Introduction
Avulsion refers to the violent separation of skin
and soft tissue from muscle and bone tissue (1), and the wound closure of avulsion
injuries is a complex surgical issue. The wound healing is highly
challenging, particularly when accompanied by open wounds and
vascular injury of the extremities. This is due to such injuries
being associated with hypovolemic (or traumatic) shock, the
exposure of important structures (nerves, tendons, blood vessels,
etc.), serious contamination of wounds and severe combined wound
injuries, as well as other factors. All the aforementioned factors
may enhance the risk of first-line wound healing and thus cause
failure of the surgery. Therefore, the thorough removal of
devitalized tissue, fracture fixation and the appropriate use of
blood tissue for covering the wound all form the basis of wound
healing (2–4).
Xenogenic (porcine) acellular dermal matrix (XADM)
is prepared by removing all the layers of the skin epidermis and
all the cellular components of the dermis, while retaining the
dermal collagen composition and basic structure, as well as the
basement membrane components. The rejection of a skin graft is
primarily caused by cell-mediated immunity. Therefore, such a
matrix causes hardly any host rejection response and may induce
normal tissue remodeling, on the condition that strong immunogenic
cell components are removed from the matrix (5). An acellular biological covering
demonstrates good air permeability, good adhesion to the wound and
reduces the amount of exudate and bleeding, in addition to having a
certain softness. In addition, such a covering is not easily broken
and does not undergo significant water-loss or shrinking, which is
quite convenient, particularly when the covering is applied to
uneven or large bending wounds. The biofilm matrix forms a barrier
that effectively isolates the wound, thus reducing the possibility
of bacterial infection, providing a moist environment for the
wound, promoting the migration of epithelial cells, inducing host
fibroblast and endothelial cell proliferation, and promoting the
ordered ingrowth of capillaries and rearrangement of the collagen
fibers (6). Furthermore, the
covering reduces the loss of moisture, calories, protein and
electrolytes from the wound and reduces the elevated metabolic
state, in addition to the systemic inflammatory response syndrome,
thus stabilizing the environment of the whole body (7–9).
XADM creates a local and suitable microenvironment for wound
healing. In such a relatively confined, moist microenvironment with
a suitable pH, necrotic tissues are enzymatically decomposed and
the physiological structures are restored. In addition, such an
environment promotes the rapid proliferation of fibroblasts and
endothelial cells, the growth of granulation tissue and the
vascularization of the wound to achieve optimum surgical
results.
It has been demonstrated that XADM is able to
effectively protect a wound when it is used in the treatment of
deep burn wounds following excision (10). XADM also reduces the loss of water,
proteins and electrolytes to prevent deep-degree expansion of the
wound. In the present study, a first-stage surgical debridement of
the wound and the application of XADM coverings, with secondary
stage wound-closure surgery were performed for the reparation of
extremities severely damaged by avulsion.
Materials and methods
General data of patients
A total of 56 patients with acute traumatic soft
tissue damage were enrolled in the Burn Unit of the People’s
Hospital of Xinjiang Uygur Autonomous Region for wound-repair
surgery (Urumqi, China) from May 2002 to May 2012. Of the patients,
46 cases were male and 10 were female and they were aged 26–42
years, with a mean age of 34.27±1.28 years. The time from injury to
hospital admission ranged from 4 h to 10 days. All patients
exhibited varying degrees of hypovolemic shock or symptoms of
septic shock (Table I). Based upon
the classification criteria of avulsion from Arnez et al
(1), these patients all had
injuries of circumferential multi-plane degloving, which are
classified as fourth-degree avulsions. The study was approved by
the ethics committee of The People’s Hospital of Xinjiang Uygur
Autonomous Region. Prior written and informed consent was obtained
from each patient.
 | Table IData of the patients (n=56). |
Table I
Data of the patients (n=56).
