Introduction
Atherosclerosis is a prevalent pathological process
that leads to coronary and cerebrovascular diseases, two major
causes of morbidity and mortality worldwide (1,2).
Atherosclerosis is a progressive disorder of the walls of large and
medium arteries, ranging from fatty streaks to atheromatous plaques
(3). Lifestyle modifications are
the first method of treatment, while medicines are usually the next
step in treating atherosclerosis, among which statins are the most
popular and widely prescribed (4).
However, in a number of susceptible individuals the available
medicine does not sufficiently prevent the progression of
atherosclerosis (5,6). There is thus an urgent requirement
for novel therapeutic strategies.
Abnormal lipid metabolism is a formally established,
and remains the most important, risk factor for atherosclerosis
(7). However, there are numerous
discrepancies in the expression of the clinical disease among
individuals with similar cholesterol levels (8–10).
Accumulating evidence has indicated that inflammation plays a
central role in atherogenesis (11–13).
Macrophages were the first inflammatory cells to be associated with
atherosclerosis (14). Thus far,
the majority of the known leukocytes have been reported to be
present in and to lead to atherosclerotic lesions (15). Cytokines are key factors during
acute and chronic inflammation (16–18).
The majority of these cytokines share common methods of action. The
intracellular signal transduction pathways include the nuclear
factor κB (NF-κB), Janus kinase/signal transducers and activators
of transcription (JAK/STAT) and mitogen-activated protein kinase
(MAPK) pathways (19–21). The generation of cytokine-deficient
animals has provided strong evidence that cytokines play a critical
role in atherosclerosis, i.e. interleukin
(IL)-1β−/−/apolipoprotein E−/− mice showed a
significant decrease in the severity of atherosclerotic lesions
compared with their IL-1β-expressing counterparts (22). Consistent with these findings,
cytokines such as C-reactive protein, tumor necrosis factor (TNF)-α
and IL-6 have been found to be associated with cardiovascular risk
(23–25).
The renin-angiotensin-aldosterone system (RAAS) also
plays a significant role in atherogenesis. Angiotensin II (AngII)
is a major effector of the RAAS, and evidence suggests that AngII
has significant proinflammatory activity (26). Blocking the effect of AngII by
angiotensin-converting enzyme inhibitors (ACEIs) or AngII receptor
blockers (ARBs) exerts an anti-inflammatory effect, which modifies
inflammatory molecules, including intercellular adhesion molecule-1
and vascular cell adhesion molecule-1, and prevents the development
of atherosclerosis in animal models (27,28).
Allium fistulosum is widely cultivated in
Southern China and has been used to treat a variety of diseases,
including the common cold and arthritis. Fistular onion stalk is
derived from A. fistulosum, and whether or not it modulates
atherosclerosis has yet to be elucidated. The present study aimed
to investigate the pharmacological effect of fistular onion stalk
on a rat atherosclerosis model and to determine whether an
anti-inflammatory mechanism is involved in this process.
Materials and methods
Preparation of fistular onion stalk
extract
The fresh fistular onion stalk was purchased from
from local farmers in Huangpi (Wuhan, China), and identified by
staff at Tongji Medical College (Huazhong University of Science and
Technology, Wuhan, China). Extracts were then prepared at Tongji
Medical College as described in a previous study (29). In brief, the white-sheath section
was isolated and homogenized. Following centrifugation, the
supernatant was filtered, frozen at −80°C and lyophilized for 24 h.
The dehydrated powder was then sent for supercritical extraction by
carbon dioxide, and the extraction was carried out with a
laboratory scale high-pressure extraction plant (Nantong Huaan
Supercritical Extraction Co., Ltd, Nantong, China). The mass of
sample in the extractor was at a pressure of 30 MPa and a
temperature of 50°C, and the carbon dioxide flow rate was 250–300
l/h. The separator conditions comprised a pressure of 8 MPa and a
temperature of 45°C. Extracts from the same batch were used for the
entire set of experiments.
Animals and groups
Male Sprague Dawley rats (age, 12 weeks; weight,
200–250 g) were purchased from and maintained at the Division of
Experimental Animals, Tongji Medical College. The care and use of
the animals was approved by the Animal Care and Use Committee of
Huazhong University of Science and Technology. Thirty rats were
randomly divided into three groups as follows: Vehicle treatment
plus non-atherosclerosis control (control, n=10), vehicle treatment
plus atherosclerosis (model, n=10) and fistular onion stalk extract
treatment plus atherosclerosis (treatment, n=10).
The atherosclerosis was induced by a high-fat diet
and vitamin D2 loading as previously described (30). The model group was fed with a
high-fat diet, which contained 83.3% normal food, 8% lard, 3%
cholesterin, 5% plantation white sugar, 0.2% propylthiouracil and
0.5% chleolate, for 16 weeks. Vitamin D2
(3×105 U/kg) was injected into each rat at the beginning
of the experiment. The treatment group was given the same diet, and
the fistular onion stalk extract was administered by gastric
perfusion (20 mg/kg) from the fifth week. The control group was fed
the basal diet.
The study protocol was approved by the institutional
review board of Wuhan No.1 Hospital, Huazhong University of Science
and Technology.
Histopathology examination
At the end of the 16th week, the rats were kept in a
fasted state for 8 h prior to anesthesia by 10% chloral hydrate
(0.3 ml/100 g). The rats were then sacrificed and the aortas were
separated, removed and cut open. A section of the aortas was
immediately sent for cryostat sectioning, and stained by oil red
for the demonstration of lipids. The other section was fixed in 4%
paraformaldehyde, embedded in paraffin, further sectioned and then
mounted on glass microscope slides. Pathological changes in the
aorta were determined by hematoxylin and eosin staining.
Atherosclerosis was analyzed in a blinded manner using four
cross-sections from each specimen at intervals of 40 μm.
