Introduction
Immunoglobulin A nephropathy (IgAN), an immune
complex-mediated glomerulonephritis, is the most common form of
primary glomerulonephritis worldwide and is characterized by
deposits of IgA as either the dominant or codominant immunoglobulin
(1,2). Proteinuria is regarded as a risk
factor for an unfavorable renal prognosis and the reduction of
proteinuria is considered an important therapeutic goal in clinical
practice (3–5). In addition to proteinuria, active
renal lesions, such as cellular crescent formation, diffuse
mesangial proliferation and interstitial inflammatory infiltration
have been identified to result in a rapid rate of deterioration and
lower kidney survival (6).
At present, the optimal immunosuppressive strategy
for IgAN treatment, particularly the duration of treatment, remains
unclear. Treatment with glucocorticoids alone or combined therapy
with glucocorticoids and other immunosuppressive agents have shown
beneficial effects by reducing proteinuria and improving renal
function (7,8). According to the guidelines ‘Kidney
Disease: Improving Global Outcomes’ (KDIGO) (9), which are based on the results of
previous studies (7,10,11),
patients with persistent proteinuria of >1 g/day following 6
months of treatment with renin-angiotensin system (RAS) inhibitors
are suggested to receive a 6-month course of corticosteroid
therapy. However, certain issues require clarification, including
whether immunomodulatory treatment should be continued or withdrawn
in patients with proteinuria of <1 g/day following 6 months of
corticosteroid treatment, and whether the complete resolution of
proteinuria is equivalent to the disappearance of renal active
lesions. Furthermore, the effectiveness of immunosuppressive
regimens other than glucocorticoid monotherapy for this
heterogeneous disease require investigation
In the present study, the effects of an
individualized, low-dose multi-drug immunosuppressive regimen on
IgAN treatment were retrospectively evaluated and a preliminary
investigation of the duration of immunosuppressive treatment for
IgAN based on repeat renal biopsies was conducted.
Materials and methods
Data collection
Clinical data of 17 patients diagnosed with primary
IgAN by biopsy, including 11 males and 6 females with a mean age of
30.5 years (range, 14–61 years) were collected from the medical
records at The Affiliated Hospital of Guangdong Medical College
(Zhangjiang, China). All patients were notified and agreed for
their clinical data to be used in this study. The institutional
review board of the Affiliated Hospital of Guangdong Medical
College approved this study and waived the requirement for patient
consent.
Therapeutic intervention
None of the patients received steroids or other
immunosuppressive agents prior to the first renal biopsy. As shown
in Table I, following the first
biopsy, 16 patients were regularly treated with low-dose prednisone
(PDN) alone or in combination with one or two other low-dose
immunosuppressants. One patient (patient no. 2) discontinued
immunosuppressive therapy from months 9 to 28. Generally, the
immunosuppressive regimen was individualized according to the
patient’s clinical and pathological presentation at the first
biopsy. Briefly, in severe cases of proteinuria and/or the marked
presence of active renal lesions the high dose immunosuppressants
were administered. The initial dose of PDN was ~0.5 mg/(kg·day) for
8 weeks followed by a 10% reduction of the original dose in 1 month
and gradual tapering to maintain a dose of 5–10 mg/day.
Tripterygium wilfordii Hook F (TwHF) was administered orally
at an initial dose of ~1.0 mg/(kg·day) in three divided doses for
~6 months and gradually tapered to 20–30 mg/day as the maintenance
therapy. Azathioprine (AZA) was administered at a single dose of
1–2 mg/(kg·day) for ~6 months and gradually tapered to 25–50 mg/day
as the maintenance therapy. Intravenous cyclophosphamide (CTX) was
administered at 0.8–1.0 g per month for 3 months, followed by 1–2
mg/(kg·day) AZA for an additional 3 months and then gradually
tapered to 25–50 mg/day. All patients received
angiotensin-converting-enzyme inhibitor (ACEI) and/or angiotensin
II receptor blocker (ARB) as part of their anti-hypertensive
regimen or their basic therapy. Six patients (patient nos. 4, 6, 9,
11, 12 and 14) received lipid-lowering agents due to the presence
of hyperlipidemia and 8 patients (patient nos. 1, 2, 3, 4, 5, 7, 10
and 11) received allopurinol due to hyperuricemia.
 | Table IBaseline characteristics of 17
patients with IgA nephropathy who underwent a repeat renal
biopsy. |
Table I
Baseline characteristics of 17
patients with IgA nephropathy who underwent a repeat renal
biopsy.
