Introduction
Fibrous dysplasia (FD) is a benign bone lesion
resulting from congenital dysplasia of bone. It is characterized by
fibro-osseous tissue replacing normal bone tissue (1,2). The
incidence rate of FD is difficult to estimate. However, it is not
rare in the clinic. It is reported that this disease accounts for
5–7% of clinical benign tumors (1,3,4).
According to its clinical characteristics, FD is divided into 4
types: monostotic type, polyostotic type, McCune-Albright syndrome
and Mazabraud syndrome (1,5). FD may occur at any age, without
gender tendency. In general, the mean age of patients with
monostotic FD presenting with clinical symptoms is 15 years old,
and the mean age of patients with polyostotic FD is 30 years old
(1). Common invasive skeletal
sites include the long bones, ribs, maxillofacial skeleton and
pelvis. The proximal femur is the most commonly affected site and
its main symptoms include pain, deformity and lameness which
seriously influence the functioning of affected limbs (6). Between April 2007 and January 2009,
the authors conducted surgical intervention in 15 patients with FD
of the proximal femur to correct deformity, eliminate symptoms,
recover function and prevent pathological fracture according to
symptoms and lesion size (7) in
order to relieve pain and recover activity. During follow-up,
efficacy for all patients was satisfactory.
Patients and methods
General data
Among the 15 cases, there were 9 males and 6
females, and their ages ranged from 16 to 32 years old. Among them,
1 case was 16 years old and 14 cases were between 18 and 32 years
old. The mean age was 25 years old. Twelve cases presented with
unilateral lesions and 3 cases presented with bilateral lesions. In
addition, 12 cases were monostotic, and 3 cases were polyostotic.
Among the 15 cases, 2 cases of FD in the proximal femur were
accompanied by shepherd’s crook deformity. The collodiaphysial
angles were 80 and 100°, and the femur lengths were 5 and 3 cm
shorter than the contra-lateral length, respectively. The disease
courses ranged from 2 months to 16 years, and the mean was 2 years.
All presented with hip pain, 10 cases were able to walk without the
support of crutches, 3 cases required the support of crutches to
walk, the gaits of 6 patients were normal, and there was no history
of surgical treatment of pathological fractures. The patients had
no endocrine disturbances and X-ray, CT and MRI examinations were
conducted prior to surgery. Lesion ranges were all >50% of the
femoral medullary cavity: 3 cases involved the partial head of the
femur, 15 cases involved the trochanter and 3 cases involved
polyostotic lesions in ipsilateral ilia and tibiae. The
postoperative pathological results all presented FD and 4 cases
also had bone cysts. This study was conducted in accordance with
the Declaration of Helsinki and with approval from the Ethics
Committee of Xi’an Red Cross Hospital (Xi’an, China). Written
informed consent was obtained from all participants.