Immunohistochemistry
Paraffin-embedded aortas were made into serial 5-μm
cross-sections. The sections were firstly deparaffinized and
rehydrated. Antigen retrieval was then performed by heating the
slides in a microwave oven in 0.1 M citrate buffer (pH 6.0) for 20
min. The endogenous peroxidase activity was blocked with 3%
hydrogen peroxide for 30 min. Subsequent to incubation with 2%
bovine serum albumin, the slides were incubated in a humid chamber
with the respective primary antibodies, at 4°C, overnight. The
following antibodies were used: Anti-AngII (H-002-12; Phoenix
Pharmaceuticals, Inc., Burlingame, CA, USA) at a dilution of 1:200,
anti-AngII type 1 receptor (AT1) (ADI-905-743; Enzo Life Sciences,
Exeter, UK) at a dilution of 1:500 and anti-AT2 (ADI-905-746; Enzo
Life Sciences) at a dilution of 1:500. The slides were then
incubated for 45 min at 37°C with horseradish peroxidase-conjugated
secondary antibody. Diaminobenzidine was used as the chromogen
substrate and Harris hematoxylin as the counterstain. Primary
antibodies were substituted with phosphate-buffered saline in the
negative controls. The expression was assessed semi-quantitatively
on a scale of 0–3, as follows: 0, negative; 1, weak intensity
staining; 2, medium intensity staining; and 3, strong intensity
staining. Evaluations were performed independently and in a blinded
manner by two pathologists.
Western blot analysis
Protein was extracted using lysis buffer and
quantified using the bicinchoninic acid method. Equal amounts of
protein from each sample were heated for 10 min at 95°C in sample
buffer and then resolved using SDS-PAGE gels and subsequently
transferred to polyvinylidene difluoride membranes by semi-dry
transfer. The membranes were blocked in a 5% milk solution and
incubated with primary antibody at 4°C overnight. The following
antibodies were used at a dilution of 1:1,000 :
Anti-phosphorylated-(p-)p65 (sc-101749), anti-p65 (sc-8008),
anti-p-stat3 (sc-135649), anti-stat3 (sc-8019), anti-p-p38
(sc-7973) and anti-p38 (sc-7149) (Santa Cruz Biotechnology, Inc.,
Santa Cruz, CA, USA). The anti-GAPDH antibody (ab9485; Abcam,
Cambridge, MA, USA) was used at a dilution of 1:2,500. The
membranes were then washed and incubated with horseradish
peroxidase-conjugated secondary antibody. The immunoreactivity was
detected by enhanced chemiluminescence. Images were captured and
quantified using National Institutes of Health (NIH) Image 1.61
software (NIH, Bethesda, MD, USA).
Quantitative polymerase chain reaction
(PCR)
The total RNA was isolated and reverse transcribed
(Applied Biosystems, Inc., Foster City, CA, USA). Quantitative
(q)PCR was then performed using an ABI 7900 System (Applied
Biosystems, Inc.) in the presence of SYBR Green (Applied
Biosystems, Inc.). The primer sequences are were follows: AngII
(forward): 5′-CCGCATTTAACTGCTCACACA-3′,
(reverse):5′-ATCATGTAGTAGAGAACAGGAATTGCTT-3′; AT1 (forward):
5′-GCAGCACTTCACTACCAAATGGGC-3′, (reverse)
5′-CAGGACAAAAGCAGGCTAGGGAGA-3′; AT2 (forward):
5′-GGAAGGTAGAACATACATTAAATG-3′, (reverse):
5′-AGAGAAACAGCAGCTAAAGAATT-3′. Target sequences were amplified at
