Introduction
Inflammatory bowel diseases (IBDs), which include
ulcerative colitis (UC) and Crohn’s disease (CD), are chronic
inflammatory disorders of the gastrointestinal tract. Currently, a
number of drugs, including 5-aminosalicylic acid (5-ASA) drugs, for
example sulfasalazine (SASP) and mesalazine, are used for the
treatment of UC (1). In addition,
corticosteroids, azathioprine and mercaptopurine are also used for
treatment of UC (2). However,
these drugs are not the optimal choice for long-term treatment and
are used only if patients do not achieve remission with 5-ASA
(3). Furthermore, these drugs have
significant risk factors, including an increased risk of cancer,
tuberculosis and heart failure (4). Therefore, the development of a novel
strategy for the treatment of UC is of importance.
Notably, ~21% of patients with IBD use alternative
treatments (5). Complementary and
alternative medicine (CAM) is becoming increasingly popular and is
used to treat patients with UC in China. CAM is considered as an
effective adjunct treatment by physicians and patients.
Banxiaxiexin decoction, containing seven commonly used plants
(Pinellia ternata, Scutellaria baicalensis, ginseng,
Rhizoma Coptidis, liquorice, ginger and red jujube), is a classical
Chinese medicine formulation. It has been widely used for centuries
to treat IBD in clinical practice in China (6). This traditional Chinese medicine
formulation is a promising agent for the treatment of many chronic
gastrointestinal diseases, including chronic gastritis, peptic
ulcer disease and certain chronic intestinal diseases. However, the
use of Banxiaxiexin decoction for the treatment of UC has yet to be
reported, and the pharmacological mechanism is not yet clearly
defined. Further studies are required prior to it being recommended
for treatment of UC.
Therefore, the aim of the present study was to
investigate the efficacy of Banxiaxiexin decoction for the
treatment of UC. To analyze the therapeutic effects of novel drugs,
an appropriate animal model is necessary. A modified experimental
model of UC in BALB/c mice was established in the present study. A
low dose of the haptenating agent oxazolone (OXA) was used to
induce colitis. OXA promotes the production of Th-2 type cytokines,
resulting in lesions characterized by lymphocyte infiltration.
Materials and methods
Animals
The study protocol was approved by the ethics
committee of Shanghai University of Traditional Chinese Medicine
(Shanghai, China) and performed in accordance with the Guide for
the Care and Use of Laboratory Animals (7). Male BALB/c mice were obtained from
the Shanghai Laboratory Animal Center (Shanghai, China).
Specific-pathogen-free male BALB/c mice, weighing 18–20 g, were
used for the OXA-induced colitis model. Mice were housed in
polycarbonate cages and fed a standard chow and tap water ad
libitum.
Induction of colitis
Colitis was induced as previously described, with
modifications (8). Briefly, a 2x2
cm field of the abdominal skin was shaved, and 200 μl 3% OXA
(Sigma, St. Louis, MO, USA) in 100% ethanol was applied to
pre-sensitize the BALB/c mice, and this was repeated the next day.
Then, each BALB/c mouse was slightly anesthetized with 0.2%
pentobarbital intraperitoneally. A 3.5-F polyurethane catheter was
inserted 4 cm into the lumen of the colon, via the anus. A solution
of OXA (150 μl; 1% OXA dissolved in 50% ethanol) was administered
into the colon via the catheter. Following injection of the OXA
solution, the catheter was removed and the mouse was held
vertically for 60 sec. For the control group, the same amount of
ethanol was injected, instead of OXA solution.
Preparation of water-soluble extracts of
Banxiaxiexin decoction and intragastric administration of SASP and
the water-soluble extracts
The Banxiaxiexin decoction consists of Pinellia
ternata 12 g, Scutellaria baicalensis 6 g, ginseng 9 g,
Rhizoma Coptidis 3 g, liquorice 9 g, ginger 9 g and four red jujube
fruits. To obtain the water-soluble extracts, a volume of water
10-fold greater than that of the decoction was added, and the
resulting mixture was heated for 1 h. This was repeated three
times. Then, all the extraction liquids were collected, dried and
stored at 4°C.