| Symptoms | Number of cases |
|---|
| Shock |
| Moderate or severe
hypovolemic | 39 |
| Early | 17 |
| Fractures |
| Open | 17 |
| Closed | 12 |
| Traumatic brain
injury | 8 |
| Thoraco-abdominal
injury |
| Liver and spleen
rupture | 5 |
| Pulmonary
contusion | 2 |
| Intestinal
perforation | 2 |
| Diaphragmatic
hernia | 1 |
| Urinary tract
trauma |
| Kidney
laceration | 2 |
| Urethral
rupture | 2 |
| Bladder injury | 1 |
| Injuries |
| Unilateral
extremity | 42 |
| Two or more physical
injuries | 14 |
Surgery
Prior to receiving any other treatments following
injury, the patients underwent infusion via intravenous access
following admission. A mixture of crystalloid and colloid was
infused. The wound was bandaged to prevent bleeding. The
contaminated, significantly necrotic tissues and ischemic tissues
were cleared away during the surgery, while physiological
structures affected by partial necrosis and vital vessels, nerves
and tendon tissues were retained as much as possible as these may
be used as stents during subsequent reconstructive surgery. The
wounds were covered with XADM, which was purchased from JiangSu
Unitrump Bio-medical Technology Co., Ltd. (Nantong, China). A
suction drainage tube was placed subcutaneously and the sterile
covering was gently placed and bandaged. The entire surgery time
was limited to 1–2 h. At 5–7 days after the first stage surgery,
the secondary stage surgery with thick flaps or an autologous skin
graft for wound closure was performed.
Results
Of the 56 patients, 47 cases who received an
autologous skin graft had their wounds repaired successfully. A
further six cases were treated with local flaps and three cases
were treated with axial flaps for wound repair. Of all the
patients, two cases underwent amputation due to irreparable damage
and three cases passed away due to acute renal failure and
hemorrhagic shock.
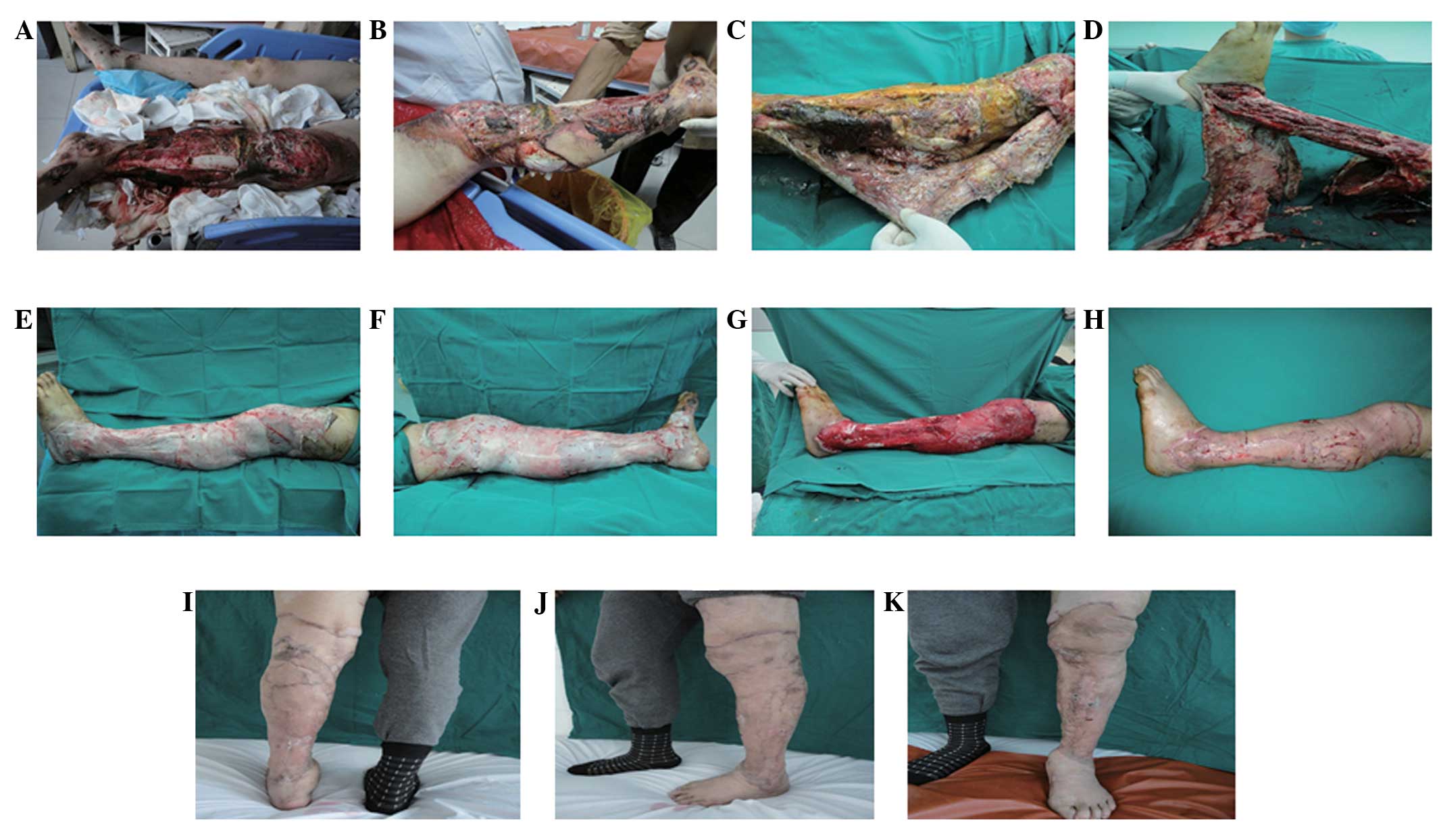
Case 1
A 19 year-old male was admitted to hospital 10 days
