Introduction
Myocarditis refers to a variety of myocardial
inflammatory lesions. There are various causes of myocarditis, such
as infection as well as physical and chemical factors, which result
in myocardial damage of varying severity. The exact diagnosis of
myocarditis requires histopathological evidence, which is
predominantly obtained from endomyocardial biopsies. However, the
diagnostic significance of endomyocardial biopsies during treatment
is limited and is associated with certain surgical risks. Thus, it
is not regularly used in current clinical treatments. The clinical
manifestations of myocarditis differ due to variations in the
degree of damage; thus, myocarditis is challenging to diagnose. For
example, in a case where the history of viral infection is not
clear and markers of myocardial necrosis are normal, the diagnosis
of myocarditis is difficult to determine, regardless of clinical
signs of heart damage, such as heart failure and arrhythmia.
Therefore, a highly sensitive and accurate method is required to
obtain a definitive diagnosis of myocarditis (1).
At present, cardiovascular magnetic resonance
imaging (MRI) is an important tool in the noninvasive assessment of
patients with suspected myocarditis, specifically in the
differential diagnosis of acute coronary syndrome (ACS).
Cardiovascular MRI is used for diagnosing myocarditis, in addition
to guiding endomyocardial biopsies (2,3). The
present study examines the importance of cardiovascular MRI in the
diagnosis and differential diagnosis of myocarditis via a case
report. This study was conducted in accordance with the Declaration
of Helsinki and with approval from the Ethics Committee of Yangzhou
University (Yangzhou, China). Written informed consent was obtained
from the participant.
Case report
A 44-year-old male patient was admitted to a local
hospital one week subsequent to first presenting with symptoms of
dyspnea and shortness of breath accompanied by dizziness, without
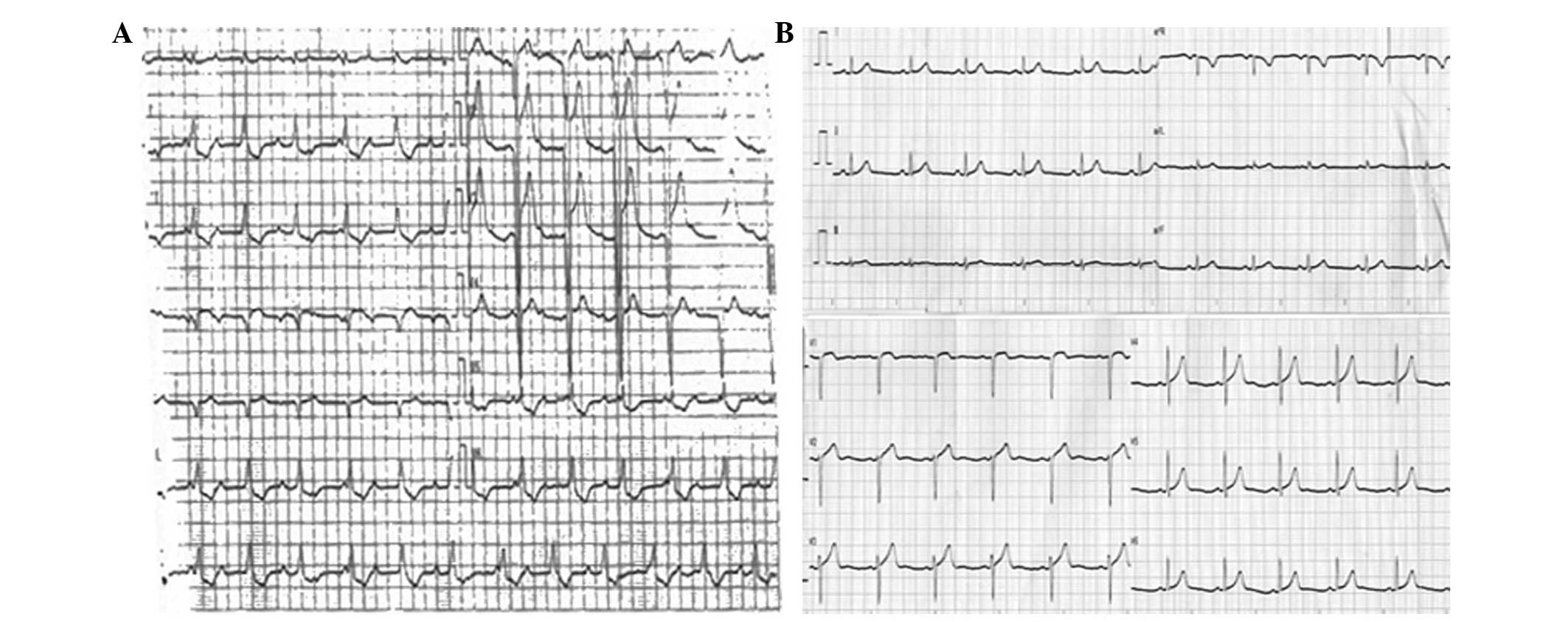
severe chest pain, amaurosis or syncope. The electrocardiogram
(ECG) demonstrated acute anteroseptal, right ventricular myocardial
infarction, ventricular escape and a third degree atrioventricular
block (AVB; Fig. 1A).
