1. Introduction
Osteonecrosis of the femoral head (ONFH) results in
the collapse of the femoral head and the rapid destruction of the
hip joint. ONFH has a significant impact on adults aged between 35
and 55 years. This pathological state has several possible
etiologies that cause a reduction in the vascular supply to the
subchondral bone of the femoral head, resulting in microcirculation
disturbance and the subsequent collapse of the femoral head
(1–3). In general, the type of treatment
carried out varies according to the disease etiology. Treatments
include non-weight-bearing (NWB) therapy, physical support and the
alteration of cytoactivity. Extracorporeal shock wave therapy
(ESWT) is used to reduce osteoblast and osteocyte apoptosis. Other
therapies used include hyperbaric oxygen (HBO) therapy and core
decompression. Certain reports (4–6)
suggest that bisphosphonates increase osteoclast apoptosis and
prevent the collapse of the femoral head. Various femoral
head-preserving procedures have been carried out in an attempt to
prevent the requirement for a complete hip replacement. The present
review focuses on treatments for ONFH (7,8).
2. NWB therapy
The initial treatment for early stage ONFH is NWB
therapy (9), including a complete
rest from weight bearing or changing the weight-bearing status.
This type of therapy is able to prevent damage to vessels that
supply the femoral head, which is advantageous for ONFH with
articular collapse (10). However,
a previous review identified that limiting the patient to a
wheelchair or walking frame to reduce weight bearing does not
achieve satisfactory clinical benefits (11). It was observed that in
nonoperatively managed patients with ONFH, only 20% achieved
recovery and 80% required surgery, including total hip replacement
or other treatments (11).
Transtrochanteric rotational osteotomy was developed
in 1972 (12,13) to prevent the progressive collapse
of the articular surface and osteoarthritic changes in patients
with ONFH. The process is technically demanding and preserves the
shape of the femoral head by altering its weight-bearing status
(14). However, a number of
studies (15–18) have indicated variable rates of
success for the surgery. A study by Hiranuma et al (16) evaluated hip instability following
transtrochanteric rotational osteotomy. Instability was defined as
>1 mm translation of the femoral head appearing on transverse
computed tomography scans obtained at 0 and 45° flexion of the hip
joint; 11 of the 27 hips studied (~40%) revealed instability
following surgery.
Although NWB therapy is widely used to treat the
early stages of ONFH, certain studies (19–21)
have concluded that it is not able to cure the disease or prevent
femoral head collapse if it is the only treatment. NWB therapy did
not prevent ONFH in rats in a study by Okazaki et al
(21), which also clarified the
role of weight bearing in the development of ONFH. In the study, an
ONFH model was established in non-weight-bearing and weight-bearing
groups of rats following lipopolysaccharide and methylprednisolone
stimulation. Three weeks after the final methylprednisolone
injection, the two groups did not differ in the progression of
ONFH. Thus, the authors concluded that weight bearing may not
contribute to the development of non-traumatic ONFH in rats.
Transtrochanteric rotational osteotomy is an ideal
treatment for joint preservation. However, it has not gained
widespread acceptance as a treatment for ONFH due to the
inconsistency of the obtained results.
3. Physical support
Bone grafting
The ideal surgical procedure for ONFH would be to
remove the necrotic bone from the femoral head and replace it with
viable and structurally sound bone, thereby restoring vitality to
the femoral head and preventing the collapse of the articular
surface. Bone grafting is an appealing treatment option as it
combines the benefit of decompressing the femoral head with the
introduction of osteoconductive and/or osteoinductive material into
the devitalized head. Furthermore, such grafting preserves the
natural hip geometry and articular cartilage, unlike the osteotomy
and arthroplasty methods.
Nonvascularized and vascularized bone
grafting
Nonvascularized bone grafting is an attractive
alternative treatment used when there is precollapse or minimal
postcollapse of ONFH with relatively preserved articular cartilage
(22–27). Rosenwasser et al (28) reported that thorough debridement
and cancellous bone-grafting in patients with ONFH was an
efficacious treatment, with 87% of the patients studied remaining
essentially free of symptoms and with minimal progression of
osteoarthritis following the procedure.
Vascularized bone is grafted onto the necrotic
femoral head to directly target its devascularized status. Such a
procedure, in addition to replacing necrotic bone with healthy
bone, establishes a new source of circulating blood, thus
introducing osteoinductive cells and promoting the restoration of a
healthy subchondral plate (29–31).
Tetik et al (23) carried
out a clinical study comparing the results of vascularized and
nonvascularized fibular grafting and revealed more improved
clinical and radiographic results with vascularized compared with
nonvascularized grafting.
Free vascularized fibular grafting has been
successfully used as a joint-preserving procedure treatment for
ONFH, and a number of studies have demonstrated satisfactory mid-
and long-term outcomes (32–36).
The procedure may be effective for avoiding or preventing the
requirement for complete hip arthroplasty in young patients with
early to intermediate stages of ONFH. Kawate et al (37) identified that minor osteonecrosis
(<300° of the femoral head) without preoperative collapse
(Steinberg classification stages I and II) was the primary
indicator for free vascularized fibular grafting treatment.
