway obstruction are more likely to quit smoking.
Thorax. 61:869–873. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Willemse B, Lesman-Leegte I, Timens W,
Postma D and ten Hacken N: High cessation rates of cigarette
smoking in subjects with and without COPD. Chest. 128:3685–3687.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Toljamo T, Kaukonen M, Nieminen P and
Kinnula VL: Early detection of COPD combined with individualized
counselling for smoking cessation: a two-year prospective study.
Scand J Prim Health Care. 28:41–46. 2010.PubMed/NCBI
|
|
16
|
The Tobacco Use and Dependence Clinical
Practice Guideline Panel, Staff, and Consortium Representatives. A
clinical practice guideline for treating tobacco use and
dependence: A US Public Health Service report. JAMA. 283:3244–3254.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Stratelis G, Mölstad S, Jakobsson P and
Zetterström O: The impact of repeated spirometry and smoking
cessation advice on smokers with mild COPD. Scand J Prim Health
Care. 24:133–139. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Ferguson GT, Enright PL, Buist AS and
Higgins MW: Office spirometry for lung health assessment in adults:
A consensus statement from the National Lung Health Education
Program. Chest. 117:1146–1161. 2000. View Article : Google Scholar
|
|
19
|
Parkes G, Greenhalgh T, Griffin M and Dent
R: Effect on smoking quit rate of telling patients their lung age:
the Step2quit randomised controlled trial. BMJ. 336:598–600. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Willemse BW, ten Hacken NH, Rutgers B,
Lesman-Leegte IG, Postma DS and Timens W: Effect of 1-year smoking
cessation on airway inflammation in COPD and asymptomatic smokers.
Eur Respir J. 26:835–845. 2005.PubMed/NCBI
|
|
21
|
Papadopoulos G, Vardavas CI, Limperi M,
Linardis A, Georgoudis G and Behrakis P: Smoking cessation can
improve quality of life among COPD patients: validation of the
clinical COPD questionnaire into Greek. BMC Pulm Med. 11:132011.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Sieminska A, Buczkowski K, Jassem E,
Lewandowska K, Ucinska R and Chelminska M: Patterns of motivations
and ways of quitting smoking among Polish smokers: a questionnaire
study. BMC Public Health. 8:2742008. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Hyland A, Li Q, Bauer JE, Giovino GA,
Steger C and Cummings KM: Predictors of cessation in a cohort of
current and former smokers followed over 13 years. Nicotine Tob
Res. 6(Suppl 3): S363–S369. 2004.PubMed/NCBI
|
|
24
|
Lee CW and Kahende J: Factors associated
with successful smoking cessation in the United States, 2000. Am J
Public Health. 97:1503–1509. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Ayo-Yusuf OA and Szymanski B: Factors
associated with smoking cessation in South Africa. S Afr Med J.
100:175–179. 2010.PubMed/NCBI
|
|
26
|
Feng G, Jiang Y, Li Q, et al:
Individual-level factors associated with intentions to quit smoking
among adult smokers in six cities of China: findings from the ITC
China Survey. Tob Control. 19(Suppl 2): i6–i11. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Yang T, Abdullah AS, Mustafa J, Chen B,
Yang X and Feng X: Factors associated with smoking cessation among
Chinese adults in rural China. Am J Health Behav. 33:125–134. 2009.
View Article : Google Scholar : PubMed/NCBI
|