| Patient | Gender | Age at first biopsy
(years) | Interval
(months) | RAS inhibitors | Immunosuppressive
treament |
|---|
| 1 | F | 28 | 12 | Yes | PDN + TwHF + AZA |
| 2 | M | 21 | 50.5 | Yes | PDN + TwHF +AZA |
| 3 | M | 18 | 9 | Yes | PDN + TwHF + CTX →
AZA |
| 4 | M | 19 | 15 | Yes | PDN + TwHF + AZA |
| 5 | M | 14 | 15 | Yes | PDN + TwHF + AZA |
| 6 | F | 59 | 21 | Yes | PDN + TwHF |
| 7 | M | 22 | 17.5 | Yes | PDN + TwHF + AZA |
| 8 | M | 61 | 12.5 | Yes | PDN + TwHF + AZA |
| 9 | F | 31 | 14 | Yes | PDN + TwHF + AZA |
| 10 | F | 39 | 14 | Yes | PDN + TwHF + AZA |
| 11 | M | 26 | 12.5 | Yes | PDN + TwHF + AZA |
| 12 | M | 35 | 15 | Yes | PDN |
| 13 | M | 14 | 11 | Yes | PDN + AZA |
| 14 | F | 32 | 16.6 | Yes | PDN + TwHF + CTX →
AZA |
| 15 | M | 26 | 17 | Yes | PDN + TwHF + AZA |
| 16 | M | 55 | 12 | Yes | PDN + AZA |
| 17 | F | 18 | 11.5 | Yes | PDN + TwHF |
Follow-up
Sixteen patients underwent regular follow-ups at the
outpatient clinic approximately once a month until they received
the second biopsy. Patient no. 2 discontinued follow-up from months
9 to 28 but continued from months 28 to 50.5. During the follow-up,
the clinical symptoms, drug consumption and possible treatment
complications of the patients were evaluated. Blood pressure was
monitored and standard body examinations were performed. Laboratory
parameters, including serum levels of creatinine, uric acid,
cholesterol and albumin, as well as results of routine blood tests
were recorded. Every month, urinary protein was semi-quantified.
The 24-h urinary protein excretion level was measured at the first
and second renal biopsies. The glomerular filtration rate (GFR) was
estimated using the Modification of Diet in Renal Disease study
(MDRD) formula: [eGFR (ml/min/1.73m2) = 186 * Scr
(mg/dl) − 1.154 * age (years) − 0.203 * (0.742 femal].
Renal biopsies and pathological
diagnosis
All patients underwent renal biopsies twice with an
interval time of 16.2±9.3 months (range, 9.0–50.5 months) under
ultrasound guidance. Following hematoxylin and eosin, Masson’s
trichrome, silver methenamine, periodic acid-Schiff and
immunofluorescent staining, the renal specimens were assessed by
one renal pathologist and one clinical nephrologist who were
blinded to the clinical information. In immunofluorescent staining,
the deposition of IgA, IgG, IgM and complement C3 was
semi-quantified as follows: Negative, (−); minimal in intensity,
(±); slight in intensity, (1+); moderate in intensity, (2+); marked
in intensity, (3+); and marked in intensity and extent, (4+). These
semi-quantified results were converted into scores as follows: 0,
(−); 0.5, (±); 1, (1+); 2, (2+); 3, (3+); and 4 (4+), respectively.
The activity and chronicity indices were evaluated as previously
described (12). Briefly, the
activity index was first graded for mesangial proliferation (grades
0–3: Normal, 0; slight, 1; moderate, 2; and severe, 3),
interstitial inflammatory cell infiltration (grades 0–3: None, 0;
1–20%, 1; 21–50%, 2; and >50%, 3) and cellular crescent
formation (grades 0–3 according to the percentage of glomeruli
involved in crescents: None, 0; 1–20%, 1; 21–50%, 2; and >50%,
3). The sum of these scores was subsequently computed (maximum of
9). The chronicity index was first graded for the percentage of
glomeruli exhibiting fibrous crescents (grades 0–3: None, 0; 1–20%,
1; 21–50%, 2; and >50%, 3), the percentage of glomeruli
exhibiting segmental or global sclerosis (grades 0–3: None, 0;
1–20%, 1; 21–50%, 2; and >50%, 3), and the degrees of tubular
atrophy (on a scale of 0–3) and interstitial fibrosis (on a scale
of 0–3). The sum of these scores was subsequently computed (maximum
of 12).
Statistical analysis
Statistical tests were performed with SPSS software,
version 16.0 for Windows (SPSS Inc., Chicago, IL, USA). Normally
distributed variables were assessed using the paired-samples
t-test. Nonparametric variables and non-normally distributed
variables were assessed by Wilcoxon signed rank test. P<0.05 was
considered to indicate a statistically significant difference.
Results
General data
The regimen was well tolerated and no severe adverse
events were observed. Blood pressure in all patients was controlled
to the standard of ~130/80 mmHg during the course of follow-up.
According to renal pathological diagnosis of the second biopsy,
five patients (patient nos. 5, 10, 14, 15 and 17) were able to
discontinue immunosuppressive treatment as substantially no active
renal lesions were observed, while the remaining patients continued
the regimen with a very low dose of immunosuppressants due to
existing residual active renal lesions.