Osteonecrosis induced by steroid use was a relative counter
indicator. Major osteonecrosis (>300° of the femoral head), with
a severe preoperative collapse (>3 mm), was a major counter
indicator. Studies concerning grafting as a treatment for ONFH in
patients with lymphoma are rare. The surgical benefits and safety
remain to be systematically assessed. Yin et al (38) retrospectively reviewed seven
patients (14 hips) with lymphoma (two cases of Hodgkin’s disease
and five cases of non-Hodgkin’s lymphoma) who underwent free
vascularized fibular grafting for ONFH. All patients exhibited a
positive recovery without any severe life-threatening
complications. The mean Harris hip score improved from 69 to 88,
while the mean pain score on a visual analog scale decreased from
54 to 18. Radiography revealed either improved or unchanged results
in the three hips with initial Steinberg classification stage II
osteonecrosis and in nine of the 11 hips with stage III or IV
osteonecrosis. None of the hips demonstrated a failure of the
treatment or required complete hip arthroplasty. Despite the
technically demanding nature of the procedure, the use of free
vascularized fibular grafting improves the quality of life of
patients with ONFH, with functional improvement and the alleviation
of pain. The procedure involves decompressing the femoral head,
excising the necrotic bone and adding a cancellous bone graft with
osteoinductive and osteoconductive properties, which augments
revascularization and neo-osteogenesis of the femoral head
(37,39).
Tantalum implants
Preservation of an osteonecrotic femoral head relies
on preventing the collapse of the structurally compromised necrotic
bone. Tantalum rod implantation has been proposed as a treatment in
the early stages of ONFH. It has demonstrated bone ingrowth and
rapid fixation in functional and non-functional animal models and
in human explant case reports (40–43).
The procedure preserves the structural integrity of the femoral
head and is most effective in hips at the pre-collapse stage.
The use of tantalum rods for ONFH was first proposed
in 1997 by Schnieders et al (44). The authors used a magnetic
resonance-based three-dimensional finite element model of ONFH to
study the mechanical effects of inserting a porous tantalum rod
into a necrotic femoral head. The porous tantalum rod was a
reasonable mechanical substitute for a fibular graft, since it
effectively reduced the peak ratio of stress to strain. Liu et
al (45) demonstrated that a
porous tantalum implant effectively supports the subchondral bone
of the femoral head and that the strength of the implant is
>9-fold than that of the loading stress exerted on the implant.
Varitimidis et al (43)
studied 27 patients who underwent tantalum rod implantation for
nontraumatic ONFH. The implant was a porous tantalum rod (10 mm).
One patient (one hip) succumbed 15 months following surgery for
unrelated reasons. In total, 13 of the 26 hips remained at the same
radiographic stage, while 13 revealed deterioration. The authors
concluded that porous tantalum rods were simple to use via a
minimally invasive and reproducible method, and may provide
functional recovery for patients at pre- and post-collapse stages
of hip osteonecrosis.
These results confirm the curative effects of a
porous tantalum rod prosthesis on ONFH, particularly at Steinberg
classification stages I and II and at stage IIIA with minimal
collapse. The procedure resolves pain as well as preventing and
curing the collapse of the femoral head due to necrosis.
4. Increased osteoclast apoptosis and
reduced osteoblast and osteocyte apoptosis
A number of studies have proposed a balanced system
of manipulating osteoclasts and osteoblasts in order to prevent
collapse of the femoral head in patients with ONFH (46,47).
Changes in the prevalence of osteoblast apoptosis may have a
significant impact on the number of osteoblasts present at bone
formation sites and on their function during therapies including
ESWT, HBO treatment and core decompression. Furthermore, an
increase in osteoclast apoptosis and inhibited action of mature
osteoclasts on bone reduces bone diminution and reinforces bone
remodeling (48).
Osteoblast promotion
ESWT
ESWT began with the incidental observation of the
osteoblastic response pattern during animal studies in the
mid-1980s, which generated interest in the potential use of ESWT
for musculoskeletal disorders (49). Shockwaves are high-energy acoustic
waves generated by electrohydraulic or electromagnetic principles.
ESWT is effective for treating non-union long bone fractures and
tendinopathy of the shoulder, elbow, knee and heel (50) It has been trialed as a treatment
for early ONFH and a number of studies (51) have reported the positive effects of
the therapy for ONFH (52,53).
Wang et al (52) demonstrated that ESWT is a more
effective treatment than core decompression and nonvascularized
fibular grafting for patients with early ONFH. In ESWT treatment,
the affected hip is positioned in adduction and with internal
rotation by securing the limb to a table. For lesions at stages II
or III, the junctional zone between the avascular and vascular bone
of the femoral head is delineated under C-arm control. Four focal
points are selected, ~1.0 cm apart, and marked with a marker. Each
of the four points is treated with 1,500 shock wave impulses at 28
kV (equivalent to 0.6 mJ/mm2 energy flux density), for a
total of 6,000 impulses. Following treatment, patients are
instructed to walk on crutches with partial weight bearing on the
affected limb for 4–6 weeks. Yin et al (50) reported that ESWT significantly
enhanced the angiogenic and osteogenic effects of bone-marrow stem
cells via the nitric oxide pathway in patients with ONFH. Thus,
ESWT is a novel non-invasive alternative to surgery (which
therefore avoids the risks associated with surgery) and is
increasingly clinically applied.
HBO therapy
HBO has numerous treatment implications as it has a
number of physiological and pharmacological modes of action.
Various studies have presented histological evidence that the
earliest stage of ONFH is preceded by bone-marrow edema, as
observed on magnetic resonance imaging (MRI) scans (54,55).
Venous drainage is restored by reducing intraosseous pressure,
thereby improving the microcirculation. HBO restores tissue
oxygenation, reduces edema and induces angioneogenesis (56). Camporesi et al (57) demonstrated that HBO therapy may be
a viable treatment modality for Ficat stage II ONFH. In the study,
symptoms were relieved following a multi-year follow-up, without
hip arthroplasty being required. In a study by Reis et al
(58), 12 patients with Steinberg
classification stage 1 ONFH received daily HBO therapy for 100
days. Overall, 81% of the treated patients demonstrated a normal
performance on MRI scans compared with 17% in the untreated group.