Extracts of the decoction were administered
intragastrically (10 mg/g bodyweight) to the OXA-treated BALB/c
mice to establish the Banxia group. SASP intragastric
administration (20 mg/g bodyweight) was used to treat the
OXA-treated mice in the SASP group, which acted as a positive
control. Even though there was no specific interval between
administration of OXA and decoction/SASP treatment, the mice were
held vertically for 60 sec. Intragastric administration of the
decoction extract or SASP was performed once a day for 7 days. In
the model group, an equal volume of water was administered to the
OXA-treated mice.
Disease activity index (DAI)
analysis
The DAI was determined at the end of the treatment
period, according to the parameters outlined in Table I.
 | Table IDisease activity index. |
Table I
Disease activity index.
| Score | Percentage weight
loss | Stool
consistency | Hematochezia
level |
|---|
| 0 | 0 | Normal | Negative
hemoccult |
| 1 | 1–5 | | |
| 2 | 5–10 | Mushy | Positive
hemoccult |
| 3 | 10–15 | | |
| 4 | ≥15 | Diarrhea | Blood traces visible
in stool |
Histological analysis
The mice were sacrificed at end of the treatment
period. Colonic tissues were dissected and washed with Hank’s
balanced salt solution (containing 10 μg/ml gentamicin, 100 U/ml
penicillin and 100 μg/ml streptomycin). The tissues were then fixed
in 10% natural buffered formalin, embedded in paraffin, cut into
tissue sections (5 μm thick) and stained with hematoxylin and eosin
(H&E). The stained sections were examined for evidence of
colitis using the Wirtz’s criteria (9) (Table
II).
 | Table IIScoring system for
inflammation-associated histological changes in the colon. |
Table II
Scoring system for
inflammation-associated histological changes in the colon.
| Score | Histological
changes |
|---|
| 0 | No evidence of
inflammation |
| 1 | Low level of
inflammation with scattered infiltrating mononuclear cells (1–2
foci) |
| 2 | Moderate inflammation
with multiple foci |
| 3 | Severe inflammation
with increased vascular density and marked wall thickening |
| 4 | Maximal severity of
inflammation with transmural leukocyte infiltration and loss of
goblet cells |
Analyses of mRNA expression levels of
interleukin (IL)-5 and IL-13 by quantitative polymerase chain
reaction (qPCR)
Total RNA was extracted from the colon after the 7
days of therapy (after colitis induction) using the
TRIzol® method (TRIzol reagent; Invitrogen Life
Technologies, Carlsbad, CA, USA) (10). Reverse transcription was performed
using a cDNA Synthesis kit (Sangon Biotech, Shanghai, China), in
accordance with the manufacturer’s instructions. qPCR was performed
in a 10 μl final volume containing the following: 5 μl 2X SYBR
Green I master mix (Qiagen, Hilden, Germany); 1 μl 5 μM forward
primer and 1 μl 5 μM reverse primer (IL-5 primers: forward,
5′-AAGGATGCTTCTGCACTTGA-3′ and reverse, 3′-GGAAGCCTCATCGTCTCATT-5′,
IL-13 primers: forward, 5′-AGCATGGTATGGAGTGTGGA-3′ and reverse,
3′-TTGCAATTGGAGATGTTGGT-5′); and 3 μl diluted cDNA. Following an
initial denaturation step at 50°C for 2 min and 95°C for 10 min,
temperature cycling was initiated. Each cycle consisted of
denaturation at 95°C for 15 sec, annealing at 60°C for 1 min and
elongation at 72°C for 20 sec. In total, 40 cycles were performed.
Mouse β-actin was used as the control for normalizing the
quantities of transcripts of IL-5 and IL-13.