Echocardiography showed mild mitral regurgitation and indicated
that the cardiac structure, systolic function and wall motion were
without abnormalities. The left ventricular ejection fraction was
65%, and the levels of troponin (Tn) were significantly increased.
The patient was treated with an antiplatelet agent, an
anticoagulant agent, vasodilators and a plaque stabilizer, and was
transferred to the Northern Jiangsu People’s Hospital (Yangzhou,
China) upon stabilization of the condition. The patient had
previously been healthy, with a history of smoking (smoking index,
20 packs/year), but no history of hypertension, diabetes,
hyperlipidemia, alcoholism or coronary heart disease. Furthermore,
the patient had no recent history of upper respiratory tract
infection or gastroenteritis virus.
The results of the physical examination of the
patient were: Body temperature, 36.5°C; heart rate, 62 bpm;
respiratory rate, 18 breaths/min; and blood pressure, 120/70 mmHg.
The patient was conscious, exhibited no lip cyanosis and had a soft
neck with no jugular vein engorgement. Clear breath sounds were
heard from both lungs, with no rales and the patient exhibited a
negative hepatojugular reflux. In addition, no abnormal precordial
bulge was observed and the apex beat was at the fifth intercostal
space, 0.5 cm medial to the left midclavicular line. The heart rate
was regular. No pathological murmurs or pericardial friction rubs
were identified on auscultation and the patient was negative for
any peripheral vascular signs. The abdomen was soft, with no
tenderness or rebound tenderness, and no pitting edema was observed
on either of the lower extremities.
The Tn level was 0.053 ng/ml (normal range, 0–0.034
ng/ml). Urinalysis, thyroid function, liver and kidney function
were normal, as were the levels of blood glucose, blood lipids and
electrolytes. Four days following admission to hospital, coronary
angiography was conducted. This revealed normal openings and a
running area without calcification in a right-dominant type
coronary system in which: the left main coronary artery was without
stenosis and had a forward flow of thrombolysis in myocardial
infarction (TIMI) level 3; the left anterior descending had no
significant stenosis and a forward flow of TIMI level 3; the left
circumflex had no significant stenosis and a forward flow of TIMI
level 3; the first obtuse marginal openings had visible plaques and
a distal blood flow of TIMI level 3; and the right coronary artery
had no significant stenosis, a forward flow of TIMI level 3 and no
collateral circulation. On the basis of the imaging results, the
diagnosis was coronary atherosclerosis. Six days following
admission to hospital, the cardiac MRI revealed small, long T2
signals on the left anterior ventricular wall, which indicated
slight edema (Fig. 2). The patient
was prescribed bed rest to improve myocardial metabolism,
traditional Chinese medicine to alleviate heart qi deficiency, and
symptomatic treatment. The repeat ECG at 1 week after patient
discharge was identified to be normal (Fig. 1B) and the symptoms of the patient
had improved. Therefore, the patient was discharged.
Discussion
The cardiovascular MRI of the patient indicated
small, long T2 signals on the left ventricular anterior wall. This,
in combination with the clinical manifestations and auxiliary
examinations, such as the ECG, resulted in a diagnosis of
myocarditis. Myocardial edema is characteristic of myocardial
inflammation, myocardial necrosis and myocardial fibrosis, and can
be detected via cardiac MRI (4).
T2-weighted imaging is able to sensitively detect myocardial tissue
edema (5), which emits a high
intensity T2 signal. Furthermore, T2-weighted imaging characterizes
myocardial damage in the acute phase of eosinophilic myocarditis as
a signal of notably high intensity (6). Patients with myocarditis may present
with an extensive myocardial edema; thus, it may be necessary to
quantitatively analyze the signal intensity to improve the accuracy
of the diagnosis (7–9).