95°C for 10 min, followed by 40 cycles of 95°C for 15 sec and 60°C
for 1 min. GAPDH was used as an endogenous normalization control.
All the assays were performed in triplicate. The fold change in
mRNA expression was determined according to the 2ΔΔCt
method.
ELISA
The affected aorta of the rats was obtained and sent
for the measurement of cytokine levels. The quantification was
determined using quantitative IL-1β, IL-6, monocyte chemoattractant
protein-1 (MCP-1) and TNF-α ELISA kits (RLB00, R6000B, MJE00 and
RTA00, respectively; R&D Systems, Minneapolis, MN, USA)
according to the manufacturer’s instructions. The results were
expressed using the optical density value of the tissue.
Statistical analysis
All data are presented as the mean ± standard
deviation. Statistical analyses were conducted using SPSS 13.0
software (SPSS, Inc., Chicago, IL, USA). The significance of
differences was calculated by a one-way analysis of variance test
followed by a least significant difference post hoc analysis. The
level of statistical significance was set at P<0.05.
Results
Fistular onion stalk extract prevents the
progression of atherosclerosis
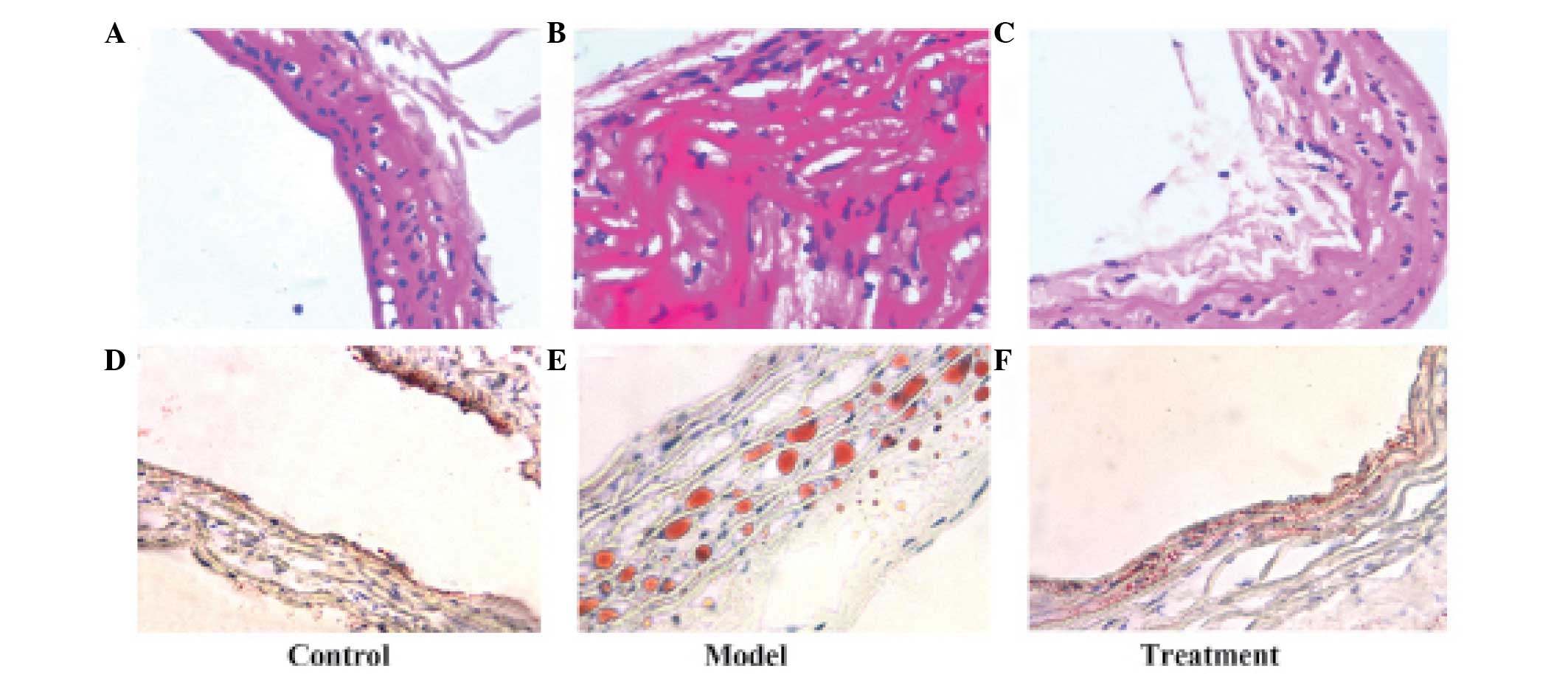
The lesion area in the transverse section of the
aorta was expressed as a percentage of the lesion to the total area
of the aortic tissue. No significant atherosclerotic lesions were
identified in the control group; however, the model rats exhibited
significantly more extensive lesions at the thoracic and abdominal
aortic regions. Evident endothelium damage, smooth muscle
proliferation and lymphocyte infiltration was observed (Fig. 1). Lesion formation at both
locations was significantly reduced after 12 weeks of treatment
(P<0.05). The average lesion area was 1.72, 64.7 and 24.9% for
the control, model and treatment groups, respectively (Fig. 1 and Table I). It was also revealed that
treatment with fistular onion stalk extract significantly reduced
lipidoses compared with the model group (P<0.05, Table I). Aortic cross-sections stained
for lipid lesions are shown in Fig.
1.
 | Table ILesion areas of the different groups
at the end of the experiment. |
Table I
Lesion areas of the different groups
at the end of the experiment.
| Group | Atherosclerotic
area (%) | Lipidoses area
(%) |
|---|
| Control | 1.72±0.61 | 0.85±0.35 |
| Model | 64.7±47.48a,b | 50.43±1.04a,b |
| Treatment | 24.9±66.07 | 4.19±1.07 |
Fistular onion stalk extract attenuates
levels of local inflammatory cytokines in aortic tissue
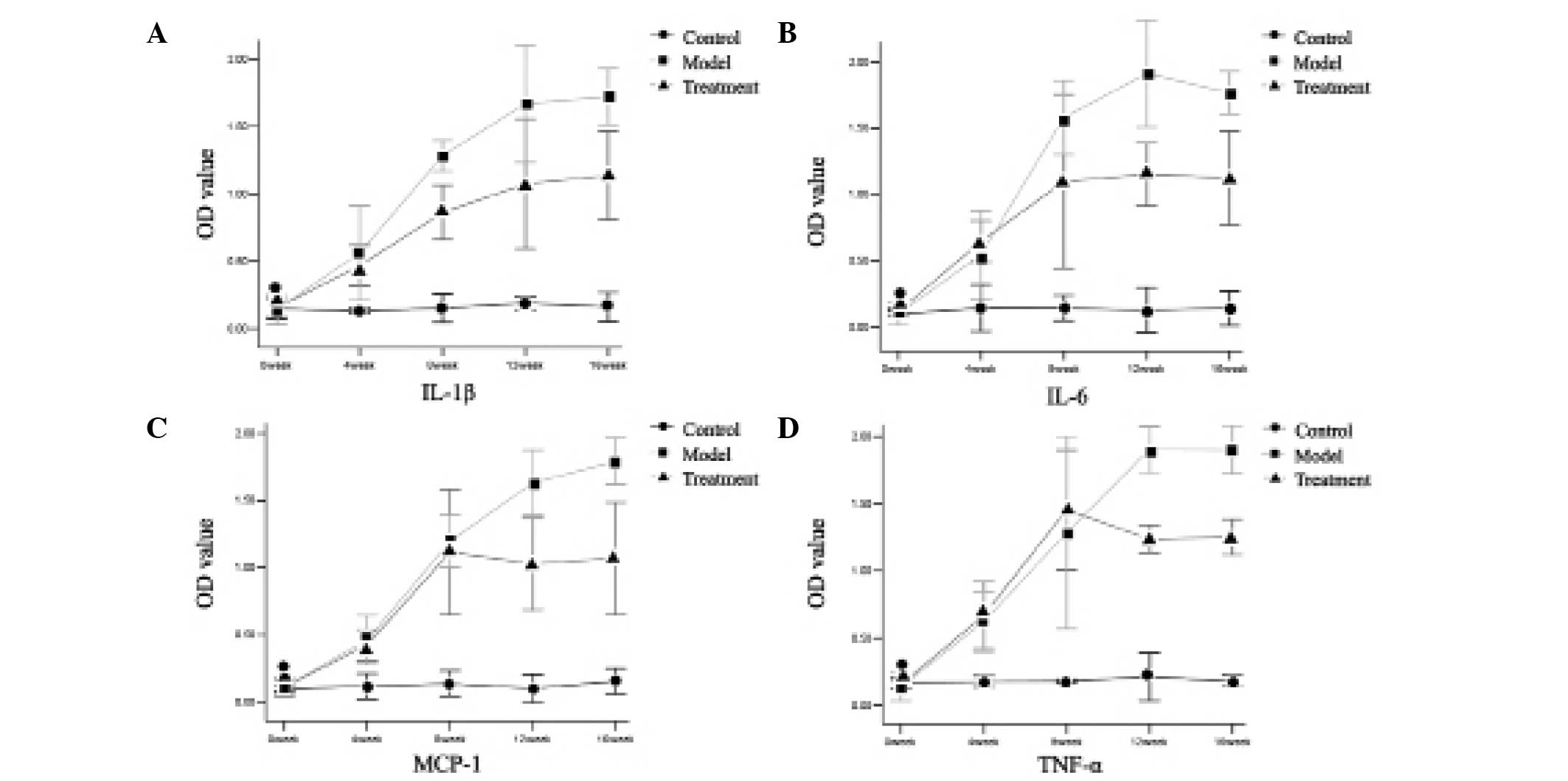
The differences in local cytokine levels in the
aortic tissue among the three groups were determined. As shown in
Fig. 2, atherosclerosis induced by
a high-fat diet was characterized by a gradual increase in the
levels of the inflammatory cytokines IL-1β, IL-6, MCP-1 and TNF-α
compared with the control group. However, the levels of these
cytokines were gradually downregulated following fistular onion
stalk extract treatment, compared with the effects observed in the
model group, and this difference was statistically significant at
the end of the 16th week.