Statistical analysis
The SNK-q test was used to compare the distributions
of the groups. P<0.05 was considered to indicate a statistically
significant difference. Data were analyzed using SPSS software,
version 13.0 (SPSS, Inc., Chicago, IL, USA).
Results
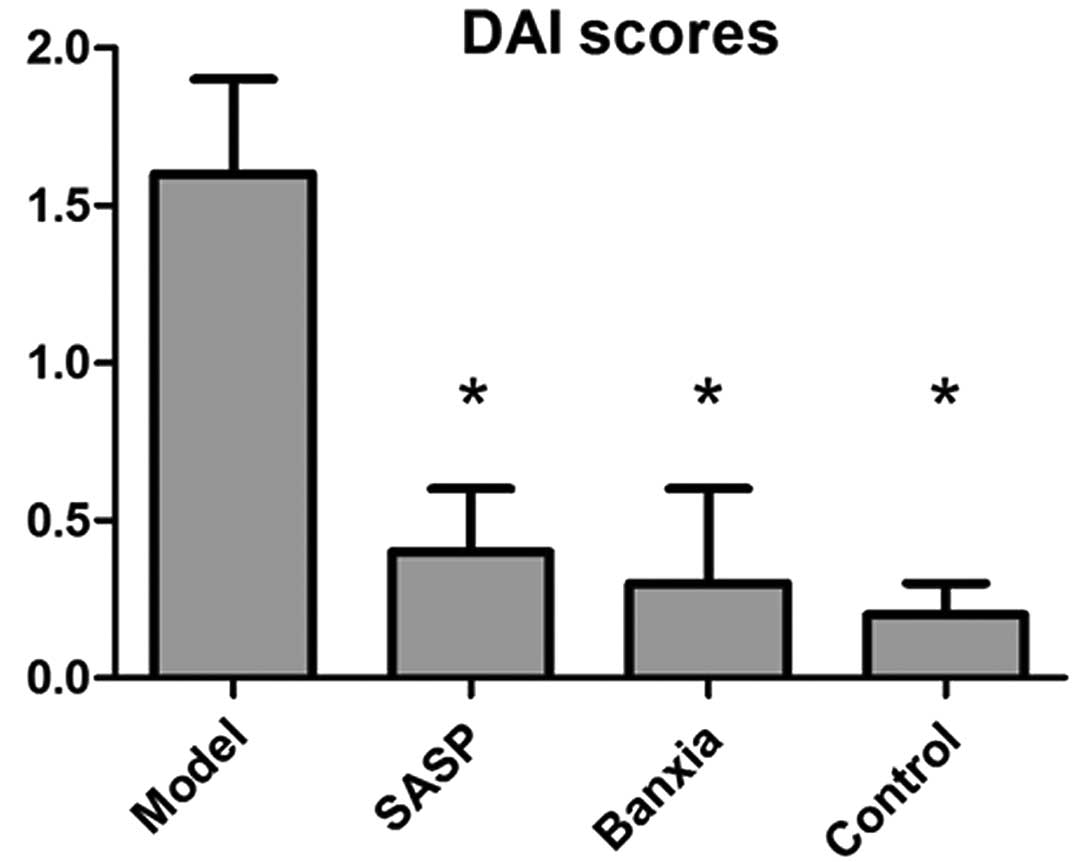
DAI score
The appearance of the fur, vitality, weight,
appetite and stools in the control group were normal. Yellow fur,
lethargy, depression, loss of appetite, significant weight loss,
diarrhea and bloody stools were observed in the OXA-induced mice.
The condition of the mice following treatment with SASP or
Banxiaxiexin decoction was significantly better than that of the
mice in the model group. The DAI scores for the mice in those
groups are shown in Fig. 1. The
DAI score of the model group was significantly higher compared with
that of the control group (P<0.05). The DAI scores of the SASP
and Banxia groups were significantly lower compared with that of
the model group (P<0.05); however, no significant difference
between the SASP and Banxia groups was observed.