The authors thus presented evidence for the benefit of HBO
treatment for idiopathic stage I ONFH. HBO therapy may be useful
when carried out in conjunction with core decompression,
fenestration and drilling, or other forms of orthopedic
intervention. It may also be considered as a primary treatment for
ONFH and not merely an adjuvant therapy.
Core decompression
The most popular treatment implemented for ONFH is
core decompression, which is the standard surgical procedure
carried out to treat early-stage non-traumatic ONFH. Various
techniques have been trialed in an attempt to discover a treatment
to protect the osteonecrotic femoral head. A number of studies have
advocated small-diameter percutaneous drilling (59–61).
Mont et al (62) reported a
new technique for core decompression involving multiple small
drilled holes and a 3-mm Steinman pin. In the study, 32 of the 45
hips (71%; 35 patients) demonstrated successful clinical results
following a mean follow-up of two years (range, 20–39 months). In
total, 24 of the 30 stage I hips (80%; 23 patients) had successful
outcomes compared with eight of the 15 stage II hips (57%; 12
patients), with no surgical complications. This technique may be
effective for delaying the need for total hip arthroplasty in young
patients with early (precollapse) stages of ONFH. Certain other
studies (62–65) have supplemented core decompression
with electrical stimulation.
In a study by Steinberg (66), 116 hips with ONFH underwent
decompression and grafting; 74 also received direct current
stimulation via a coil inserted into the femoral head.
Decompression and grafting were safe and reasonably effective for
retarding the progression of ONFH. The supplementary electrical
stimulation was observed to further improve the results.
Core decompression remains the leading surgical
treatment for ONFH (early- and mid-stage), and the efficacy of any
new treatments should be compared with core decompression. Marker
et al (67) collected data
from 1,268 hips following decompression and revealed a clinical
success rate of 70% after 63 months, without the need for
additional surgery. Certain studies reported core decompression
combined with other treatments produces an improved effect for ONFH
(68–70). Implanting a demineralized bone
matrix or porous hydroxyapatite composite filler achieves more
improved results than using core decompression with other
augmentation strategies, including bone marrow and growth factors
(71–73).
Adrenocorticotropic hormone (ACTH) and
vascular endothelial growth factor (VEGF)
The development of ONFH is accompanied by the
apoptosis of osteocytes and osteoclasts (74). Zaidi et al (75) reported that ACTH plays a role in
preventing osteonecrosis by promoting osteoblastic support and the
expression of VEGF. Early ONFH reveals medium or strong staining of
fibroblast growth factor 2 and VEGF, which may promote osteogenesis
and bone reconstruction (76).
VEGF is a key factor in bone remodeling. Ingrowth of
reparative arterioles has been observed in late-stage osteonecrosis
(77). VEGF is a prominent
angiogenesis control factor and is used as a therapeutic tool to
enhance neovascularization. Angiogenesis is an important part of
the bone repair process, and the close connection between blood
vessels (endothelial cells) and bone (osteoblasts) was recognized
by Trueta and Buhr (78) in 1963.
Cao et al (79) implanted
deproteinized bone (DPB) with VEGF (absorbed in the form of the
recombinant plasmid pcDNA3.1-hVEGF165) into necrotic femoral heads
to induce angiogenesis and promote repair. The study revealed that
transfection with hVEGF165 enhanced local angiogenesis and the
DPB-VEGF compound improved repair. Hang et al (80) evaluated the efficacy of VEGF165
transgenic bone marrow mesenchymal stem cells on the repair of
early-stage ONFH in mature mongrel dogs and demonstrated that the
treatment enhanced bone reconstruction and blood vessel
regeneration.
Osteoclast inhibition
Pharmacotherapy
Bisphosphonates, such as alendronate, promote
osteoclast apoptosis through several mechanisms, including
inhibiting protein prenylation and blocking mevalonate metabolism
(81). Bisphosphonate reduces
edema and the rate of remodeling, which contracts the remodeling
spaces and prevents the progression of bone collapse (82). Bone formed during alendronate
treatment is histologically normal (83–86)
and the treatment appears to offer the greatest protection against
fracture. Bisphosphonates are antiresorptive agents that act by
inhibiting the action of mature osteoclasts on bone. They
transiently stimulate the proliferation and increase the
differentiation of pro-osteoblasts, increase the production of the
antiresorptive protein osteoprotegerin by osteoblasts, and decrease
edema at the site of ONFH, possibly through their anti-inflammatory
action.
Agarwala et al (87) treated 69 patients with ONFH with
alendronate. The disease duration was 0–36 months. The treatment
decreased pain and disability within a few weeks and reduced
progressive bone collapse, thus positively altering the progress of
ONFH. Alendronate is an antiresorptive agent which reduces edema,
the risk of fracture, and the rate of remodeling, thereby
contracting the remodeling spaces and preventing the progression of
bone collapse.
Although bisphosphonates, including alendronate and
zoledronate, have revolutionized treatment for ONFH and
osteoporosis, a number of studies (88–94)
have demonstrated a serious complication of osteonecrosis in the
jaw, which has been the subject of much media attention and
resulted in patients at risk of ONFH refusing treatment with
bisphosphonates. Outeiriño-Fernández (89) reviewed studies on osteonecrosis of
the jaw and concluded that alendronate was the bisphosphonate used
in the majority of cases, with a mean duration of treatment prior
to jaw osteonecrosis of 48.3 months.
In summary, bisphosphonates have revolutionized the
treatment of ONFH; however, they carry an increased risk of
bisphosphonate-related osteonecrosis of the jaw. Thus, monitoring
should be increased in order to prevent the disadvantages
associated with these drugs.