Fistular onion stalk extract inhibits
local RAAS activity in aortic tissue
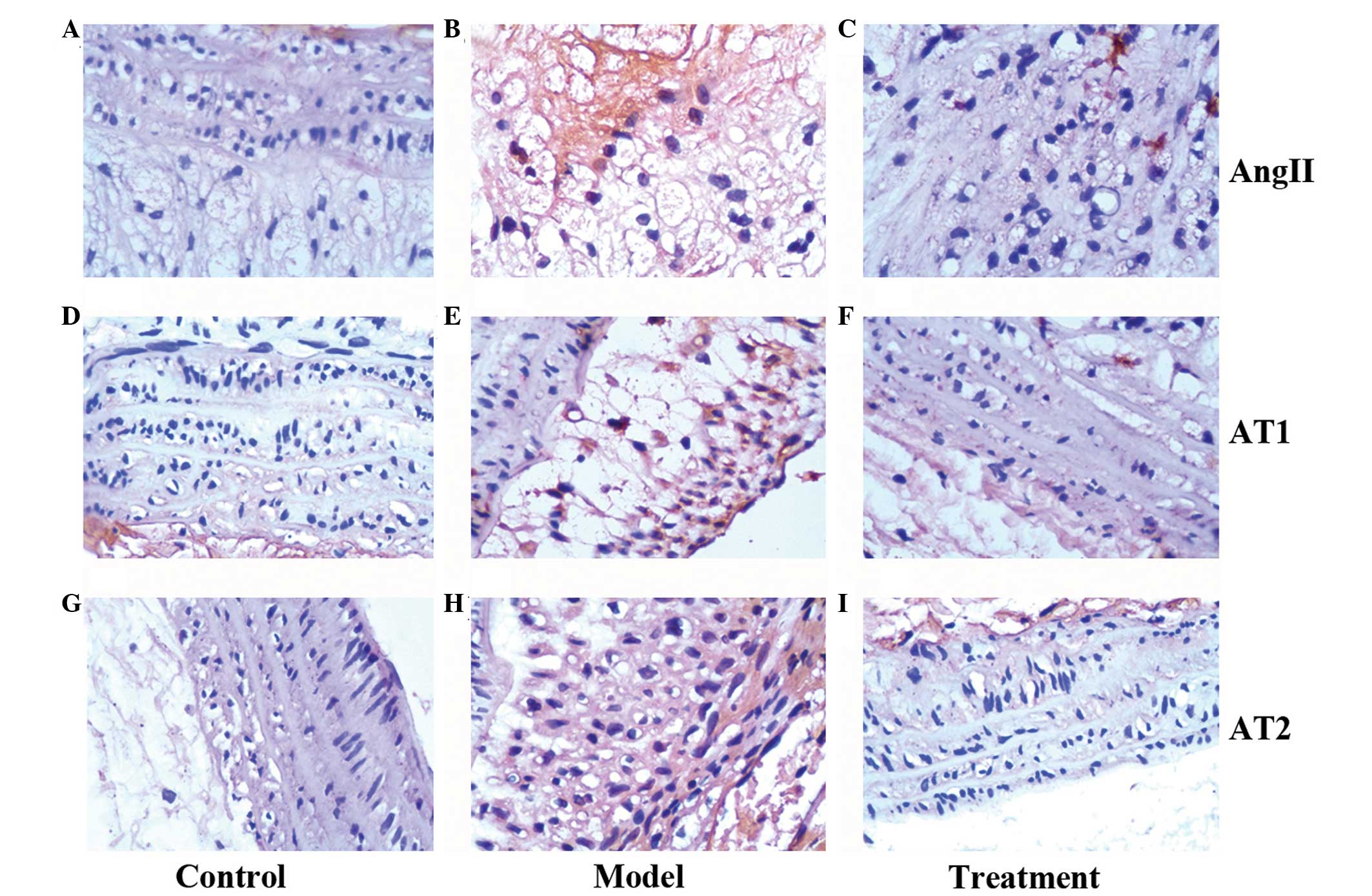
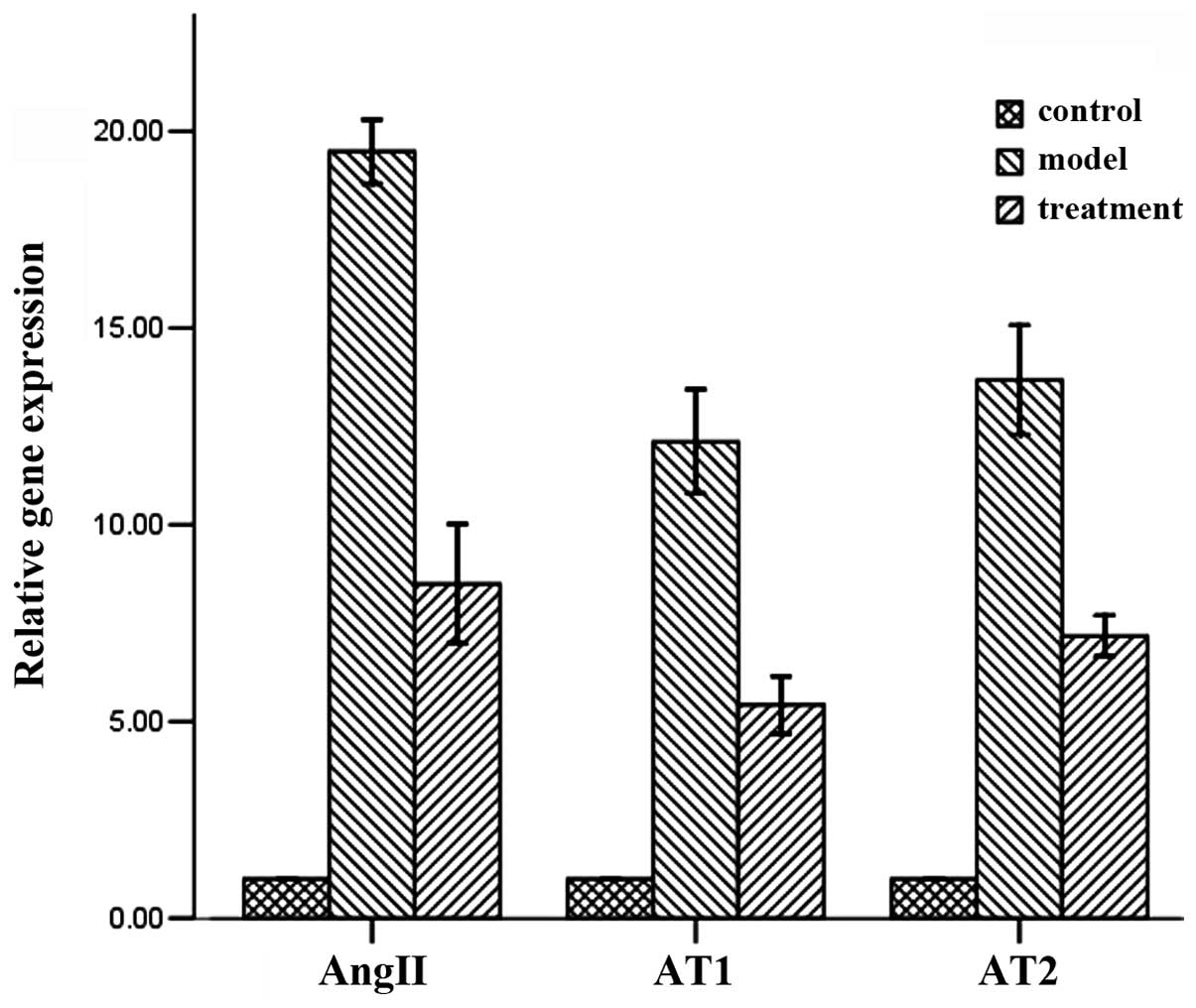
To evaluate the local RAAS activity, the expression
levels of AngII, AT1 and AT2 were determined by western blot
analysis. The data revealed that the levels of these proteins were
elevated at 16 weeks post-atherosclerosis induction; however,
fistular onion stalk extract treatment resulted in a significant
decrease in their expression (Fig.