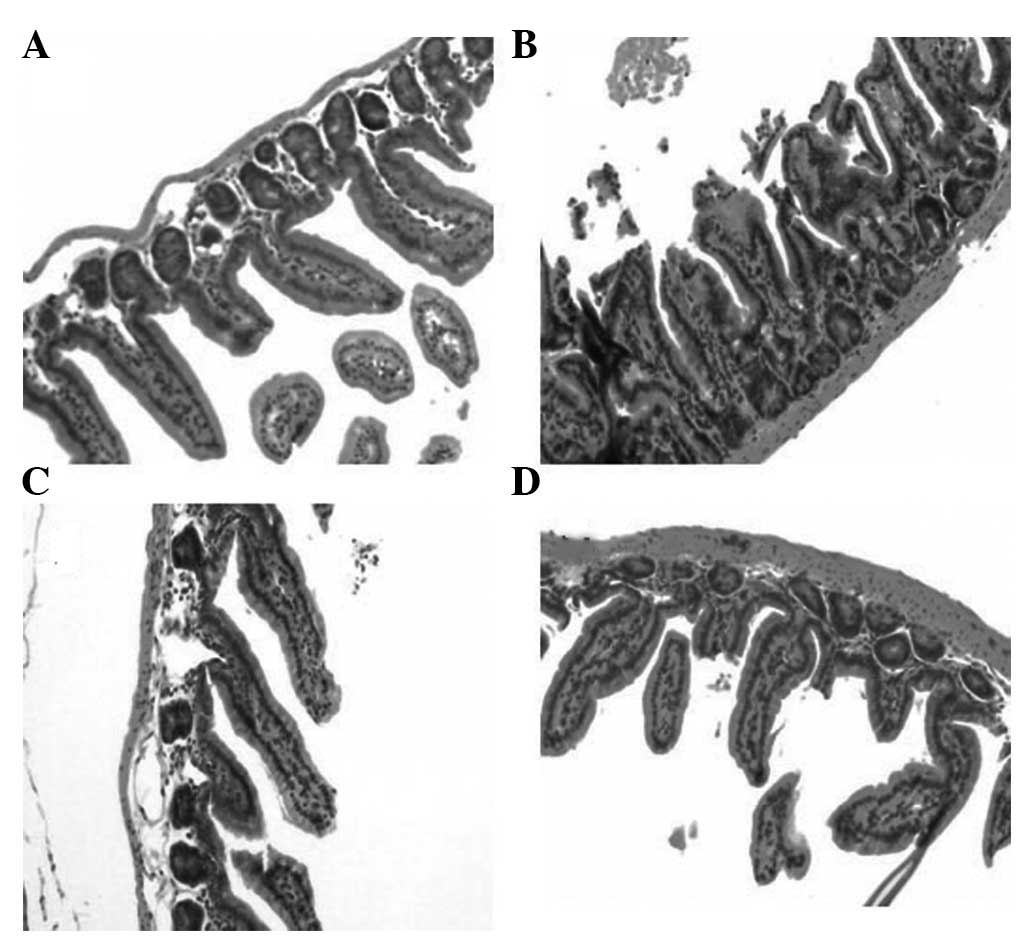
Histological examination of
inflammation
Histological examination of colonic sections from
the OXA-treated mice revealed mucosal inflammation, characterized
by the presence of mononuclear cell infiltration, primarily
lymphocytes, monocytes and plasma cells, but also neutrophils and
eosinophils, a reduction of goblet cells, increased vascular
density and a thickening of the colonic wall. These lesions were
reduced in severity in the SASP and Banxia groups (Fig. 2). Scores for the
inflammation-associated histological changes in the colon for the
model, SASP, Banxia and control groups are shown in Table III. The score was significantly
increased in the model group compared with that in the control
group. Furthermore, scores were decreased in the SASP and Banxia
groups compared with that in the model group. However, no
significant difference was identified between the SASP and Banxia
groups.
 | Table IIIScores for inflammation-associated
histological changes (mean ± SD). |
Table III
Scores for inflammation-associated
histological changes (mean ± SD).