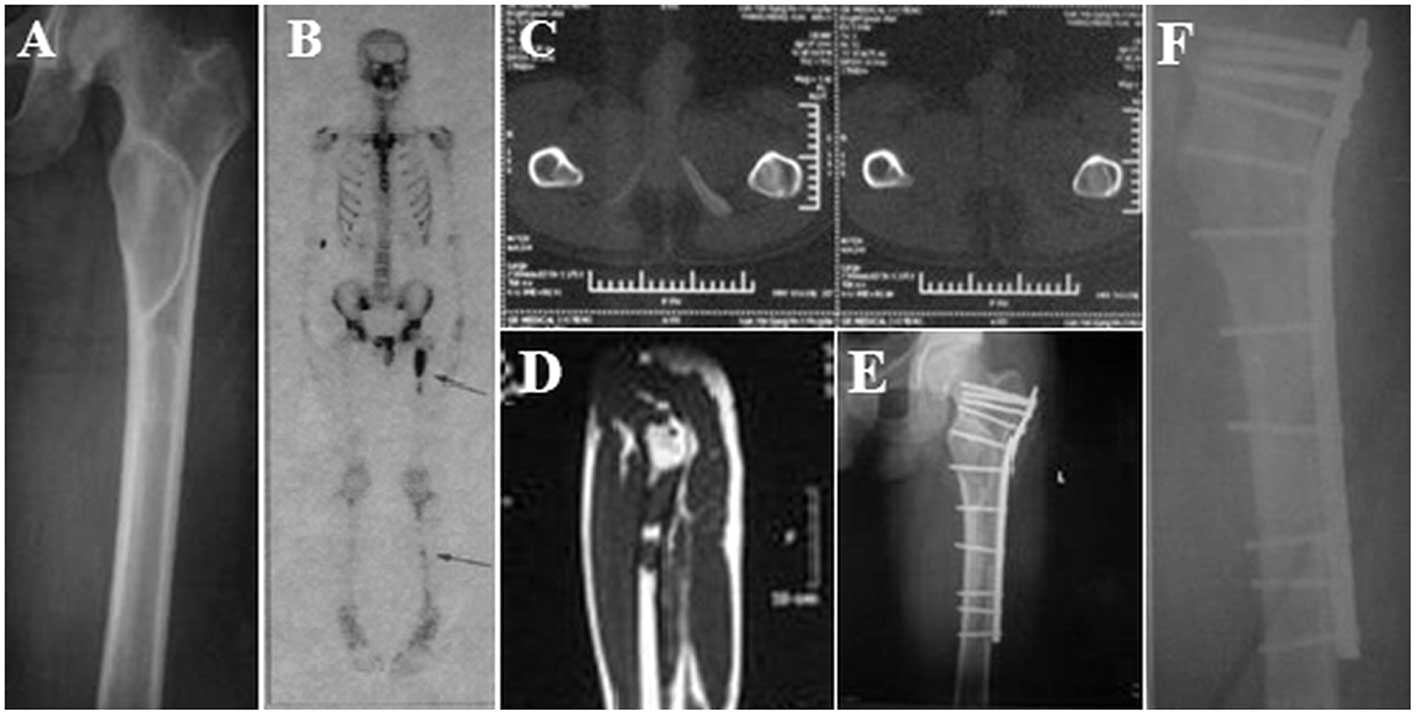
Internal fixation following curettage and
bone grafting
The patients were placed in a supine position, the
buttock of the affected side was cushioned and the proximal femur
was exposed by approach from the hip and lateral upper femur. A
window was opened at the anterolateral of the proximal femur FD
lesions, and intramedullary gravel-like lesion tissues were removed
with a curet under direct vision and were sent for pathological
biopsy. The remaining tissues were washed, cauterized with an
electrotome and soaked in 95% alcohol. A large block of autologous
iliac bone (structural bone graft; Hubei Lianjie Company, Wuhan,
China) was grafted at the femoral neck defect following curettage
to improve the stability of internal fixation screws using iliac,
and have better effects of repairing defects for autologous bone.
(Fig. 1). For patients with an
open osteoepiphyseal line, internal fixation of the anatomical
plate was conducted in such a way as to avoid damaging the
epiphyseal line.