after a car accident trauma. The admission examination results were
as follows: Temperature, 39.8°C; heart rate, 124 beats/min;
respiration, 24 beats/min; and blood pressure, 75/50 mmHg. The
results of the laboratory examination were as follows: white blood
cell count, 3.5×109/l. An X-ray of the left lower
extremity indicated left tibia and fibula fractures. The diagnosis
concluded there was: i) Avulsion and severe infection of the skin
and soft tissues of the left lower extremity; ii) fracture of the
left tibia and fibula; and iii) septic shock. Visual examination
(Fig. 1) revealed a wide range of
soft tissue loss and wound contamination below the knee, to the
ankle of the left leg. In addition, it indicated a large area of
necrotic tissue and heavy purulent discharge, and the tibia and
knee joint cavities were partially exposed (Fig. 1A and B). Certain muscles of the
left leg were noted to be affected by infection and necrosis during
the surgery. A number of areas of sediment and purulent discharge
were observed on the wound (Fig.
1C). The muscles had automatically self-separated from the
gastrocnemius and soleus and the tibia and fibula after the surface
of the skin was cut (Fig. 1D).
Following debridement, the ruptured Achilles tendon was connected
with the gastrocnemius and soleus (Fig. 1E and F). The sections of the skin
and subcutaneous tissue affected by infection and necrosis were
removed and a large sheet of XADM was used to cover the wound.
Several holes were opened in the covering for drainage on the left
lateral leg (Fig. 1E) and left
medial leg (Fig. 1F). Following 10
days of XADM covering, the wound granulation tissue appeared fresh
with fine particles and the wound bed preparation was complete
(Fig. 1G). Wound closure was
achieved 12 days after the conduction of a large sheet edge
autologous skin graft of the left lower extremity (Fig. 1H). The follow-up was conducted one
year after the surgery and the shape and function of the left lower
extremity exhibited good recovery (Fig. 1I–K).