| Parameter | Model | SASP | Banxia | Control |
|---|
| N | 10 | 10 | 10 | 10 |
| Scores | 2.7±0.7 | 1.3±0.6 | 1.5±0.4 | 1.7±0.5 |
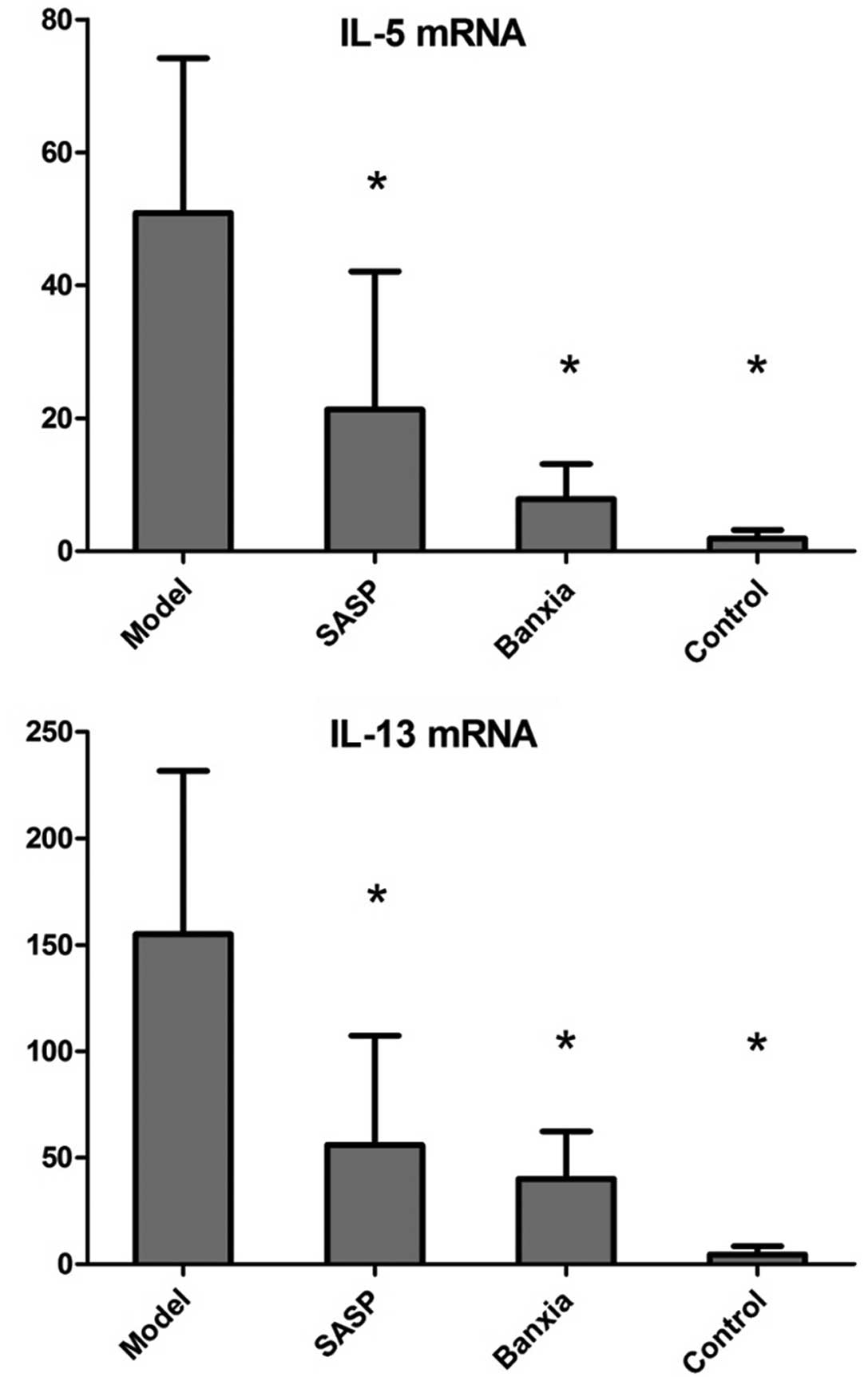
mRNA expression of IL-5 and IL-13
The expression levels of IL-5 mRNA were
significantly increased in the model group compared with those in
the control group; however, the expression levels were decreased in
the SASP and Banxia groups, compared with those in the model group.