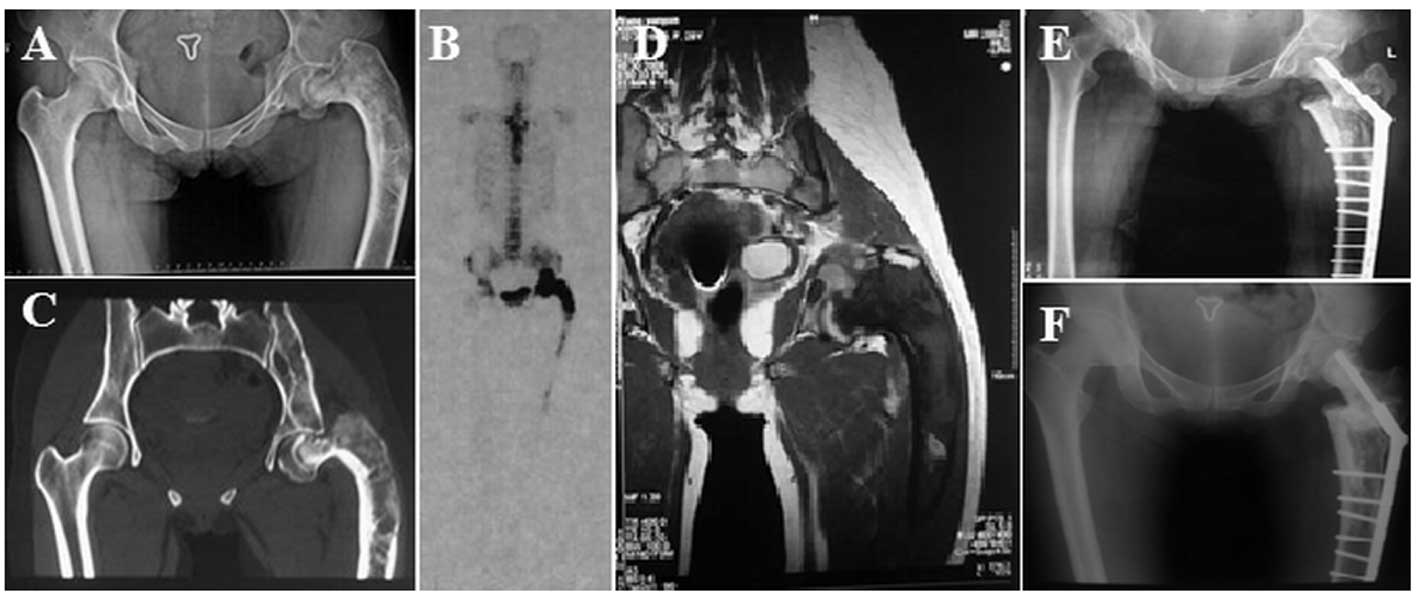
Osteotomy and internal fixation following
curettage and bone grafting
For 2 patients with FD in the proximal femur
accompanied by shepherd’s crook deformity, lesion tissues were
removed with a curet under direct vision. After the remaining
tissues had been cauterized with an electrotome and soaked in 95%
alcohol, an allogeneic artificial bone was grafted by impaction.
Valgus osteotomy was conducted in the lateral wedge nearby
subtrochanteric femoral deformity vertex to relax gluteus medius
and surrounding contractile tissues. After correcting the hip varus
deformity or shepherd’s crook deformity and femoral axis rotational
deformity, the 9-well dynamic hip screw (DHS) fixation was
conducted (Fig. 2).
Postoperative treatment
Long contraction exercises of the quadriceps
femoris muscle and passive movement of the hip and knee joints
began 24 h after surgery. Patients receiving the internal fixation
after lesion curettage and impaction grafting were able to walk
with the support of crutches at 8 weeks after surgery. For patients
with FD in the proximal femur accompanied by shepherd’s crook
deformity receiving osteotomy, internal fixation following
curettage and bone grafting, the hip and knee joints were gradually
unbent from the position of hip and knee flexion in order to avoid
stretching the sciatic nerve following surgery. After 4 months,
these patients were gradually able to walk with the support of
crutches and they could walk without support of crutches after 10
months. In addition, postoperative follow-up and X-ray examination
were conducted regularly.
Results
FD is confirmed by intraoperative
histological examination of the excised specimens
All patients were followed up for 12–32 months, and
postoperative incisions were healed in first grade healing.