Clinical data
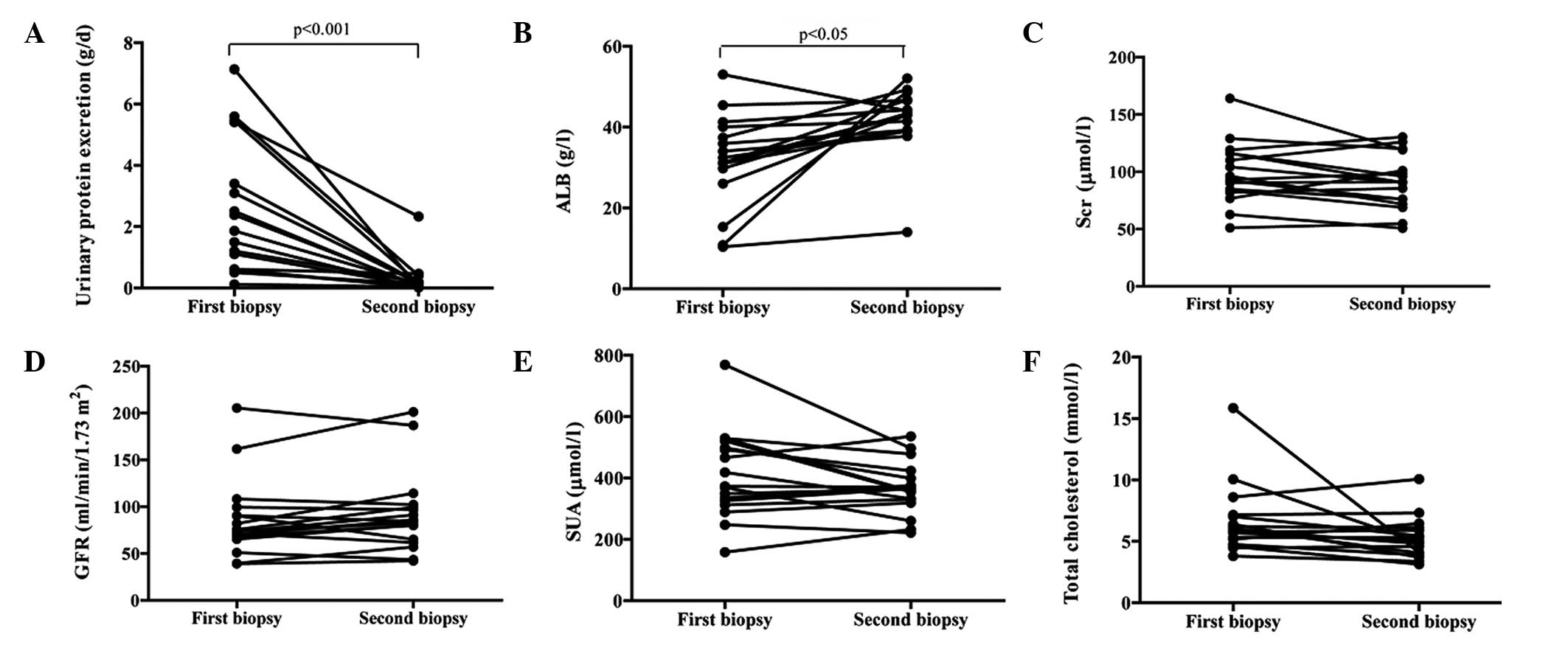
Semi-quantified analysis showed that the urinary
protein levels in all patients decreased gradually to normal levels
from months 2 to 7 (data not shown). The mean 24-h protein
excretion levels markedly declined from 2.53±2.17 g/day at the
first biopsy to 0.26±0.55 g/day at the second biopsy (patient no. 2
was 2.33 g/day) (P<0.001; Fig.
1A). Correspondingly, the serum albumin levels increased
significantly from 31.5±11.3 to 42.1±8.2 g/l (P<0.05; Fig. 1B). The serum creatinine levels
decreased from 98.3±26.5 to 91.0±23.5 μmol/l (Fig. 1C), while the GFR increased from
86.1±41.8 to 92.6±43.1 ml/min/1.73 m2 (Fig. 1D); however, there were no
significant differences in these levels between the two biopsies.
Additionally, serum uric acid and total cholesterol levels were not
significantly different between the two biopsies (Fig. 1E and F).
Notably, proteinuria decreased gradually to normal
level at 5 months in patient no. 2 who received the combined
therapy with a low-dose of PDN, TwHF and AZA. The patient
discontinued immunosuppressive treatment at 9 months and
proteinuria relapsed severely at 28 months. Although
immunosuppressants were administered again following relapse,
proteinuria was not alleviated until the second biopsy at 50.5
months.