Similar to IL-5, the expression levels of IL-13 mRNA were also
significantly increased in the mice treated with OXA compared with
those in the control group. OXA-treated mice that received SASP or
Banxiaxiexin decoction exhibited significant reductions in the
expression level of IL-13 mRNA. However, no significant difference
was identified in the expression levels of IL-5 and IL-13 mRNA
between the SASP- and Banxia decoction-treated mice. The expression
levels of IL-5 and IL-13 mRNA for the different groups are shown in
Fig. 3.
Discussion
In the present study, the therapeutic effects of the
water-soluble extracts from the traditional Chinese medicine
formulation Banxiaxiexin decoction on UC in an animal model was
investigated. UC was induced in BALB/c mice by the intrarectal
administration of a low dose of OXA, following skin sensitization
with OXA. Morphological changes, analyzed using histological
methods, were similar to the tissue damage observed in patients
with UC. The morphological changes were characterized by a
thickening of the colonic wall, depletion of goblet cells,
increased vascular density and lymphocyte infiltration.
SASP, a 5-ASA drug used for the treatment of IBD,
and the water-soluble extracts from Banxiaxiexin decoction, were
used in the present study for the treatment of UC. It was found
that Banxiaxiexin decoction exerted a significant anti-inflammatory
effect and the therapeutic effect of the Banxiaxiexin decoction was
found to be similar to that of SASP. BALB/c mice treated with
Banxiaxiexin decoction showed improvements in body weight and the
appearance of feces, and alleviation of bloody stools. Furthermore,
the DAI score, an indicator of the severity of intestinal
inflammation, was increased in the model group, but decreased in
the SASP and Banxia treatment groups.
The mRNA expression levels of cytokines from
mononuclear cells, primarily CD4+ T-helper-2 (Th-2)
cells and NK-T cells, were determined using qPCR. Increased IL-5
and IL-13 mRNA expression levels were observed in the model group.
A previous study suggested that disruption of the intestinal
mucosal immune system is involved in the pathogenesis of IBD
(11). Several pathways, including
the Th-1 and Th-2 immune response pathways, are considered to have
a role in development of IBD. It should be noted that the Th-1
immune response may have an important role in CD, whilst the Th-2
response may be involved in UC (12,13).
IL-5 and IL-13 are characteristic Th-2 cytokines involved in UC
(12). It has been previously
demonstrated that the overexpression of IL-5 significantly
increases the severity of OXA-induced colitis. Lack of IL-5 has
been shown to attenuate the accumulation of eosinophils in the
colon of dextran-sodium sulfate-treated mice (14). Eosinophils may reduce the barrier
properties of epithelial cell monolayers. In addition, preliminary
evidence suggests that eosinophil activation results in an increase
in epithelial permeability in biopsy specimens from patients with
UC (15). Eosinophils may enhance
intestinal inflammation via the induction of a reduction in
epithelial barrier function (16).
In the present study, no adverse effects of
Banxiaxiexin decoction were observed. However, the safety of this
decoction is not yet known, although it is widely believed that it
is safe to use herbal medicines for the treatment of various
diseases in China. Since numerous adverse effects of Chinese herbal
medicines have been reported, the long-term safety of Banxiaxiexin
decoction requires further investigation.
Acknowledgements
This study was supported by a grant the from Putuo
District Science and Technology Committee (no. 2010ptkw010).