3). These effects were further confirmed by a quantitative
polymerase chain reaction analysis of mRNA levels (Fig. 4).
Fistular onion stalk extract inhibits
local inflammatory signaling pathways in aortic tissue
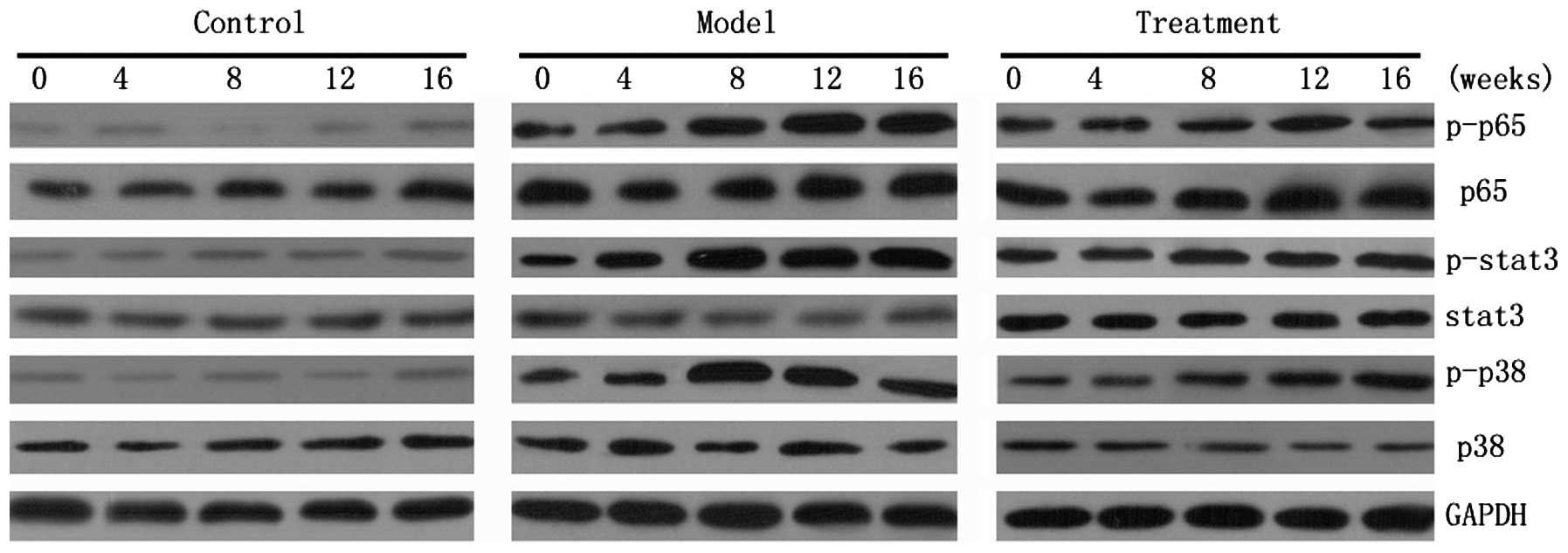
A number of signaling pathways are believed to
involve the transduction of signals from cytokines as well as the
regulation of inflammatory cytokines. Three pathways were examined
in the present study: The NF-κB, JAK/STAT and p38 MAPK pathways.