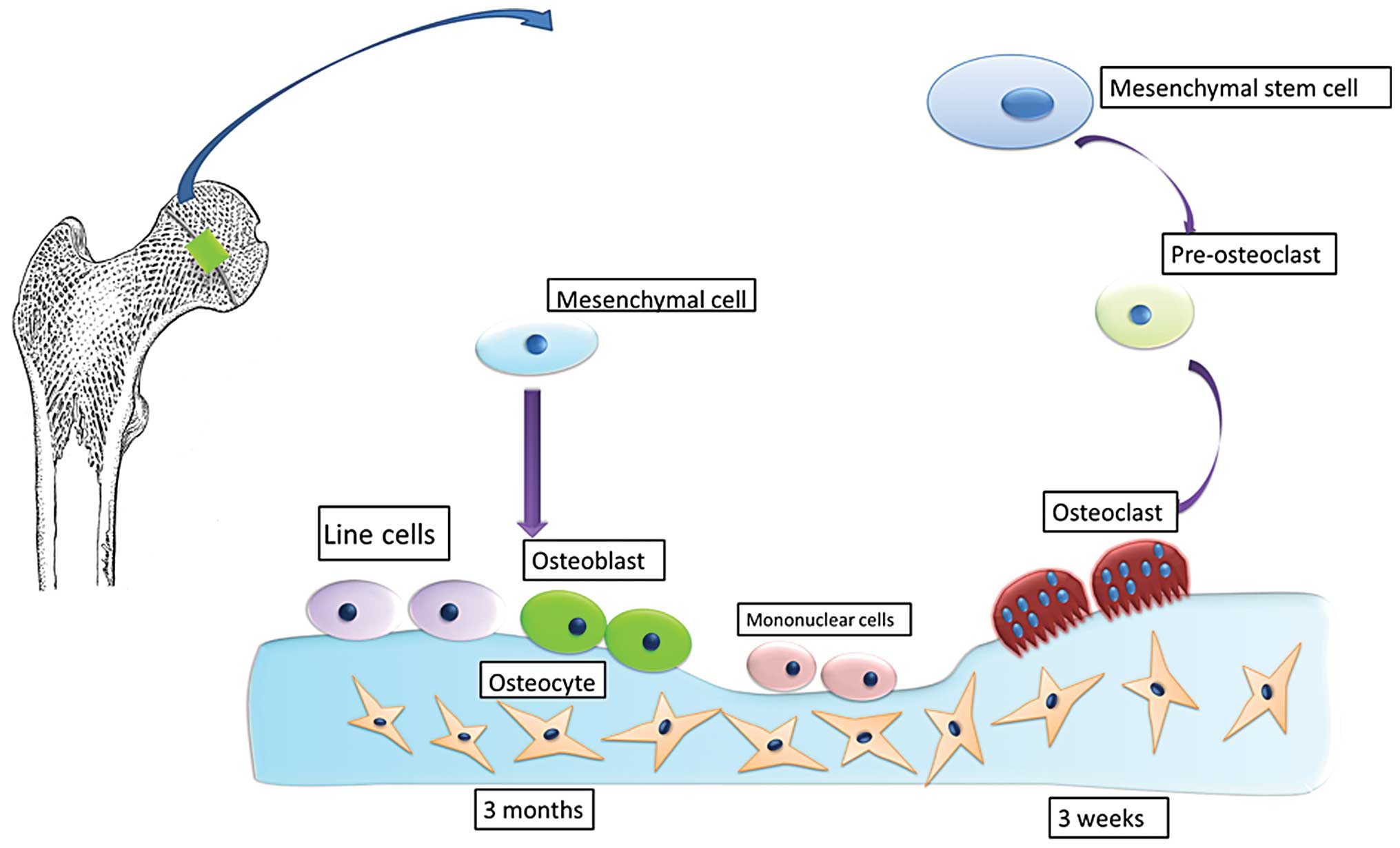
5. Conclusions
ONFH is frequently observed in relatively young
adults and its management remains controversial. Conservative
treatment may be a major focus for orthopedic studies in the
future. The principle of the treatment is to provide mechanical
support to prevent collapse of the femoral head and improve the
speed and quality of repair at the molecular level, increase
osteoclast apoptosis, and reduce osteoblast and osteocyte
apoptosis. A number of treatment modalities (operative and
nonoperative) have positively altered the natural progression of
ONFH during the early stage of the disease. Such treatments include
ESWT, HBO, pharmacotherapy and paracentesis therapy with VEGF or
stem cells. Surgical approaches include core decompression with
structural and cellular supplementation. Damage to the bone
structure, a reduction in macromechanical performance, and
subsequent collapse is considered to occur during the process of
restoration. The phenomenon of the destructive bone repair process
is inherent, with bone restoration occurring first followed by
repeated action of the bone leading to fatigue from the load and
subsequent fracture. Following the initiation of restoration,
neovascularization occurs and new bone formation is required to
initially break down the sequestrum. Under continued mechanical
loads, the femoral head collapses and there is no further bone
resorption or osteogenesis. During the repair process, the balanced
bone remodeling carried out by osteoblasts and osteoclasts begins.
The process of osteogenesis takes ~3 months to establish new bone
with an effective mechanical performance; however, it takes only ~3
weeks for osteoclasts to affect the trabecular bone structure. A
reduction of the macromechanical strength of the entire femoral
head is present in the repair process and also during the collapse
of the femoral head under mechanical load. Therefore, delaying or
altering the process of femoral head necrosis and collapse through
human intervention and recreating a balanced system of osteoblast
and osteoclast actions, whilst simultaneously providing sufficient
mechanical support, should be studied in the future (Fig. 1).
Preventing collapse of the femoral head is likely to
increase in focus in the coming decades since the majority of
patients are relatively young at diagnosis. ONFH is undoubtedly a
challenging condition to treat; however, ongoing scientific and
clinical investigations are progressing towards the development of
effective future treatment options.