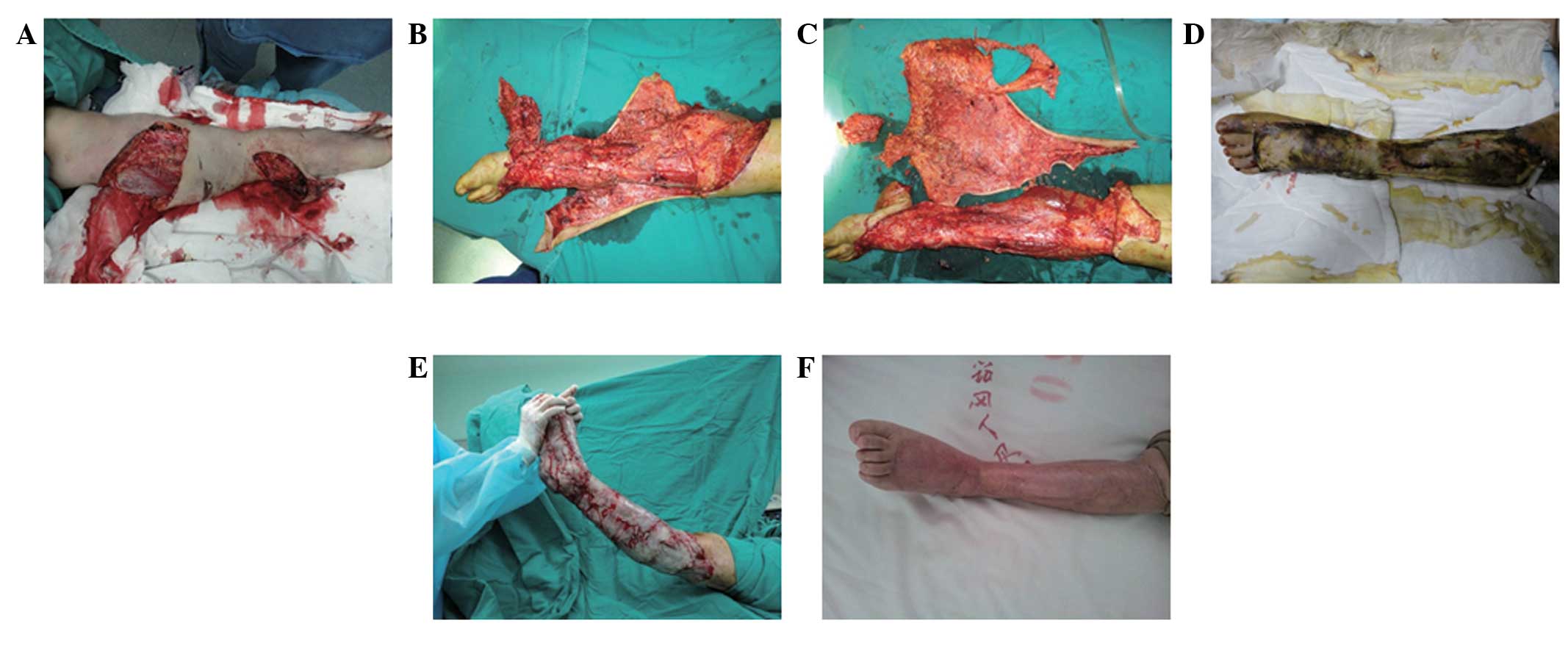
Case 2
A 45 year-old female was admitted to hospital 4 h
after a motor vehicle accident. The diagnosis was as follows: i)
Avulsion of the left lower extremity; ii) fracture of the left
tibia; and iii) hemorrhagic shock. As presented in Fig. 2, the skin and subcutaneous soft
tissue below the left knee were stripped off and separated from the
deep fascia (Fig. 2A and B). The
wound bed tissue became swollen following debridement. Furthermore,
the physiological structures and normal tissues were mixed.
Therefore, the success rate of a skin graft was likely to be
relatively low (Fig. 2C). A large
sheet of XADM was used to cover the wound and several holes were
opened in it for drainage (Fig. 2D and
E). The wound bed preparation was complete following 10 days of
debridement and an autologous skin graft was subsequently performed
for wound closure (Fig. 2F). The
follow-up was conducted one year after surgery. The shape and
function of the left lower extremity demonstrated good recovery
(Fig. 2G). These results indicate
that the XADM is useful in the wound healing of severely damaged
extremities.
Discussion
Gangrene, infection of avulsed tissues and even
certain serious complications such as systemic sepsis are likely to
occur if damaged wounds are not treated in a timely and effective
manner. Therefore, early-stage thorough debridement, drainage and
conservation of physiological structures are important in the
repair of avulsion injuries. In the present study, it was
demonstrated that XADM reduced the risk of emergency during surgery
and had good success rates for wound healing and patient treatment.
The use of XADM in the application of severely damaged wound
repair, to the best of our knowledge, has not been previously
reported.