Western blot analysis revealed that the expression levels of p-p65,
p-stat3 and p-p38 were upregulated following the induction of
atherosclerosis, while the total levels of p65, stat3 and p38 did
not significantly differ. This indicates that these pathways are
all activated through phosphorylation. The activity of these
pathways was then detected in the treatment group. As expected,
administration of fistular onion stalk extract was able to inhibit
pathway activation (Fig. 5).
Discussion
A. fistulosum L. var. caespitosum
Makino possesses, according to the Traditional Chinese Medicine
theory, the capacity for engorgement-alleviating, detoxifying and
perspiration-promoting effects (31). Our previous study (32) showed that fistular onion stalk
extract exhibited a potential benefit in the treatment of
cardiovascular disease. In the present study, the most notable
finding was that treatment with fistular onion stalk extract
reduced the development of high-fat-induced experimental
atherosclerosis in rats. Treatment was shown to preserve the aortic
wall structure, inhibit local RAAS activity and prevent an
inflammatory response. These data provide experimental evidence
that treatment with fistular onion stalk extract can suppress
atherosclerosis.
Continuing systemic administration of a high-fat
diet appears to induce a cascade of events in the aortas, including
immune cell recruitment, increased local production of cytokines
and structural disruption of the aortic wall (30,33).
These events lead to the recognized histological features of human
atherosclerosis.
Chronic inflammation is one of the most important
features involved in the development and progression of
atherosclerosis. Early atherogenesis is characterized by the
expression of pro-inflammatory cytokines. Cytokines such as IL-1β,
IL-6, MCP-1 and TNF-α may be produced by cardiovascular cells,
including endothelial and vascular smooth muscle cells,
monocytes/macrophages and lymphocytes; these cytokines can, in
turn, activate various cardiovascular cells (34,35).
The positive feedback therefore results in a growing inflammatory
response and loss of homeostasis within the vessel wall. Consistent
with this, the in vivo model in the present study showed an
enhanced local expression of IL-1β, IL-6, MCP-1 and TNF-α in the
damaged vessel walls. It has been reported that the attenuation of
the inflammatory response in animal models inhibits atherosclerosis
(36). Therefore, the hypothesis
of the present study was that fistular onion stalk extract would
inhibit the expansion of atherosclerosis via a reduction in the
local inflammatory response. The results demonstrated that
lymphocyte infiltration was significantly reduced and local
cytokines were downregulated following fistular onion stalk extract
treatment.
The RAAS plays an important role in the regulation
of extracellular fluid volume and sodium balance. It is now
apparent that the RAAS also plays a pivotal role in the initiation
and deterioration of vascular inflammatory processes, which are
involved in in the formation of foam cells, the production of fatty
streaks and the eventual progression to the development of
rupture-vulnerable plaques (37–39).
In the in vivo model in the present study, the expression of
AngII, AT1 and AT2 was increased in the affected aorta. Antagonists
of the RAAS, including ACEIs and ARBs, also exert anti-inflammatory
effects (40,41); therefore, the present study
investigated whether fistular onion stalk extract would influence
local RAAS activity. It was revealed that the activity of AngII,
AT1 and AT2 was downregulated in the treatment group compared with
that in the model group.
The present study further determined the effect of
fistular onion stalk extract on inflammatory signaling pathways.
The NF-κB signaling pathway regulates inflammatory responses and
has been implicated in atherosclerosis (42). Endothelium-restricted inhibition of
NF-κB activation results in markedly reduced atherosclerotic plaque
formation (43). Consistent with
the above studies, the present study revealed that the p-p65 levels
were elevated in the model group, but decreased following treatment
with fistular onion stalk extract.
The majority of ILs, colony-stimulating factors and
interferons mediate their effects through the JAK/STAT pathway. A
previous study showed that the JAK/STAT pathway is an important
signaling pathway regulating the initiation/progression of
atherosclerosis (21), and
JAK/STAT activation has been found in atherosclerotic lesions
(44). In addition, when vascular
cells were incubated with cytokines or AngII, the JAK/STAT pathway
was activated (45,46). The present study also demonstrated
that the levels of p-stat3 became elevated following
atherosclerosis induction, while downregulated following fistular
onion stalk extract administration.
MAPK cascades have also been reported to contribute
to foam cell formation. When mouse peritoneal macrophages were
treated with oxidized low-density lipoprotein (oxLDL),
extracellular signal-regulated kinase 1/2, p38α MAPK and c-Jun
N-terminal kinase (JNK) 1/2 were all activated within 15 min, and
the treatment of macrophages with Src, JNK or p38 MAPK inhibitors
blocked oxLDL-induced foam cell formation (47). The present study also found that
the levels of p-p38 were increased in the atherosclerosis model
group, and treatment with fistular onion stalk extract suppressed
its expression.
Flavonoids are polyphenolic substances derived from
plants. Considerable in vitro and in vivo animal
research has focused on the anti-inflammatory potential of
flavonoids, including protection against arthritis (48), acute spinal cord injury (49) and metabolic syndrome (50), as well as the anti-atherosclerotic
effects of flavonoids (51). In a
previous study (31), four
flavonoids were successfully isolated from fistular onion stalk
extract, which may explain the potent anti-inflammatory effect of
fistular onion stalk extract observed in the present study. In
addition, the total expression of p65, stat3 and p38 in all three
groups in the present study was similar, which suggested that
fistular onion stalk extract exerted its anti-inflammatory effect
via the inhibition of phosphorylation.
In conclusion, the present study demonstrated that
fistular onion stalk extract significantly prevents the progression
of experimental atherosclerosis. This compound attenuates
lymphocyte infiltration and preserves vascular structure.