References
|
1
|
Kim HJ: Autologous adipose tissue-derived
stem cells induce persistent bone-like tissue in osteonecrotic
femoral heads: not bone-like, but fat-like tissue. Pain Physician.
15:E749–E752. 2012.PubMed/NCBI
|
|
2
|
Hasan SS and Romeo AA: Nontraumatic
osteonecrosis of the humeral head. J Shoulder Elbow Surg.
11:281–298. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kaushik AP, Das A and Cui Q: Osteonecrosis
of the femoral head: An update in year 2012. World J Orthop.
3:49–57. 2012.PubMed/NCBI
|
|
4
|
Chen CH, Chang JK, Lai KA, Hou SM, Chang
CH and Wang GJ: Alendronate in the prevention of collapse of the
femoral head in nontraumatic osteonecrosis: a two-year multicenter,
prospective, randomized, double-blind, placebo-controlled study.
Arthritis Rheum. 64:1572–1578. 2012.PubMed/NCBI
|
|
5
|
Shabtai L, Drexler M and Blummberg N:
Biphosphonate in the treatment of avascular necrosis of the femoral
head. Harefuah. 151:242–245. 2522012.(In Hebrew).
|
|
6
|
Peled E, Bejar J, Barak M, Orion E and
Norman D: Core decompression and alendronate treatment of the
osteonecrotic rat femoral head: computer-assisted analysis. Int J
Exp Pathol. 94:212–216. 2013.PubMed/NCBI
|
|
7
|
Amanatullah DF, Strauss EJ and Di Cesare
PE: Current management options for osteonecrosis of the femoral
head: part II, operative management. Am J Orthop (Belle Mead NJ).
40:E216–E225. 2011.PubMed/NCBI
|
|
8
|
Amanatullah DF, Strauss EJ and Di Cesare
PE: Current management options for osteonecrosis of the femoral
head: part 1, diagnosis and nonoperative management. Am J Orthop
(Belle Mead NJ). 40:E186–E192. 2011.PubMed/NCBI
|
|
9
|
Mihara K and Hirano T: Standing is a
causative factor in osteonecrosis of the femoral head in growing
rats. J Pediatr Orthop. 18:665–669. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Peskin B, Shupak A, Levin D, et al:
Effects of non-weight bearing and hyperbaric oxygen therapy in
vascular deprivation-induced osteonecrosis of the rat femoral head.
Undersea Hyperb Med. 28:187–194. 2001.PubMed/NCBI
|
|
11
|
Mont MA, Carbone JJ and Fairbank AC: Core
decompression versus nonoperative management for osteonecrosis of
the hip. Clin Orthop Relat Res. 324:169–178. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sugioka Y: Transtrochanteric anterior
rotational osteotomy of the femoral head in the treatment of
osteonecrosis affecting the hip: a new osteotomy operation. Clin
Orthop Relat Res. 130:191–201. 1978.PubMed/NCBI
|
|
13
|
Sugioka Y, Katsuki I and Hotokebuchi T:
Transtrochanteric rotational osteotomy of the femoral head for the
treatment of osteonecrosis. Follow-up statistics. Clin Orthop Relat
Res. 169:115–126. 1982.PubMed/NCBI
|
|
14
|
Koo KH, Song HR, Yang JW, Yang P, Kim JR
and Kim YM: Trochanteric rotational osteotomy for osteonecrosis of
the femoral head. J Bone Joint Surg Br. 83:83–89. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Eyb R and Kotz R: The transtrochanteric
anterior rotational osteotomy of Sugioka. Early and late results in
idiopathic aseptic femoral head necrosis. Arch Orthop Trauma Surg.
106:161–167. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hiranuma Y, Atsumi T, Kajiwara T, Tamaoki
S and Asakura Y: Evaluation of instability after transtrochanteric
anterior rotational osteotomy for nontraumatic osteonecrosis of the
femoral head. J Orthop Sci. 14:535–542. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Yamamoto T, Ikemura S, Iwamoto Y and
Sugioka Y: The repair process of osteonecrosis after a
transtrochanteric rotational osteotomy. Clin Orthop Relat Res.
468:3186–3191. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Dean MT and Cabanela ME: Transtrochanteric
anterior rotational osteotomy for avascular necrosis of the femoral
head. Long-term results. J Bone Joint Surg Br. 75:597–601.
1993.PubMed/NCBI
|
|
19
|
Mont MA and Hungerford DS: Non-traumatic
avascular necrosis of the femoral head. J Bone Joint Surg Am.
77:459–474. 1995.PubMed/NCBI
|
|
20
|
Lavernia CJ, Sierra RJ and Grieco FR:
Osteonecrosis of the femoral head. J Am Acad Orthop Surg.
7:250–261. 1999.PubMed/NCBI
|
|
21
|
Okazaki S, Nagoya S, Tateda K, et al:
Weight bearing does not contribute to the development of
osteonecrosis of the femoral head. Int J Exp Pathol. 93:458–462.
2012.PubMed/NCBI
|
|
22
|
Ohzono K, Saito M, Takaoka K, et al:
Natural history of nontraumatic avascular necrosis of the femoral
head. J Bone Joint Surg Br. 73:68–72. 1991.PubMed/NCBI
|
|
23
|
Tetik C, Başar H, Bezer M, Erol B, Ağir I
and Esemenli T: Comparison of early results of vascularized and
non-vascularized fibular grafting in the treatment of osteonecrosis
of the femoral head. Acta Orthop Traumatol Turc. 45:326–334.
2011.PubMed/NCBI
|
|
24
|
Seyler TM, Marker DR, Ulrich SD, Fatscher
T and Mont MA: Nonvascularized bone grafting defers joint
arthroplasty in hip osteonecrosis. Clin Orthop Relat Res.