Pathological data
The intensity of glomerular IgA and C3 deposits was
dramatically decreased at the second biopsy compared with that at
the first biopsy (P=0.004 and P=0.011, respectively); however,
glomerular IgA and/or C3 deposits remained present in the majority
of patients at the second biopsy (Table II). The intensity of other
immunoglobulin deposition was not significantly different between
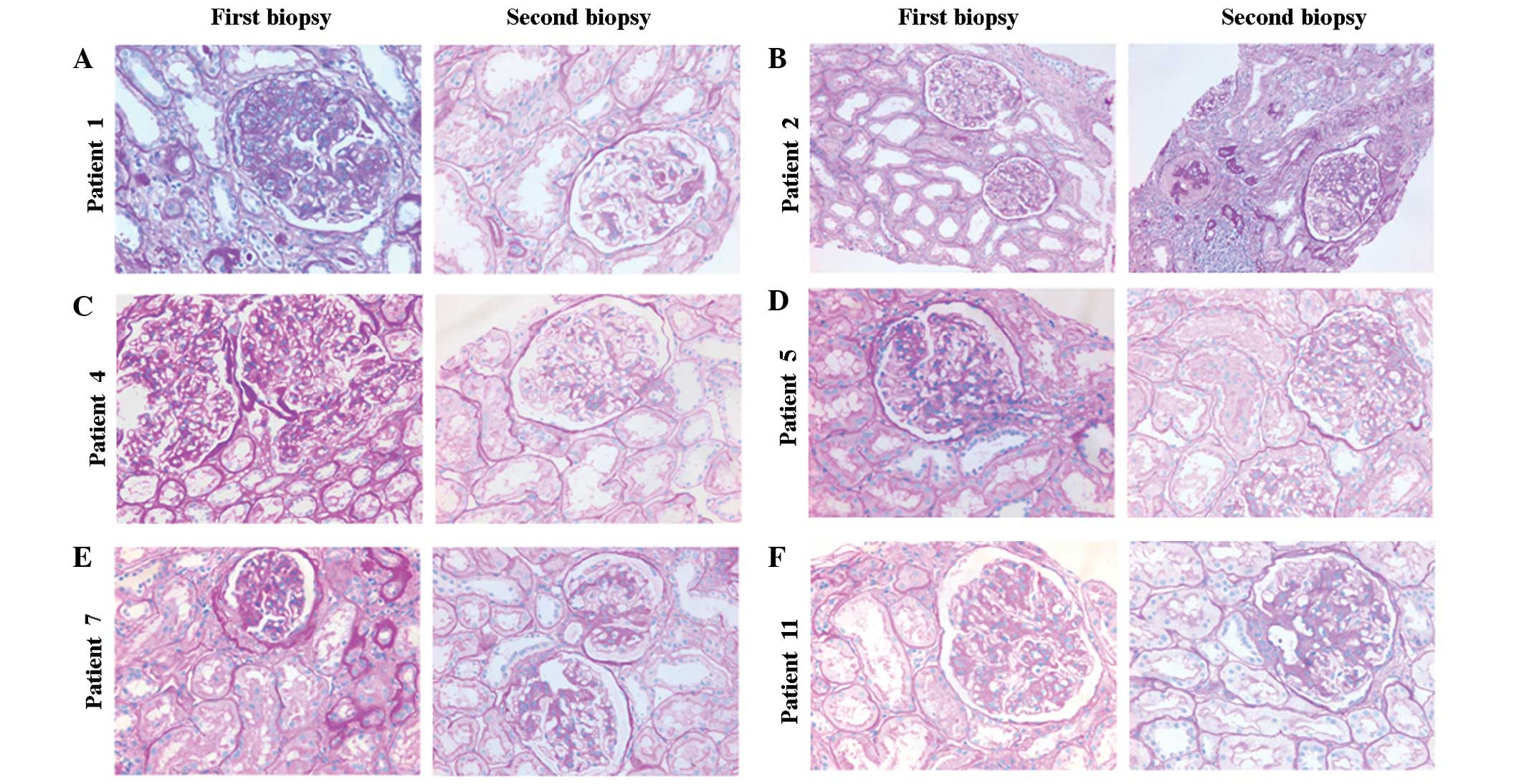
the two biopsies (data not shown). The acute lesions, such as
diffuse mesangial proliferation, cellular crescent formation or
interstitial mononuclear cell infiltrates showed marked
amelioration in the majority of patients at the second biopsy
compared with that at the first (Fig.
2). In addition, chronic pathological damage, including
glomerular capsular adhesion, segmental glomerular sclerosis,
global sclerosis and the degree of interstitial fibrosis, did not
show progression in the majority of patients (Fig. 2). As indicated by the results in
Table II, the activity index
decreased significantly from 3.18±1.33 to 2.47±0.80 (P<0.05),
while the chronicity index remained unchanged (2.59±2.00 versus
2.76±1.89). Moreover, although the score of acute lesions
decreased, residual renal active lesions were identified in 12
patients who had almost complete remission of proteinuria at the
second renal biopsy. Histopathology was aggravated severely in
patient no. 2, observed as severe glomerular sclerosis and
interstitial fibrosis (Fig.
2B).