Following curettage and bone grafting, pain was relieved, 13
patients did not present postoperative recurrent lesions and no
internal fixation became loose in the internal fixation group. In
the bone grafting area, local bone resorption was visible at the
3rd month after surgery. From 8 to 12 months after surgery, the
bones in the bone grafting area were healed, pain had disappeared,
hip joint function was recovered and gaits were nearly normal. For
the 2 patients with shepherd’s crook deformity in the proximal
femur who received an orthopedic procedure following osteotomy, the
collodiaphysial angle was recovered and femur length was increased
by 3 or 4 cm. At the 4th month after surgery, patients were able to
walk with the support of crutches, the pain had disappeared and hip
joint function was recovered. In addition, all patients experienced
no infection, re-fracture or progression of deformity, and no focus
recurred during follow-up visits.
Discussion
The development of FD lesions occurs at all stages
of the bone formation and growth process, and is most likely to
occur in the proximal femur. The treatment of foci at this site is
more difficult. Body weight and mechanical stretching of muscle may
cause stress and weaken bones, easily leading to fractures and
deformity. In addition, repeated fractures may exacerbate the
deformity. Among patients with multiple FD, a long bone usually
fractures due to stress and thus bends to form a shepherd’s crook
deformity (1). The age, focus size
and behavior of the patient all influence the selection of a
therapeutic regimen. For young patients, particularly patients
younger than 12 years old, lesion symptoms prior to skeletal
maturation are active, therefore the efficacy of surgical
intervention is poor and the lesion is frequently recurrent or the
nature of the lesion readily changes. We used oral bisphosphonates
and followed up these patients (8). For polyostotic foci, lesions are
likely to progress throughout adulthood, and the focus recurrence
rate after curettage and bone grafting is higher. In this study,
only 1 case was younger than 18 years old. According to the
proximal femur symptoms and focus size, it is usually necessary to
perform surgical intervention to relieve pain and recover activity.
The purpose of surgery is to correct deformity, eliminate symptoms,
recover function and prevent pathological fracture (7).
Lesion curettage and bone grafting is the main
method of treating FD in the proximal femur, and highlights the
lesion sites opening bone window method for the thorough removal of
foci and applies electrosurgical cautery and 95% alcohol soaking
for 20 min, which reduces the possibility of recurrence. Since we
observed that bone resorption usually occurred at 3 months
following focus curettage and allograft bone implantation, we used
an impaction grafting technique to increase the bone density of the
hollow bone graft. In general, there is a fracture risk following
lesion curettage and the initial structural support role may be
obtained by impaction grafting at the defect site following
proximal femur lesion curettage. However, the bone graft will lose
its structural strength as the bone bonding process progresses. The
additional application of internal fixation may provide a strong
mechanical support for the reconstructed defect bone to obtain
early stability, which facilitates maintenance of gravity line of
lower limb and the early ambulation of patients (without load or
with partial load). There are numerous optional internal fixation
methods (1,8–11).
According to lesion range and surrounding bone quality, we used
internal fixation with DHS/anatomical plates. For patients with an
open osteoepiphyseal line, the internal fixation of the anatomical
plate was conducted in such a way as to avoid damaging the
epiphyseal line.
Among the 13 patients in the internal fixation group
following curettage and bone grafting, pain was relieved, no case
presented with postoperative recurrent lesions and no internal
fixation became loose. At 3 months after surgery, local bone
resorption was visible in the bone grafting area of 4 cases. At
8–12 months after surgery, the bones in the bone grafting area were
healed, the myelocoele was unobstructed, pain disappeared, hip
joint function was recovered and gaits were nearly normal.
Among the patients with multiple FD, a long bone
usually fractures due to stress and thus bends into a shepherd’s
crook deformity (2,12,13).
The main symptoms of FD include pain of the affected hip,
deformity, lameness and shortening of the affected limb. The
purpose of the treatment is to obtain a normal gait and relieve the
pain caused by secondary pathological fractures. However,
orthopedic malformation is a challenge in surgical treatment
(9–11,14).