In 1999, the China Society of Cardiovascular Disease
developed the adult acute viral diagnostic reference criteria as
follows: i) Influenza, diarrhea and other viral infections occurred
within three weeks of a cardiac event. ii) Arrhythmias or ECG
changes observed within three weeks of infection, including the
following; a) ventricular tachycardia, AVB, sinoatrial or bundle
branch block, b) multi-source, paired ventricular premature atrial
or ventricular flutter or fibrillation, and c) two or more
horizontal or downward sloping lead ST segments ≥0.01 mV, ST
segment elevation or abnormal wall motion. iii) Myocardial injury
reference or wall motion abnormalities; a) significantly increased
troponin T (TnT), troponin I (TnI) and creatine kinase-MB levels,
b) ultrasound cardiography showing heart chamber enlargement, and
c) radionuclide examination confirming left ventricular systolic
heart function or diastolic dysfunction. iv) The etiological
criteria for diagnosing myocarditis are as follows: 1) A virus, a
virus gene fragment or a viral antigen in the endocardium,
myocardium, pericardium or a pericardial puncture. 2) Antibody
isotypes to the same pathogenic virus detected over two weeks in
the serum, with the first determination four-fold higher than the
second, or an antibody titer ≥640. 3) Virus-specific immunoglobulin
M levels ≥1:320 are considered positive. Patients are clinically
diagnosed with myocarditis if they exhibit any one of the criteria
in 1 and 2 or any two of the criteria in 1, 2 and 3, excluding
other symptoms. Etiological diagnosis is based on the clinical
diagnosis, which includes one of the items among the criteria in
iv. Severe viral myocarditis may be observed in patients with
Adams-Stokes syndrome, heart failure or ECG changes, including
myocardial infarction, cardiogenic shock, acute renal failure,
ventricular tachycardia with hypotension or cardiac pericarditis as
one or more of the manifestations.
The majority of clinicians consider that conducting
a endomyocardial biopsy is the gold standard for diagnosing
myocarditis. The Dallas criteria describes lymphocyte infiltration
with myocardial cell injury, but without myocardial ischemia; it
has a high degree of specificity but a sensitivity of only 10–22%
(American Heart Association, 1984). Endomyocardial biopsies result
in a greater number of complications, such as cardiac perforation
and cardiac tamponade occurring in ~0.1–0.5% of patients, in
addition to a variety of complications with an overall incidence
rate of ~6% (American Heart Association, 1984). The low sensitivity
and risks that are associated with performing endomyocardial
biopsies limit its use in the diagnosis of myocarditis; therefore,
it is unsuitable for numerous patients with myocarditis,
particularly those with mild myocarditis.
At present, cardiovascular MRI is an important tool
for the noninvasive assessment of patients with suspected
myocarditis (specifically in the differential diagnosis of ACS),
and is useful for guiding endomyocardial biopsies. Lurz et
al (10) identified that
cardiovascular MRI has a sensitivity of 81%, specificity of 71% and
accuracy of 81% for diagnosing acute myocarditis. The authors also
demonstrated that the sensitivity, specificity and accuracy of
cardiovascular MRI for diagnosing acute myocarditis were
significantly higher than for diagnosing chronic myocarditis.
Cardiac MRI is safe and reliable, and is capable of examining
cardiac structure and function and performing myocardial perfusion
scans in addition to other one-stop, accurate quantitative
evaluations. Cardiac MRI directly identifies the characteristic
pathological changes in myocardial tissue with a high
repeatability; thus, it has become an internationally accepted
cardiovascular imaging modality. In addition, cardiac MRI is highly
sensitive and moderately specific for diagnosing myocarditis. Focal
myocardial edema on T2-weighted imaging highlights the limitations
of high signal enhancement scanning, as it appeared to strengthen
with early myocardial involvement in delayed enhancement scanning.
The shape and position of the delayed enhancement aids with
distinguishing between the primary disease and ischemic
cardiomyopathy, with the former strengthening in the myocardium or
epicardium located in the subendocardial region. Focal myocardial
enhancement and segmental wall motion abnormalities that occur
simultaneously are indicative of myocarditis.
Cardiac MRI parameters exhibit differential
precision. The T2 rate (assessment of edema), general
myocardium-associated enhancement and late gadolinium enhancement
(LGE) are specific parameters for detecting irreversible myocardial
damage. Šramko et al (11)
demonstrated that early gadolinium enhancement had a sensitivity of
40%, specificity of 96% and accuracy of 76% for the diagnosis of
myocardial inflammation, whereas LGE had a sensitivity of 87%, a
specificity of 44% and accuracy of 60%. Delayed enhancement
scanning is of significant value in the diagnosis of myocarditis.