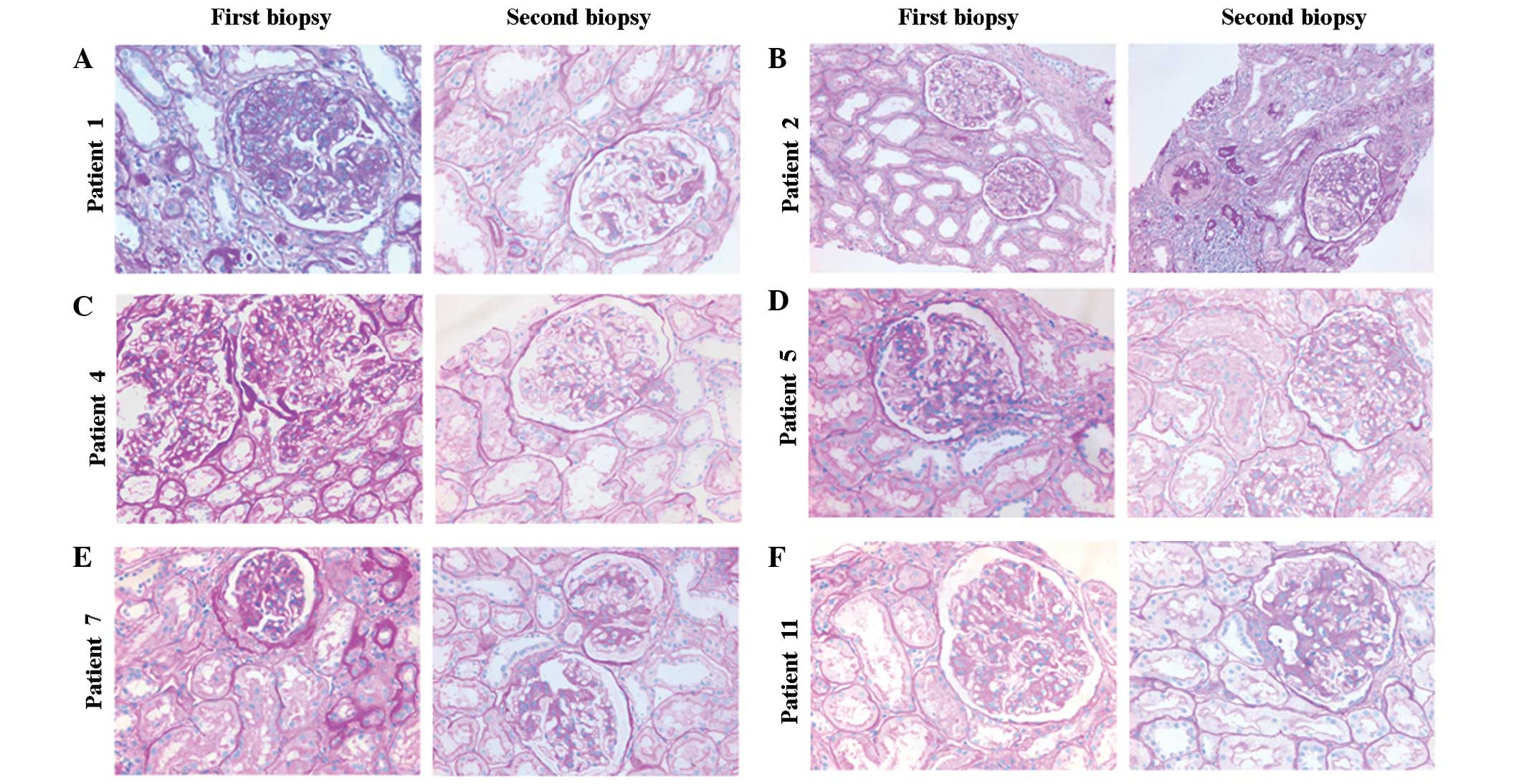 | Figure 2Representative histological sections
following immunomodulatory therapy in immunoglobulin A nephropathy.
All sections were stained with periodic acid-Schiff. (A) In patient
1, at the first renal biopsy moderate diffuse mesangial cell
proliferation, increased matrix deposition, adhesion to the
Bowman’s capsule and interstitial mononuclear cell infiltration
were observed. At the second renal biopsy, slight mesangial cell
proliferation and matrix expansion, but no adhesion to the Bowman’s
capsule or interstitial mononuclear cell infiltration were
observed. (B) In patient 2, compared with that at the first biopsy,
segmental glomerulosclerosis, interstitial infiltration, tubular
atrophy and interstitial fibrosis were observed in the second renal
biopsy. The histopathological features had deteriorated at the
second renal biopsy (magnification, ×200). (C,D,F) In patients 4, 5
and 11, the mesangial proliferation and matrix increases observed
in the first biopsy were ameliorated at the second renal biopsy. No
major changes of tubulointerstitial lesions were visible
(magnification, ×400). (E) In patient 7, at the first renal biopsy,
glomerular cell proliferation, matrix expansion, focal adhesion to
the Bowman’s capsule, tubular atrophy and interstitial fibrosis
were observed. At the second renal biopsy, mild mesangial cell
proliferation and adhesion to the Bowman’s capsule were detected.