In this study, 2 cases of FD in the proximal femur were accompanied
by shepherd’s crook deformity. The collodiaphysial angles were 80
and 100°, and femur lengths were 5 and 3 cm shorter than the
contra-lateral length, respectively. The disease courses were 16
and 9 years, respectively. Both presented with hip deformity, pain
and lameness. Under direct vision, an allogeneic artificial bone
was grafted by impaction, and valgus osteotomy was conducted in the
lateral wedge nearby subtrochanteric femoral deformity vertex to
relax the gluteus medius and surrounding contractile tissues. After
correcting the hip varus deformity or shepherd’s crook deformity
and femoral axis rotational deformity, the 9-well DHS fixation was
conducted to recover the collodiaphysial angle and femur length.
Following surgery, the hip and knee joints were gradually unbent
from the position of hip and knee flexion in order to avoid sciatic
nerve stretch, the deformity was corrected and pain disappeared. It
was observed that due to a larger bone graft mass, postoperative
bone graft capacity was poor. At the 3rd month after surgery, there
was a small amount of bone resorption at the grafting site. The
patients were able to walk with the support of crutches 4 months
after surgery and normally walk without the support of crutches
after 10 months, the pain had disappeared and no deformity was
observed. The purpose of the surgery was achieved and a good
treatment efficacy was obtained.
For FD in the proximal femur, intralesional
curettage and bone grafting is the main treatment mode (9,15).
For bone defects following focus curettage, it is feasible to
select autologous bone or allogeneic bone as the filling according
to different situations. However, the issue remains a subject of
debate. Stephenson et al(16) suggest that only the method of
curettage and bone grafting is able to obtain a favorable result
for patients older than 18 years old. However, Enneking and Gearen
(17) reported that after focus
curettage and autogenous cancellous bone transplantation were
conducted for patients with FD in the proximal femur, the
transplanted autogenous cancellous bone was completely replaced by
hypogenetic bone tissue, tumors were likely to be recurrent and it
was not possible to obtain a satisfactory efficacy, whereas,
following the transplantion of autologous fibula into control
cases, a satisfactory efficacy was obtained (18). The likely cause is that the
cortical bone graft is rarely or slowly replaced by host bone and
may be maintained longer. Therefore, it is more appropriate for FD
treatment than an autologous bone graft. Certain scholars (19) suggest that the combination of focus
curettage and cancellous bone or cortical bone grafting is not
superior to simple osteotomy in FD treatment, while an autologous
bone graft with blood vessels is not absorbed by the host bone
(20). We suggest that as long as
no further expansion of the tumor range or orthopedic failure
occurs, it is acceptable for FD in the proximal femur following
focus curettage, regardless of the bone graft material.
In conclusion, it is necessary to proficiently
interpret the indications, conduct observations, administer oral
bisphosphonates and perform curettage and bone grafting, internal
fixation and orthopedic treatment of deformities in FD treatment.
In addition, further clinical observations regarding the selection
and application of bone graft materials are required.
References
|
1.
|
DiCaprio MR and Enneking WF: Fibrous
dysplasia. Pathophysiology, evaluation, and treatment. J Bone Joint
Surg Am. 87:1848–1864. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Harris WH, Dudley HR Jr and Barry RJ: The
natural history of fibrous dysplasia. An orthopaedic, pathological,
and roentgenographic study. J Bone Joint Surg Am. 44:207–233.
1962.PubMed/NCBI
|
|
3.
|
Coley BL: Neoplasms of Bone and Related
Conditions: Etiology, Pathogenesis, Diagnosis and Treatment. 2nd
edition. Paul B. Hober, Inc.; New York: 484. 1960
|
|
4.
|
Campanacci M: Bone and Soft Tissue Tumors:
Clinical Features, Imaging, Pathology and Treatment. 2nd edition.