In comparison with certain traditional techniques,
such as the Integra® artificial dermis (11–13)
and closed suction drainage techniques (14–16),
the cost of XADM is low. XADM is easily prepared from abundant
resources. Furthermore, the side-effects caused by XADM are usually
less than those of the Integra artificial dermis and the closed
suction drainage techniques. These advantages suggest that XADM may
be a good type of material for the treatment of severely damaged
wounds.
Acknowledgements
This study was supported by a grant from the Natural
Science Foundation of Xinjiang Uygur Autonomous Region (grant no.
2012211A090).
References
|
1
|
Arnez ZM, Khan U and Tyler MP:
Classification of soft-tissue degloving in limb trauma. J Plast
Reconstr Aesthet Surg. 63:1865–1869. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
MacCollum DW: Wringer arm - A report of
twenty-six cases. N Engl J Med. 218:549–554. 1938. View Article : Google Scholar
|
|
3
|
Bosse MJ, MacKenzie EJ, Kellam JF, et al:
An analysis of outcomes of reconstruction or amputation after
leg-threatening injuries. N Engl J Med. 347:1924–1931. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Naique SB, Pearse M and Nanchahal J:
Management of severe open tibial fractures: the need for combined
orthopaedic and plastic surgical treatment in specialist centres. J
Bone Joint Surg Br. 88:351–357. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sclafani AP, Romo T III, Jacono AA, et al:
Evaluation of acellular dermal graft (AlloDerm) sheet for soft
tissue augmentation: a 1-year follow-up of clinical observations
and histological findings. Arch Facial Plast Surg. 3:101–103.
2001.PubMed/NCBI
|
|
6
|
Richmond NA, Vivas AC and Kirsner RS:
Topical and biologic therapies for diabetic foot ulcers. Med Clin
North Am. 97:883–898. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wang ZX: Analysis of 21 cases of
electrical burn wounds treated with biologic dressing. Zhonghua
Shao Shang Za Zhi. 19:3252003.(In Chinese).
|
|
8
|
Lu SL, Liao ZJ, Xiang J, Wang ZY, Yang LY
and Shi JX: Clinical observation of the effect of tangential
excision within 24 postburn hours on the patients with deep partial
thickness burn. Zhonghua Shao Shang Za Zhi. 19:326–328. 2003.(In
Chinese).
|
|
9
|
Peng YZ: The new measures of the repairing
of massive deep burn wounds in large burn area. Zhonghua Shao Shang
Za Zhi. 19:321–322. 2003.(In Chinese).
|
|
10
|
Feng X, Tan J, Pan Y, et al: Control of
hypertrophic scar from inception by using xenogenic (porcine)
acellular dermal matrix (ADM) to cover deep second degree burn.
Burns. 32:293–298. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wolter TP, Noah EM and Pallua N: The use
of Integra in an upper extremity avulsion injury. Br J Plast Surg.
58:416–418. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Greig A, Angel J, Jones N and Healy C: The
use of Integra with a sensate fasciocutaneous pedicled flap for the
salvage reconstruction of a below knee amputation after pedestrian
vs train multi-planar degloving injury. J Plast Reconstr Aesthet
Surg. 63:e38–e40. 2010. View Article : Google Scholar
|
|
13
|
Iorio ML, Goldstein J, Adams M, et al:
Functional limb salvage in the diabetic patient: the use of a
collagen bilayer matrix and risk factors for amputation. Plast
Reconstr Surg. 127:260–267. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kanakaris NK, Thanasas C, Keramaris N,
Kontakis G, Granick MS and Giannoudis PV: The efficacy of negative
pressure wound therapy in the management of lower extremity trauma:
review of clinical evidence. Injury. 38(Suppl 5): S9–S18. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Krug E, Berg L, Lee C, et al:
Evidence-based recommendations for the use of negative pressure
wound therapy in traumatic wounds and reconstructive surgery: steps
towards an international consensus. Injury. 42(Suppl 1): S1–S12.
2011. View Article : Google Scholar
|
|
16
|
Dini M, Quercioli F, Mori A, Romano GF,
Lee AQ and Agostini T: Vacuum-assisted closure, dermal regeneration
template and degloved cryopreserved skin as useful tools in
subtotal degloving of the lower limb. Injury. 43:957–959. 2012.
View Article : Google Scholar : PubMed/NCBI
|