(A,C–F) Histopathological changes were improved at the second renal
biopsy (magnification, ×400). |
 | Table IIHistological data of 17 patients with
IgAN who underwent a repeat renal biopsy. |
Table II
Histological data of 17 patients with
IgAN who underwent a repeat renal biopsy.
| | Intensity of
deposits | Index of renal
pathological lesions |
|---|
| |
|
|
|---|
| Patient | Biopsies | IgA | C3 | AS | CS | TS |
|---|
| 1 | First | 3 | 3 | 5 | 4 | 9 |
| Second | 2 | 2 | 4 | 2 | 6 |
| 2 | First | 2 | 0 | 2 | 0 | 2 |
| Second | 2 | 0 | 3 | 6 | 9 |
| 3 | First | 1 | 4 | 4 | 5 | 9 |
| Second | 1 | 1 | 2 | 3 | 5 |
| 4 | First | 1 | 0 | 2 | 1 | 3 |
| Second | 0.5 | 0 | 1 | 0 | 1 |
| 5 | First | 3 | 0.5 | 2 | 0 | 2 |
| Second | 2 | 0.5 | 3 | 1 | 4 |
| 6 | First | 4 | 4 | 3 | 5 | 8 |
| Second | 4 | 1 | 2 | 6 | 8 |
| 7 | First | 3 | 2 | 3 | 4 | 7 |
| Second | 3 | 2 | 3 | 3 | 7 |
| 8 | First | 3 | 2 | 6 | 3 | 9 |
| Second | 3 | 2 | 2 | 3 | 5 |
| 9 | First | 4 | 2 | 2 | 0 | 2 |
| Second | 2 | 1 | 2 | 4 | 6 |
| 10 | First | 3 | 2 | 5 | 5 | 10 |
| Second | 2 | 2 | 4 | 6 | 10 |
| 11 | First | 4 | 3 | 5 | 1 | 6 |
| Second | 2 | 2 | 3 | 1 | 4 |
| 12 | First | 2 | 0.5 | 2 | 1 | 3 |
| Second | 2 | 0 | 2 | 2 | 4 |
| 13 | First | 4 | 3 | 3 | 3 | 6 |
| Second | 3 | 3 | 2 | 2 | 4 |
| 14 | First | 2 | 0.5 | 2 | 6 | 8 |
| Second | 1 | 0 | 2 | 2 | 4 |
| 15 | First | 3 | 2 | 2 | 2 | 4 |
| Second | 3 | 2 | 2 | 1 | 3 |
| 16 | First | 3 | 0 | 3 | 3 | 6 |
| Second | 1 | 0 | 3 | 4 | 7 |
| 17 | First | 3 | 3 | 3 | 1 | 4 |
| Second | 2 | 2 | 2 | 1 | 3 |
Discussion
The benefits of corticosteroid monotherapy for the
treatment of IgAN have been elucidated in several studies (7,13,14)
and suggested in the KDIGO guidelines. However, an additional
randomly controlled trial conducted in Japan showed that
corticosteroid monotherapy was not beneficial for protecting kidney
function (15). AZA is not
suggested for the treatment of IgAN according to the KDIGO
guidelines; however, the addition of AZA to corticosteroids has
been shown to provide further benefits in the reduction of
proteinuria and the stabilization of renal function in patients
with IgAN, particularly in those who did not respond to
corticosteroid monotherapy (16).
Notably, Shima et al showed that glomerular IgA deposits
disappeared following combined therapy with corticosteroids and AZA
in children with IgAN showing diffuse mesangial proliferation
(17). TwHF, an extract from a
traditional Chinese medicine, has been widely used to treat
autoimmune and inflammatory diseases, including lupus nephritis and
rheumatoid arthritis (18–20). A previous study showed that Chinese
patients with IgAN benefited from TwHF treatment (21). In conclusion, the optimal treatment
strategy for IgAN remains controversial, despite the KIDIGO
guidelines.
In the past few years, prior to the publication of
the KDIGO guidelines for IgAN treatment, we applied an
individualized, low-dose and multi-drug immunosuppressive regimen
for the treatment of IgAN based on clinical and pathological
patterns, which was inspired from the idea of multi-target therapy
for lupus nephritis (22). All
patients in the present retrospective study received relatively
low-dose PDN treatment in order to avoid the obvious side-effects
of high-dose steroids. However, to compensate for the insufficient
immunosuppressive strength of low-dose PDN, AZA or a short course
of CTX was administered to those patients with more severe
proteinuria and/or active pathological changes. The dosage was
flexibly adjusted according to the condition of the patient. In
particular, the traditional Chinese medicine, TwHF, was also added
to the two immunosuppressants in the majority of patients, which
formed a triple immunosuppressive regimen. Notably, it was observed
that this immunosuppressive regimen significantly decreased
proteinuria, increased serum albumin levels and stabilized renal
function. Complete remission of proteinuria was achieved in the
majority of patients. However, it may be suggested that basic
therapy, such as ACEI and/or ARB usage and blood pressure control
may have also contributed to the reduction in proteinuria. However,
according to previous studies, basic RAS inhibition fails to
achieve complete remission of proteinuria in the majority of
patients with IgAN (23,24), which suggests that
immunosuppressive treatment may be important for proteinuria
remission in the patients in the present study. Furthermore, a
decline in the renal pathological activity index indicated that
renal inflammation was controlled at the second biopsy. The
chronicity index did not increase in the majority of patients,
suggesting that no additional active renal lesions developed into
chronic destruction. It has been suggested that the intensity of
glomerular IgA and C3 deposition may be associated with IgAN
progression (25,26) and the disappearance of IgA
indicates a better prognosis (17). In the present study, the quantities
of IgA and C3 deposits were significantly decreased, indicating
that the remission of proteinuria and improvement of renal
pathological lesions may be due to the minimizing of the abnormal
immune inflammatory response by the combined immunosuppressive
strategy, and may be independent to the basic therapy. This
supports the positive therapeutic effects of this immunosuppressive
regimen on IgAN. In addition, the side-effects were mild and
patients successfully tolerated the immunosuppressive regimen.