Furthermore, fistular onion stalk extract reduces the expression of
local inflammatory cytokines and RAAS proteins and inhibits the
intracellular phosphorylation of a number of key proteins in
inflammatory signal transduction. Fistular onion stalk extract is
thus useful as a potential therapy for atherosclerosis.
Acknowledgements
This study was supported by a grant from the Natural
Science project of Hubei Province of China (no. 2010CDZO23). The
authors would like to thank Tao Wang (Zishan BioTec Lab, Wuhan,
China) for technical support and Ling Yu (Wuhan University, Wuhan,
China) for his critical reading.
References
|
1
|
Kraaijeveld AO, de Jager SC, van Berkel
TJ, Biessen EA and Jukema JW: Chemokines and atherosclerotic plaque
progression: towards therapeutic targeting? Curr Pharm Des.
13:1039–1052. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Roger VL, Go AS, Lloyd-Jones DM, et al;
American Heart Association Statistics Committee and Stroke
Statistics Subcommittee. Heart disease and stroke statistics - 2012
update: a report from the American Heart Association. Circulation.
125:e2–e220. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Weber C, Zernecke A and Libby P: The
multifaceted contributions of leukocyte subsets to atherosclerosis:
lessons from mouse models. Nat Rev Immunol. 8:802–815. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Koh KK: Combination treatment to prevent
atherosclerosis. Hypertension. 54:e10–e11. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Tian J, Gu X, Sun Y, et al: Effect of
statin therapy on the progression of coronary atherosclerosis. BMC
Cardiovasc Disord. 12:702012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hoffmann H, Frieler K, Schlattmann P, Hamm
B and Dewey M: Influence of statin treatment on coronary
atherosclerosis visualised using multidetector computed tomography.
Eur Radiol. 20:2824–2833. 2010. View Article : Google Scholar
|
|
7
|
Ross R and Harker L: Hyperlipidemia and
atherosclerosis. Science. 193:1094–1100. 1976. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Inadera H and Hamazaki T: Cholesterol
controversy: cutoff point of low-density lipoprotein cholesterol
level in Guidelines by Japan Atherosclerosis Society. Nihon
Eiseigaku Zasshi. 65:506–515. 2010.(In Japanese).
|
|
9
|
Ravnskov U: High cholesterol level may
protect against infections and probably also atherosclerosis.
Lakartidningen. 101:1215–1217; discussion 1218, 1221–1222. 2004.(In
Swedish).
|
|
10
|
Nishizawa Y, Shoji T, Ishimura E, Inaba M
and Morii H: Paradox of risk factors for cardiovascular mortality
in uremia: is a higher cholesterol level better for atherosclerosis
in uremia? Am J Kidney Dis. 38(4 Suppl 1): S4–S7. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Liuzzo G: Atherosclerosis: an inflammatory
disease. Rays. 26:221–230. 2001.
|
|
12
|
Navab M, Gharavi N and Watson AD:
Inflammation and metabolic disorders. Curr Opin Clin Nutr Metab
Care. 11:459–464. 2008. View Article : Google Scholar
|
|
13
|
Campbell KA, Lipinski MJ, Doran AC,
Skaflen MD, Fuster V and McNamara CA: Lymphocytes and the
adventitial immune response in atherosclerosis. Circ Res.
110:889–900. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Gerrity RG, Naito HK, Richardson M and
Schwartz CJ: Dietary induced atherogenesis in swine. Morphology of
the intima in prelesion stages. Am J Pathol. 95:775–792.
1979.PubMed/NCBI
|
|
15
|
Gerszten RE, Mach F, Sauty A, Rosenzweig A
and Luster AD: Chemokines, leukocytes, and atherosclerosis. J Lab
Clin Med. 136:87–92. 2000. View Article : Google Scholar
|
|
16
|
Frieri M: Accelerated atherosclerosis in
systemic lupus erythematosus: role of proinflammatory cytokines and
therapeutic approaches. Curr Allergy Asthma Rep. 12:25–32. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Takahashi M: Inflammatory cytokines in the
pathogenesis of atherosclerosis. Nihon Rinsho. 69:30–33. 2011.(In
Japanese).
|
|
18
|
Ait-Oufella H, Taleb S, Mallat Z and
Tedgui A: Recent advances on the role of cytokines in
atherosclerosis. Arterioscler Thromb Vasc Biol. 31:969–979. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Morris JB, Olzinski AR, Bernard RE, et al:
p38 MAPK inhibition reduces aortic ultrasmall superparamagnetic
iron oxide uptake in a mouse model of atherosclerosis: MRI
assessment. Arterioscler Thromb Vasc Biol. 28:265–271. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Dąbek J, Kułach A and Gąsior Z: Nuclear
factor kappa-light-chain-enhancer of activated B cells (NF-κB): a
new potential therapeutic target in atherosclerosis? Pharmacol Rep.
62:778–783. 2010.
|
|
21
|
Ortiz-Muñoz G, Martin-Ventura JL,
Hernandez-Vargas P, et al: Suppressors of cytokine signaling
modulate JAK/STAT-mediated cell responses during atherosclerosis.
Arterioscler Thromb Vasc Biol. 29:525–531. 2009.PubMed/NCBI
|
|
22
|
Kirii H, Niwa T, Yamada Y, et al: Lack of
interleukin-1beta decreases the severity of atherosclerosis in
ApoE-deficient mice. Arterioscler Thromb Vasc Biol. 23:656–660.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Egorova MO: Increased serum level of the
acute inflammation phase parameter CRP and the high level of low
density lipoprotein cholesterol - factors of increased risk of
development of atherosclerosis and its complications (a literature
review). Klin Lab Diagn. 3–6. 2002.(In Russian).
|
|
24
|
Olson NC, Callas PW, Hanley AJ, et al:
Circulating levels of TNF-α are associated with impaired glucose
tolerance, increased insulin resistance, and ethnicity: the Insulin
Resistance Atherosclerosis Study. J Clin Endocrinol Metab.