466:1125–1132. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Mont MA, Marulanda GA, Seyler TM, Plate JF
and Delanois RE: Core decompression and nonvascularized bone
grafting for the treatment of early stage osteonecrosis of the
femoral head. Instr Course Lect. 56:213–220. 2007.PubMed/NCBI
|
|
26
|
Kim SY, Kim YG, Kim PT, Ihn JC, Cho BC and
Koo KH: Vascularized compared with nonvascularized fibular grafts
for large osteonecrotic lesions of the femoral head. J Bone Joint
Surg Am. 87:2012–2018. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Mont MA, Etienne G and Ragland PS: Outcome
of nonvascularized bone grafting for osteonecrosis of the femoral
head. Clin Orthop Relat Res. 417:84–92. 2003.PubMed/NCBI
|
|
28
|
Rosenwasser MP, Garino JP, Kiernan HA and
Michelsen CB: Long term followup of thorough debridement and
cancellous bone grafting of the femoral head for avascular
necrosis. Clin Orthop Relat Res. 306:17–27. 1994.PubMed/NCBI
|
|
29
|
Soucacos PN, Beris AE, Malizos K,
Koropilias A, Zalavras H and Dailiana Z: Treatment of avascular
necrosis of the femoral head with vascularized fibular transplant.
Clin Orthop Relat Res. 386:120–130. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Marciniak D, Furey C and Shaffer JW:
Osteonecrosis of the femoral head. A study of 101 hips treated with
vascularized fibular grafting. J Bone Joint Surg Am. 87:742–747.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Malizos KN, Soucacos PN and Beris AE:
Osteonecrosis of the femoral head. Hip salvaging with implantation
of a vascularized fibular graft. Clin Orthop Relat Res. 314:67–75.
1995.PubMed/NCBI
|
|
32
|
Sakamoto A, Yoshida T, Uchida Y, Kojima T,
Kubota H and Iwamoto Y: Long-term follow-up on the use of
vascularized fibular graft for the treatment of congenital
pseudarthrosis of the tibia. J Orthop Surg Res. 3:132008.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Zhang C, Zeng B, Xu Z, et al: Treatment of
femoral head necrosis with free vascularized fibula grafting: a
preliminary report. Microsurgery. 25:305–309. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Berend KR, Gunneson EE and Urbaniak JR:
Free vascularized fibular grafting for the treatment of
postcollapse osteonecrosis of the femoral head. J Bone Joint Surg
Am. 85-A:987–993. 2003.PubMed/NCBI
|
|
35
|
Liang K, Xiang Z, Chen S, et al: Folded
free vascularized fibular grafts for the treatment of
subtrochanteric fractures complicated with segmental bone defects.
J Trauma Acute Care Surg. 72:1404–1410. 2012.PubMed/NCBI
|
|
36
|
Watters TS, Browne JA, Orlando LA, Wellman
SS, Urbaniak JR and Bolognesi MP: Cost-effectiveness analysis of
free vascularized fibular grafting for osteonecrosis of the femoral
head. J Surg Orthop Adv. 20:158–167. 2011.PubMed/NCBI
|
|
37
|
Kawate K, Yajima H, Sugimoto K, et al:
Indications for free vascularized fibular grafting for the
treatment of osteonecrosis of the femoral head. BMC Musculoskelet
Disord. 8:782007. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Yin S, Zhang C, Jin D, Chen S, Sun Y and
Sheng J: Treatment of osteonecrosis of the femoral head in lymphoma
patients by free vascularised fibular grafting. Int Orthop.
35:1125–1130. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Feng Y, Wang S, Jin D, et al: Free
vascularised fibular grafting with OsteoSet®2
demineralised bone matrix versus autograft for large osteonecrotic
lesions of the femoral head. Int Orthop. 35:475–481.
2011.PubMed/NCBI
|
|
40
|
Cohen R: A porous tantalum trabecular
metal: basic science. Am J Orthop (Belle Mead NJ). 31:216–217.
2002.PubMed/NCBI
|
|
41
|
Stronach BM, Duke JN, Rozensweig SD and
Stewart RL: Subtrochanteric femur fracture after core decompression
and placement of a tantalum strut for osteonecrosis of the femoral
head. J Arthroplasty. 25:1168.e5–1168.e7. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Aldegheri R, Taglialavoro G and Berizzi A:
The tantalum screw for treating femoral head necrosis: rationale
and results. Strategies Trauma Limb Reconstr. 2:63–68. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Varitimidis SE, Dimitroulias AP,
Karachalios TS, Dailiana ZH and Malizos KN: Outcome after tantalum
rod implantation for treatment of femoral head osteonecrosis: 26
hips followed for an average of 3 years. Acta Orthop. 80:20–25.
2009.PubMed/NCBI
|
|
44
|
Schnieders MJ, Dave SB, Morrow DE, Heiner
AD, Pedersen DR and Brown TD: Assessing the accuracy of a prototype
drill guide for fibular graft placement in femoral head necrosis.
Iowa Orthop J. 58–63. 1997.PubMed/NCBI
|
|
45
|
Liu B, Sun W, Yue D, Li Z and Guo W:
Combined tantalum implant with bone grafting for the treatment of
osteonecrosis of the femoral head. J Invest Surg. 26:158–162. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Samara S, Dailiana Z, Chassanidis C,
Koromila T, Papatheodorou L, Malizos KN and Kollia P: Expression
profile of osteoprotegerin, RANK and RANKL genes in the femoral
head of patients with avascular necrosis. Exp Mol Pathol. 96:9–14.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Fan M, Jiang WX, Wang AY, Wang Y, Peng J,
Zhang L, Xu WJ and Lu SB: Effect and mechanism of zoledronate on
prevention of collapse in osteonecrosis of the femoral head.
Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 34:330–336. 2012.(In
Chinese).
|
|
48
|
Wang C, Wang X, Xu XL, Yuan XL, Gou WL,
Wang AY, Guo QY, Peng J and Lu SB: Bone microstructure and regional
distribution of osteoblast and osteoclast activity in the
osteonecrotic femoral head. PLoS One. 9:e963612014. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Wang CJ: Extracorporeal shockwave therapy
in musculoskeletal disorders. J Orthop Surg Res. 7:112012.
View Article : Google Scholar
|
|
50
|
Yin TC, Wang CJ, Yang KD, Wang FS and Sun
YC: Shockwaves enhance the osteogenetic gene expression in marrow
stromal cells from hips with osteonecrosis. Chang Gung Med J.
34:367–374. 2011.PubMed/NCBI
|
|
51
|
Ludwig J, Lauber S, Lauber HJ, Dreisilker
U, Raedel R and Hotzinger H: High-energy shock wave treatment of
femoral head necrosis in adults. Clin Orthop Relat Res.
387:119–126. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Wang CJ, Wang FS, Huang CC, Yang KD, Weng
LH and Huang HY: Treatment for osteonecrosis of the femoral head:
comparison of extracorporeal shock waves with core decompression
and bone-grafting. J Bone Joint Surg Am. 87:2380–2387. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Alves EM, Angrisani AT and Santiago MB:
The use of extracorporeal shock waves in the treatment of
osteonecrosis of the femoral head: a systematic review. Clin
Rheumatol. 28:1247–1251. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Turner DA, Templeton AC, Selzer PM,
Rosenberg AG and Petasnick JP: Femoral capital osteonecrosis: MR
finding of diffuse marrow abnormalities without focal lesions.
Radiology. 71:135–140. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Hofmann S, Schneider W, Breitenseher M,
Urban M and Plenk H Jr: ‘Transient osteoporosis’ as a special
reversible form of femur head necrosis. Orthopade. 29:411–419.
2000.(In German).
|
|
56
|
Yang JC, Pan ZY, Gu H, Li N, Qian XJ, Zhai
RY, Wu LH and Gao CJ: Quantitative study of therapeutic efficacy on
early intervention of hyperbaric oxygen to model of steroid-induced
avascular osteonecrosis of femoral head by multi-slice perfusion
imaging. Zhonghua Yi Xue Za Zhi. 88:3210–3216. 2008.(In
Chinese).
|
|
57
|
Camporesi EM, Vezzani G, Bosco G, Mangar D
and Bernasek TL: Hyperbaric oxygen therapy in femoral head
necrosis. J Arthroplasty. 25:118–123. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Reis ND, Schwartz O, Militianu D, et al:
Hyperbaric oxygen therapy as a treatment for stage-I avascular
necrosis of the femoral head. J Bone Joint Surg Br. 85:371–375.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Ficat P, Arlet J, Vidal R, Ricci A and
Fournial JC: Therapeutic results of drill biopsy in primary
osteonecrosis of the femoral head (100 cases). Rev Rhum Mal
Osteoartic. 38:269–276. 1971.(In French).
|
|
60
|
Lieberman JR, Conduah A and Urist MR:
Treatment of osteonecrosis of the femoral head with core
decompression and human bone morphogenetic protein. Clin Orthop
Relat Res. 429:139–145. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Lieberman JR: Core decompression for
osteonecrosis of the hip. Clin Orthop Relat Res. 418:29–33. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Mont MA, Ragland PS and Etienne G: Core
decompression of the femoral head for osteonecrosis using
percutaneous multiple small-diameter drilling. Clin Orthop Relat
Res. 429:131–138. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Steinberg ME, Brighton CT, Corces A, et
al: Osteonecrosis of the femoral head. Results of core
decompression and grafting with and without electrical stimulation.
Clin Orthop Relat Res. 249:199–208. 1989.PubMed/NCBI
|
|
64
|
Trancik T, Lunceford E and Strum D: The
effect of electrical stimulation on osteonecrosis of the femoral
head. Clin Orthop Relat Res. 256:120–124. 1990.PubMed/NCBI
|
|
65
|
Steinberg ME, Brighton CT, Bands RE and
Hartman KM: Capacitive coupling as an adjunctive treatment for
avascular necrosis. Clin Orthop Relat Res. 261:11–18.
1990.PubMed/NCBI
|
|
66
|
Steinberg ME: Core decompression of the
femoral head for avascular necrosis: indications and results. Can J
Surg. 38(Suppl 1): S18–S24. 1995.PubMed/NCBI
|
|
67
|
Marker DR, Seyler TM, Ulrich SD,
Srivastava S and Mont MA: Do modern techniques improve core
decompression outcomes for hip osteonecrosis? Clin Orthop Relat
Res. 466:1093–1103. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Rackwitz L, Eden L, Reppenhagen S, et al:
Stem cell- and growth factor-based regenerative therapies for
avascular necrosis of the femoral head. Stem Cell Res Ther.