According to the KDIGO guidelines, the duration of
corticosteroid treatment is 6 months in patients with IgAN and
proteinuria of >1 g/day. However, the present study indicated
that although proteinuria was markedly decreased (as shown in
Fig. 1A), the deposits of IgA and
C3 and renal active lesions remained in the glomerulus following
combined immunosuppressive treatment for ~1 year in the majority of
patients. This indicated that complete remission of proteinuria did
not conform to the disappearance of histopathological activity.
Thus, a 6-month course of immunosuppressive therapy may not be
enough to completely control renal active lesions and a longer
course of treatment may be required for certain patients with IgAN.
Moreover, in patient no. 2, proteinuria relapsed following the
withdrawal of immunosuppressants. The patient had not achieved
complete remission of proteinuria and chronic histopathological
changes with significant deterioration were observed at the second
renal biopsy, which may have resulted from failure to continue
treatment. Therefore, remission of proteinuria may not be the only
decisive factor for withdrawing immunosuppressants in certain
patients with IgAN and additional factors, such as renal pathology
should be considered (12,27).
It is widely considered that proteinuria of <1
g/day indicates a favorable prognosis (3) and such patients require no specific
treatment, but should be kept under periodic review (28,29).
However, Usui et al (30)
demonstrated that certain patients with mild proteinuria (<0.5
g/day) progress to dialysis. In the present study, five patients
with an initial proteinuria of <1 g/day presented marked active
renal lesions at the first biopsy and were administered a very
low-dose of the multi-drug immunosuppressive regimen for ~1 year.
During follow-up, the patients achieved complete remission of
proteinuria and their renal pathological lesions improved. This
supports the idea that immunosuppressive therapy will bring
additional benefits for those patients with IgAN whose urinary
protein is <1 g/day, but show existing active renal lesions.
It should be acknowledged that there are limitations
in the present study, including the lack of a control group, a
small sample size, a retrospective study design and the relatively
short follow-up period. Therefore, the optimal drug-combined
regimen and duration of immunosuppressive therapy in patients with
IgAN requires further study.
In conclusion, the individualized low-dose
multi-drug immunosuppressive regimen significantly minimized
proteinuria, stabilized renal function and alleviated histological
lesions without inducing overt adverse effects in patients with
IgAN in the short-term follow-up. However, optimal treatment
strategies require further investigation. Notably, the results also
indicated that additional factors to proteinuria, particularly
renal pathological alterations, should be considered when
withdrawing immunosuppressant therapy from IgAN treatment. The
duration of immunosuppressive therapy on IgAN requires further
study.
Acknowledgements
This work was supported by Zhanjing city program for
tackling key problems in science and technology (No. 2013B01296)
and Youth Foundation of the Affiliated Hospital of Guangdong
Medical College (No. QK1301).
References
|
1
|
Floege J and Feehally J: IgA nephropathy:
recent developments. J Am Soc Nephrol. 11:2395–2403.
2000.PubMed/NCBI
|
|
2
|
Donadio JV and Grande JP: IgA nephropathy.
N Engl J Med. 347:738–748. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Reich HN, Troyanov S, Scholey JW and
Cattran DC; Toronto Glomerulonephritis Registry. Remission of
proteinuria improves prognosis in IgA nephropathy. J Am Soc
Nephrol. 18:3177–3183. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
D’Amico G: Natural history of idiopathic
IgA nephropathy and factors predictive of disease outcome. Semin
Nephrol. 24:179–196. 2004.PubMed/NCBI
|
|
5
|
Berthoux F, Mohey H, Laurent B, Mariat C,
Afiani A and Thibaudin L: Predicting the risk for dialysis or death
in IgA nephropathy. J Am Soc Nephrol. 22:752–761. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Coppo R, Cattran D, Roberts Ian SD, et al:
The new Oxford Clinico-Pathological Classification of IgA
nephropathy. Prilozi. 31:241–248. 2010.PubMed/NCBI
|
|
7
|
Pozzi C, Bolasco PG, Fogazzi GB, et al:
Corticosteroids in IgA nephropathy: a randomised controlled trial.
Lancet. 353:883–887. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Harmankaya O, Oztürk Y, Baştürk T, Obek A
and Kiliçarslan I: Efficacy of immunosuppressive therapy in IgA
nephropathy presenting with isolated hematuria. Int Urol Nephrol.