97:1032–1040. 2012.
|
|
25
|
Haddy N, Sass C, Droesch S, et al: IL-6,
TNF-alpha and atherosclerosis risk indicators in a healthy family
population: the STANISLAS cohort. Atherosclerosis. 170:277–283.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Zaritsky JJ and Kalantar-Zadeh K: The
crossroad of RAAS modulation, inflammation, and oxidative stress in
dialysis patients: light at the end of the tunnel? J Am Soc
Nephrol. 23:189–191. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Ferrario C: Effect of angiotensin receptor
blockade on endothelial function: focus on olmesartan medoxomil.
Vasc Health Risk Manag. 5:301–314. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Hershon KS: Mechanistic and clinical
aspects of renin-angiotensin-aldosterone system blockade in the
prevention of diabetes mellitus and cardiovascular disease. Endocr
Pract. 17:430–440. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Cheng M, Wen R and Zhang CG: Supercritical
fluid extraction of fistular onion stalk by carbon dioxide. Herald
of Medicine. 27:213–215. 2008.(In Chinese).
|
|
30
|
Zhou BR, Pan Y and Zhai ZM: Fibrinogen and
P-selectin expression in atherosclerosis model of Sprague Dawley
rat. Chin Med J (Engl). 124:3768–3772. 2011.PubMed/NCBI
|
|
31
|
Fu Q, Liu J, Zhang C, et al: Separation
and identification of flavonoids from fistular onion stalk
(Allium fisturosum L. var. caespitosum Makino). J
Huazhong Univ Sci Technolog Med Sci. 30:255–257. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Zhang JM, Hao JJ, Guo J, He BH and Huang
H: Effects of fistular onion stalk extract on the level of NO and
expression of endothelial NO synthase (eNOS) in human umbilical
vein endothelium cells. Afr J Biotechnol. 10:2536–2540. 2011.
|
|
33
|
Fotis L, Agrogiannis G, Vlachos IS, et al:
Intercellular adhesion molecule (ICAM)-1 and vascular cell adhesion
molecule (VCAM)-1 at the early stages of atherosclerosis in a rat
model. In Vivo. 26:243–250. 2012.PubMed/NCBI
|
|
34
|
Fan J and Watanabe T: Inflammatory
reactions in the pathogenesis of atherosclerosis. J Atheroscler
Thromb. 10:63–71. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Libby P: Inflammation in atherosclerosis.
Nature. 420:868–874. 2002. View Article : Google Scholar
|
|
36
|
Paoletti R, Gotto AM Jr and Hajjar DP:
Inflammation in atherosclerosis and implications for therapy.
Circulation. 109(23 Suppl 1): III20–III26. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Fukui K, Yamada H and Matsubara H:
Pathophysiological role of tissue renin-angiotensin-aldosterone
system (RAAS) in human atherosclerosis. Nihon Rinsho. 70:1556–1561.
2012.(In Japanese).
|
|
38
|
Hirata Y, Fukuda D and Sata M: Critical
role of renin-angiotensin system in the pathogenesis of
atherosclerosis. Nihon Rinsho. 69:55–59. 2011.(In Japanese).
|
|
39
|
Partigulova AS and Naumov VG: Inflammation
and atherosclerosis: the role of Renin-Angiotensin system and its
inhibition. Kardiologiia. 50:50–55. 2010.(In Russian).
|
|
40
|
Fukuda D, Enomoto S, Nagai R and Sata M:
Inhibition of renin-angiotensin system attenuates periadventitial
inflammation and reduces atherosclerotic lesion formation. Biomed
Pharmacother. 63:754–761. 2009. View Article : Google Scholar
|
|
41
|
Lu H, Balakrishnan A, Howatt DA, et al:
Comparative effects of different modes of renin angiotensin system
inhibition on hypercholesterolaemia-induced atherosclerosis. Br J
Pharmacol. 165:2000–2008. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Monaco C, Andreakos E, Kiriakidis S, et
al: Canonical pathway of nuclear factor kappa B activation
selectively regulates proinflammatory and prothrombotic responses
in human atherosclerosis. Proc Natl Acad Sci USA. 101:5634–5639.
2004. View Article : Google Scholar
|
|
43
|
Gareus R, Kotsaki E, Xanthoulea S, et al:
Endothelial cell-specific NF-kappaB inhibition protects mice from
atherosclerosis. Cell Metab. 8:372–383. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Gharavi NM, Alva JA, Mouillesseaux KP, et
al: Role of the Jak/STAT pathway in the regulation of interleukin-8
transcription by oxidized phospholipids in vitro and in
atherosclerosis in vivo. J Biol Chem. 282:31460–31468. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
45
|
O’Sullivan LA, Liongue C, Lewis RS,
Stephenson SE and Ward AC: Cytokine receptor signaling through the
Jak-Stat-Socs pathway in disease. Mol Immunol. 44:2497–2506.
2007.PubMed/NCBI
|
|
46
|
Recinos A III, LeJeune WS, Sun H, et al:
Angiotensin II induces IL-6 expression and the Jak-STAT3 pathway in
aortic adventitia of LDL receptor-deficient mice. Atherosclerosis.
194:125–133. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Muslin AJ: MAPK signalling in
cardiovascular health and disease: molecular mechanisms and
therapeutic targets. Clin Sci (Lond). 115:203–218. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Mamani-Matsuda M, Kauss T, Al-Kharrat A,
et al: Therapeutic and preventive properties of quercetin in
experimental arthritis correlate with decreased macrophage
inflammatory mediators. Biochem Pharmacol. 72:1304–1310. 2006.
View Article : Google Scholar
|
|
49
|
Schültke E, Kendall E, Kamencic H, Ghong
Z, Griebel RW and Juurlink BH: Quercetin promotes functional
recovery following acute spinal cord injury. J Neurotrauma.
20:583–591. 2003.PubMed/NCBI
|
|
50
|
Rivera L, Morón R, Sánchez M, Zarzuelo A
and Galisteo M: Quercetin ameliorates metabolic syndrome and
improves the inflammatory status in obese Zucker rats. Obesity
(Silver Spring). 16:2081–2087. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Kleemann R, Verschuren L, Morrison M, et
al: Anti-inflammatory, anti-proliferative and anti-atherosclerotic
effects of quercetin in human in vitro and in vivo models.
Atherosclerosis. 218:44–52. 2011. View Article : Google Scholar : PubMed/NCBI
|