3:72012. View
Article : Google Scholar : PubMed/NCBI
|
|
69
|
Helbig L, Simank HG, Kroeber M,
Schmidmaier G, Grützner PA and Guehring T: Core decompression
combined with implantation of a demineralised bone matrix for
non-traumatic osteonecrosis of the femoral head. Arch Orthop Trauma
Surg. 132:1095–1103. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Liu Y, Liu S and Su X: Core decompression
and implantation of bone marrow mononuclear cells with porous
hydroxylapatite composite filler for the treatment of osteonecrosis
of the femoral head. Arch Orthop Trauma Surg. 133:125–133. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Wang W, Liu L, Dang X, Ma S, Zhang M and
Wang K: The effect of core decompression on local expression of
BMP-2, PPAR-γ and bone regeneration in the steroid-induced femoral
head osteonecrosis. BMC Musculoskelet Disord. 13:1422012.PubMed/NCBI
|
|
72
|
Xie XH, Wang XL, He YX, et al: Promotion
of bone repair by implantation of cryopreserved bone marrow-derived
mononuclear cells in a rabbit model of steroid-associated
osteonecrosis. Arthritis Rheum. 64:1562–1571. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Wei BF and Ge XH: Treatment of
osteonecrosis of the femoral head with core decompression and bone
grafting. Hip Int. 21:206–210. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Li W, Sakai T, Nishii T, et al:
Distribution of TRAP-positive cells and expression of HIF-1α, VEGF,
and FGF-2 in the reparative reaction in patients with osteonecrosis
of the femoral head. J Orthop Res. 27:694–700. 2009.
|
|
75
|
Zaidi M, Sun L, Robinson LJ, et al: ACTH
protects against glucocorticoid-induced osteonecrosis of bone. Proc
Natl Acad Sci USA. 107:8782–8787. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Gao YS, Wang HF, Ding H and Zhang CQ: A
novel rat model of osteonecrosis of the femoral head induced by
periarticular injection of vascular endothelial growth factor
receptor 2 antibody. J Surg Res. 183:e1–e5. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Zhang C, Li Y, Cornelia R, Swisher S and
Kim H: Regulation of VEGF expression by HIF-1α in the femoral head
cartilage following ischemia osteonecrosis. Sci Rep. 2:6502012.
|
|
78
|
Trueta J and Buhr AJ: The vascular
contribution to osteogenesis. V The vasculature supplying the
epiphysial cartilage in rachitic rats. J Bone Joint Surg Br.
45:572–581. 1963.PubMed/NCBI
|
|
79
|
Cao K, Huang W, An H, Jiang DM, Shu Y and
Han ZM: Deproteinized bone with VEGF gene transfer to facilitate
the repair of early avascular necrosis of femoral head of rabbit.
Chin J Traumatol. 12:269–274. 2009.PubMed/NCBI
|
|
80
|
Hang D, Wang Q, Guo C, Chen Z and Yan Z:
Treatment of osteonecrosis of the femoral head with VEGF165
transgenic bone marrow mesenchymal stem cells in mongrel dogs.
Cells Tissues Organs. 195:495–506. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Rizzoli R: Bisphosphonates treatment in
patients with osteoporosis. Ther Umsch. 69:173–181. 2012.(In
German).
|
|
82
|
Gou W, Wang X, Peng J, et al: Controlled
delivery of zoledronate improved bone formation locally in vivo.
PLoS One. 9:e913172014. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Hayes WC, Shea M and Rodan GA: Preclinical
evidence of normal bone with alendronate. Int J Clin Pract Suppl.
101:9–13. 1999.PubMed/NCBI
|
|
84
|
Agarwala S, Sule A, Pai BU and Joshi VR:
Study of alendronate in avascular necrosis of bone. J Assoc
Physicians India. 49:949–950. 2001.PubMed/NCBI
|
|
85
|
Agarwala S, Sule A, Pai BU and Joshi VR:
Alendronate in the treatment of avascular necrosis of the hip.
Rheumatology (Oxford). 41:346–347. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Peled E, Bejar J, Barak M, Orion E and
Norman D: Core decompression and alendronate treatment of the
osteonecrotic rat femoral head: computer-assisted analysis. Int J
Exp Pathol. 94:212–216. 2013.PubMed/NCBI
|
|
87
|
Agarwala S, Jain D, Joshi VR and Sule A:
Efficacy of alendronate, a bisphosphonate, in the treatment of AVN
of the hip. A prospective open-label study. Rheumatology (Oxford).
44:352–359. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Wong PK, Borromeo GL and Wark JD:
Bisphosphonate-related osteonecrosis of the jaw in non-malignant
bone disease. Rheumatol Int. 33:2189–2198. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Outeiriño-Fernández A: Osteonecrosis of
the jaw associated with bisphosphonate therapy in primary
osteoporosis. Review of the literature. An Sist Sanit Navar.
36:87–97. 2013.(In Spanish).
|
|
90
|
Chiu WY, Lee JJ and Tsai KS: Atypical
femoral fractures shortly after osteonecrosis of the jaw in a
postmenopausal woman taking alendronate for osteoporosis. J Clin
Endocrinol Metab. 98:E723–E726. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Conte Neto N, Spolidorio LC, Andrade CR,
Bastos SA, Guimarães M and Marcantonio E Jr: Experimental
development of bisphosphonate-related osteonecrosis of the jaws in
rodents. Int J Exp Pathol. 94:65–73. 2013.PubMed/NCBI
|
|
92
|
Arranz Caso JA, Flores Ballester E, Ngo
Pombe S, López Pizarro V, Dominguez-Mompello JL and Restoy Lozano
A: Bisphosphonate related osteonecrosis of the jaw and infection
with Actinomyces. Med Clin (Barc). 139:676–680. 2012.(In
Spanish).
|
|
93
|
Schaudinn C, Gorur A, Webster P, et al:
Quantification by energy dispersive X-ray spectroscopy of
alendronate in the diseased jaw bone of patients with
bisphosphonate-related jaw osteonecrosis. Oral Surg Oral Med Oral
Pathol Oral Radiol. 114:480–486. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Bocanegra-Pérez MS, Vicente-Barrero M,
Sosa-Henríquez M, et al: Bone metabolism and clinical study of 44
patients with bisphosphonate-related osteonecrosis of the jaws. Med
Oral Patol Oral Cir Bucal. 17:e948–e955. 2012.PubMed/NCBI
|