33:167–171. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
KDIGO: Kidney Disease: Improving Global
Outcomes. KDIGO Clinical Practice Guideline for Glomerulonephritis.
Kidney Int. 2(suppl): 209–217. 2012.
|
|
10
|
Manno C, Torres DD, Rossini M, Pesce F and
Schena FP: Randomized controlled clinical trial of corticosteroids
plus ACE-inhibitors with long-term follow-up in proteinuric IgA
nephropathy. Nephrol Dial Transplant. 24:3694–3701. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lv J, Zhang H, Chen Y, et al: Combination
therapy of prednisone and ACE inhibitor versus ACE-inhibitor
therapy alone in patients with IgA nephropathy: a randomized
controlled trial. Am J Kidney Dis. 53:26–32. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Andreoli SP and Bergstein JM: Treatment of
severe IgA nephropathy in children. Pediatr Nephrol. 3:248–253.
1989. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Tamura S, Ueki K, Ideura H, et al:
Corticosteroid therapy in patients with IgA nephropathy and
impaired renal function. Clin Nephrol. 55:192–195. 2001.PubMed/NCBI
|
|
14
|
Moriyama T, Honda K, Nitta K, Yumura W and
Nihei H: The effectiveness of steroid therapy for patients with
advanced IgA nephropathy and impaired renal function. Clin Exp
Nephrol. 8:237–242. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Katafuchi R, Ikeda K, Mizumasa T, et al:
Controlled, prospective trial of steroid treatment in IgA
nephropathy: a limitation of low-dose prednisolone therapy. Am J
Kidney Dis. 41:972–983. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Stangou M, Ekonomidou D, Giamalis P, et
al: Steroids and azathioprine in the treatment of IgA nephropathy.
Clin Exp Nephrol. 15:373–380. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Shima Y, Nakanishi K, Kamei K, et al:
Disappearance of glomerular IgA deposits in childhood IgA
nephropathy showing diffuse mesangial proliferation after 2 years
of combination/prednisolone therapy. Nephrol Dial Transplant.
26:163–169. 2011.
|
|
18
|
Qiu D and Kao PN: Immunosuppressive and
anti-inflammatory mechanisms of triptolide, the principal active
diterpenoid from the Chinese medicinal herb Tripterygium
wilfordii Hook. f Drugs R D. 4:1–18. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Lipsky PE and Tao XL: A potential new
treatment for rheumatoid arthritis: thunder god vine. Semin
Arthritis Rheum. 26:713–723. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Tao X and Lipsky PE: The Chinese
anti-inflammatory and immunosuppressive herbal remedy
Tripterygium wilfordii Hook F. Rheum Dis Clin North Am.
26:29–50. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Chen YZ, Gao Q, Zhao XZ, et al:
Meta-analysis of Tripterygium wilfordii Hook F in the
immunosuppressive treatment of IgA nephropathy. Intern Med.
49:2049–2055. 2010.PubMed/NCBI
|
|
22
|
Bao H, Liu ZH, Xie HL, Hu WX, Zhang HT and
Li LS: Successful treatment of class V+IV lupus nephritis with
multitarget therapy. J Am Soc Nephrol. 19:2001–2010. 2008.
|
|
23
|
Cheng J, Zhang X, Tian J, Li Q and Chen J:
Combination therapy an ACE inhibitor and an angiotensin receptor
blocker for IgA nephropathy: a meta-analysis. Int J Clin Pract.
66:917–923. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Cheng J, Zhang W, Zhang XH, He Q, Tao XJ
and Chen JH: ACEI/ARB therapy for IgA nephropathy: a meta analysis
of randomised controlled trials. Int J Clin Pract. 63:880–888.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
van Dixhoorn MG, Sato T, Muizert Y, van
Gijlswijk-Janssen DJ, De Heer E and Daha MR: Combined glomerular
deposition of polymeric rat IgA and IgG aggravates renal
inflammation. Kidney Int. 58:90–99. 2000.PubMed/NCBI
|
|
26
|
Komatsu H, Fujimoto S, Hara S, Sato Y,
Yamada K and Eto T: Relationship between serum IgA/C3 ratio and
progression of IgA nephropathy. Intern Med. 43:1023–1028. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Lee SM, Rao VM, Franklin WA, et al: IgA
nephropathy: morphologic predictors of progressive renal disease.
Hum Pathol. 13:314–322. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Glassock RJ: The treatment of IgA
nephropathy: status at the end of the millenium. J Nephrol.
12:288–296. 1999.PubMed/NCBI
|
|
29
|
Alexopoulos E: Treatment of primary IgA
nephropathy. Kidney Int. 65:341–355. 2004. View Article : Google Scholar
|
|
30
|
Usui J, Yamagata K, Kai H, et al:
Heterogeneity of prognosis in adult IgA nephropathy, especially
with mild proteinuria or mild histological features. Intern Med.
40:697–702. 2001. View Article : Google Scholar : PubMed/NCBI
|