Safiullina et al (12)
investigated 51 patients with inflammatory cardiomyopathy and
observed myocardial areas of delayed enhancement in 20 patients. Di
Bella et al (13) reported
observations for 81 patients in whom acute myocarditis was
diagnosed by delayed contrast-enhanced MRI.
Patients with myocardial injury usually demonstrate
elevated markers, abnormal Q waves or ST segment changes in their
ECG. However, myocardial infarction and myocarditis are complex to
diagnose in atypical cases with no medical history or symptoms.
Furthermore, when diagnosing myocardial infarction in younger
patients, other diagnostic possibilities should be excluded. In
such patients, coronary angiography or coronary computed tomography
angiography are recommended to exclude coronary artery disease.
When the coronary arteries of a patient are healthy, cardiac MRI
may be considered, with signs of edema in T2-weighted imaging or
evident focal high signal enhancement enabling a definitive
diagnosis of myocarditis. Combined electrocardiography, coronary
angiography and magnetic resonance imaging is a favorable method
for the diagnosis of viral myocarditis, and it requires further
cases to confirm.
References
|
1
|
Park Y, Ahn SG, Ko A, et al:
Hypersensitivity myocarditis confirmed by cardiac magnetic
resonance imaging and endomyocardial biopsy. Korean J Intern Med.
29:236–240. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Shauer A, Gotsman I, Keren A, et al: Acute
viral myocarditis: current concepts in diagnosis and treatment. Isr
Med Assoc J. 15:180–185. 2013.PubMed/NCBI
|
|
3
|
Gutberlet M, Lücke C, Krieghoff C, et al:
MRI for myocarditis. Radiologe. 53:30–37. 2013.(In German).
|
|
4
|
Jeserich M, Brunner E, Kandolf R, et al:
Diagnosis of viral myocarditis by cardiac magnetic resonance and
viral genome detection in peripheral blood. Int J Cardiovasc
Imaging. 29:121–129. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Carbone I and Friedrich MG: Myocardial
edema imaging by cardiovascular magnetic resonance: current status
and future potential. Curr Cardiol Rep. 14:1–6. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Tani H, Amano Y, Tachi M, Machida T,
Mizuno K and Kumita S: T2-weighted and delayed enhancement MRI of
eosinophilic myocarditis: relationship with clinical phases and
global cardiac function. Jpn J Radiol. 30:824–831. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Abdel-Aty H, Boyé P, Zagrosek A, et al:
Diagnostic performance of cardiovascular magnetic resonance in
patients with suspected acute myocarditis: comparison of different
approaches. J Am Coll Cardiol. 45:1815–1822. 2005. View Article : Google Scholar
|
|
8
|
Gutberlet M, Spors B, Thoma T, et al:
Suspected chronic myocarditis at cardiac MR: diagnostic accuracy
and association with immunohistologically detected inflammation and
viral persistence. Radiology. 246:401–409. 2008. View Article : Google Scholar
|
|
9
|
Friedrich MG, Sechtem U, Schulz-Menger J,
et al; International Consensus Group on Cardiovascular Magnetic
Resonance in Myocarditis. Cardiovascular magnetic resonance in
myocarditis: A JACC White Paper. J Am Coll Cardiol. 53:1475–1487.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Lurz P, Eitel I, Adam J, et al: Diagnostic
performance of CMR imaging compared with EMB in patients with
suspected myocarditis. JACC Cardiovasc Imaging. 5:513–524. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Šramko M, Kubánek M, Tintěra J, et al:
Utility of combination of cardiac magnetic resonance imaging and
high-sensitivity cardiac troponin T assay in diagnosis of
inflammatory cardiomyopathy. Am J Cardiol. 111:258–264.
2013.PubMed/NCBI
|
|
12
|
Safiullina AA, Sharia MA, Narusov OIu,
Alaeva EN and Tereshchenko SN: Diagnostic capabilities of cardiac
magnetic resonance imaging in patients with inflammatory
cardiomyopathy: comparison of its results with endomyocardial
biopsy data and clinical picture. Ter Arkh. 85:22–28. 2013.(In
Russian).
|
|
13
|
Di Bella G, Florian A, Oreto L, et al:
Electrocardiographic findings and myocardial damage in acute
myocarditis detected by cardiac magnetic resonance. Clin Res
Cardiol. 101:617–624. 2012.PubMed/NCBI
|