Abbreviations:
|
IBD
|
inflammatory bowel diseases
|
|
UC
|
ulcerative colitis
|
|
CD
|
Crohn’s disease
|
|
5-ASA
|
5-aminosalicylic acid
|
|
CAM
|
complementary and alternative
medicine
|
|
OXA
|
oxazolone
|
|
SASP
|
sulfasalazine
|
|
DAI
|
disease activity index
|
|
DSS
|
dextran-sodium sulfate
|
References
|
1
|
Lee HJ, Jung ES, Lee JH, et al: Long-term
clinical outcomes and factors predictive of relapse after
5-aminosalicylate or sulfasalazine therapy in patients with
mild-to-moderate ulcerative colitis. Hepatogastroenterology.
59:1415–1420. 2012.PubMed/NCBI
|
|
2
|
Manz M, Vavricka SR, Wanner R, et al:
Therapy of steroid-resistant inflammatory bowel disease. Digestion.
86(Suppl 1): 11–15. 2012. View Article : Google Scholar
|
|
3
|
Taba Taba Vakili S, Taher M and Ebrahimi
Daryani N: Update on the management of ulcerative colitis. Acta Med
Iran. 50:363–372. 2012.PubMed/NCBI
|
|
4
|
Sutherland LR, May GR and Shaffer EA:
Sulfasalazine revisited: a meta-analysis of 5-aminosalicylic acid
in the treatment of ulcerative colitis. Ann Inter Med. 118:540–549.
1993. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Bensoussan M, Jovenin N, Garcia B, et al:
Complementary and alternative medicine use by patients with
inflammatory bowel disease: results from a postal survey.
Gastroenterol Clin Biol. 30:14–23. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Xu G: Treatment of reflux
laryngopharyngitis with modified Banxia Xiexin Tang
(Pinellia decoction for draining the heart) - a report of 40 cases.
J Tradit Chin Med. 26:127–131. 2006.PubMed/NCBI
|
|
7
|
Health NIO: Guide for the care and use of
laboratory animals. National Academies, National Academy Press;
1985
|
|
8
|
Heller F, Fuss IJ, Nieuwenhuis EE,
Blumberg RS and Strober W: Oxazolone colitis, a Th2 colitis model
resembling ulcerative colitis, is mediated by IL-13 producting NK-T
cells. Immunity. 17:629–638. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Wirtz S, Neufert C, Weigmann B and Neurath
MF: Chemically induced mouse models of intestinal inflammation. Nat
Protoc. 2:541–546. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ali SA and Alman B: RNA extraction from
human articular cartilage by chondrocyte isolation. Anal Biochem.
429:39–41. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bouma G and Strober W: The immunological
and genetic basis of inflammatory bowel disease. Nat Rev Immunol.
3:521–533. 2003. View
Article : Google Scholar : PubMed/NCBI
|
|
12
|
Fuss IJ, Neurath M, Boirivant M, et al:
Disparate CD4+ lamina propria (LP) lymphokine secretion profiles in
inflammatory bowel disease. Crohn’s disease LP cells manifest
increased secretion of IFN-gamma, whereas ulcerative colitis LP
cells manifest increased secretion of IL-5. J Immunol.
157:1261–1270. 1996.PubMed/NCBI
|
|
13
|
Kakazu T, Hara J, Matsumoto T, et al: Type
1 T-helper cell predominance in granulomas of Crohn’s disease. Am J
Gastroenterol. 94:2149–2155. 1999.
|
|
14
|
Lampinen M, Carlson M, Hakansson LD and
Venge P: Cytokine-regulated accumulation of eosinophils in
inflammatory disease. Allergy. 59:793–805. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Michail S and Abernathy F: A new model for
studying eosinophil migration across cultured intestinal epithelial
monolayers. J Pediatr Gastroenterol Nutr. 39:56–63. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Wang A, Fernando M, Leung G, Phan V, Smyth
D and McKay DM: Exacerbation of oxazolone colitis by infection with
the helminth Hymenolepsis diminuta: involvement of IL-5 and
eosinophils. Am J Pathol. 177:2850–2859. 2010. View Article : Google Scholar : PubMed/NCBI
|