Springer; New York: pp. 88–101. 1999
|
|
5.
|
Endres S and Wilke A: Fibrous dysplasia -
differential diagnosis of cystic lesions in the proximal femur: a
case report. Cases J. 2:26–30. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Stanton RP, Ippolito E, Springfield D,
Lindaman L, Wientroub S and Leet A: The surgical management of
fibrous dysplasia of bone. Orphanet J Rare Dis. 7(Suppl 1): S1–S9.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Ippolito E, Bray EW, Corsi A, et al:
Natural history and treatment of fibrous dysplasia of bone: a
multicenter clinicopathologic study promoted by the European
Pediatric Orthopaedic Society. J Pediatr Orthop B. 12:155–177.
2003.
|
|
8.
|
Chapurlat RD, Hugueny P, Delmas PD and
Meunier PJ: Treatment of fibrous dysplasia of bone with intravenous
pamidronate: long-term effectiveness and evaluation of predictors
of response to treatment. Bone. 35:235–242. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Onoda S, Hatori M, Yamada N, Hosaka M and
Kokubun S: A two-stage surgery for severe femoral neck deformity
due to fibrous dysplasia: a case report. Ups J Med Sci.
109:123–130. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Chen WJ, Chen WM, Chiang CC, Huang CK,
Chen TH and Lo WH: Shepherd’s crook deformity of polyostotic
fibrous dysplasia treated with corrective osteotomy and dynamic hip
screw. J Chin Med Assoc. 68:343–346. 2005.
|
|
11.
|
Jung ST, Chung JY, Seo HY, Bae BH and Lim
KY: Multiple osteotomies and intramedullary nailing with neck
cross-pinning for shepherd’s crook deformity in polyostotic fibrous
dysplasia: 7 femurs with a minimum of 2 years follow-up. Acta
Orthop. 77:469–473. 2006.PubMed/NCBI
|
|
12.
|
Funk FJ Jr and Wells RE: Hip problems in
fibrous dysplasia. Clin Orthop Relat Res. 90:77–82. 1973.PubMed/NCBI
|
|
13.
|
Grabias SL and Campbell CJ: Fibrous
dysplasia. Orthop Clin North Am. 8:771–783. 1977.
|
|
14.
|
Kataria H, Sharma N and Kanojia RK:
One-stage osteotomy and fixation using a long proximal femoral nail
and fibular graft to correct a severe shepherd’s crook deformity in
a patient with fibrous dysplasia: a case report. J Orthop Surg
(Hong Kong). 17:245–247. 2009.PubMed/NCBI
|
|
15.
|
Nakashima Y, Kotoura Y, Nagashima T,
Yamamuro T and Hamashima Y: Monostotic fibrous dysplasia in the
femoral neck. A clinicopathologic study. Clin Orthop Relat Res.
191:242–248. 1984.PubMed/NCBI
|
|
16.
|
Stephenson RB, London MD, Hankin FM and
Kaufer H: Fibrous dysplasia = An analysis of options for treatment.
J Bone Joint Surg Am. 69:400–409. 1987.
|
|
17.
|
Enneking WF and Gearen PF: Fibrous
dysplasia of the femoral neck. Treatment by cortical bone-grafting.
J Bone Joint Surg Am. 68:1415–1422. 1986.PubMed/NCBI
|
|
18.
|
George B, Abudu A, Grimer RJ, Carter SR
and Tillman RM: The treatment of benign lesions of the proximal
femur with non-vascularised autologous fibular strut grafts. J Bone
Joint Surg Br. 90:648–651. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Guille JT, Kumar SJ and MacEwen GD:
Fibrous dysplasia of the proximal part of the femur. Long-term
results of curettage and bone-grafting and mechanical realignment.
J Bone Joint Surg Am. 80:648–658. 1998.PubMed/NCBI
|
|
20.
|
Perea-Tortosa D, García-López A,
Saura-Sánchez E and Aguirre-Pastor A: Treatment of fibrous
dysplasia of the proximal femur by means of pedicled iliac crest
bone graft: a case report. Microsurgery. 31:56–58. 2011. View Article : Google Scholar : PubMed/NCBI
|