Introduction
Ameloblastic fibrosarcoma (AFS) is a rare malignant
odontogenic neoplasm, first described by Heath in 1887 (1). AFS is composed of a benign
odontogenic epithelium and a malignant mesenchymal component
(2). The disease is characterized
by bone destruction and swelling with pain. To date, only 91
documented cases have been reported in the English literature. The
majority of AFS cases are located in the mandible and most commonly
involve the posterior region. It has previously been shown that AFS
can be regarded as the malignant counterpart of ameloblastic
fibroma (AF) (3); however, AFS can
also originate de novo (4).
In this case report, a new case of AFS arising from a pre-existing
AF is described. Furthermore, an analysis of the radiographic
appearances and immunochemical features, as well as a review of the
relevant literature, are presented. The patient provided written
informed consent for this study.
Case report
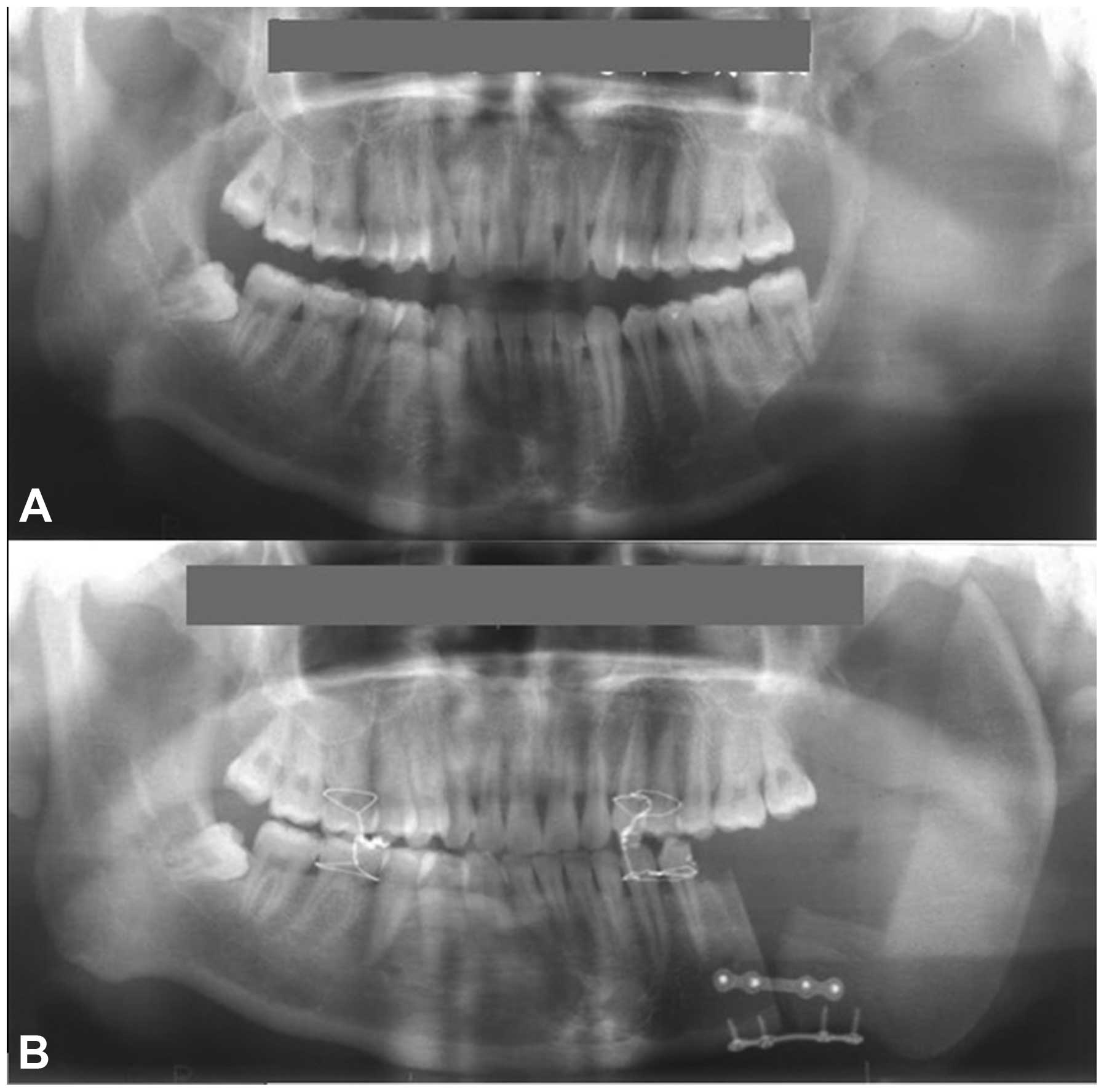
A 22-year-old Chinese male was referred to a local
hospital in March 2005 with a two-month history of a painful
swelling in his left mandible. Radiographic examination disclosed a
unilocular radiolucent lesion located in the left mandible
(Fig. 1A). An incisional biopsy
was performed and the histopathological diagnosis was AF. The
patient underwent left mandibulectomy and reconstruction with the
ilia and iliac myocutaneous free flap (Fig. 1B).
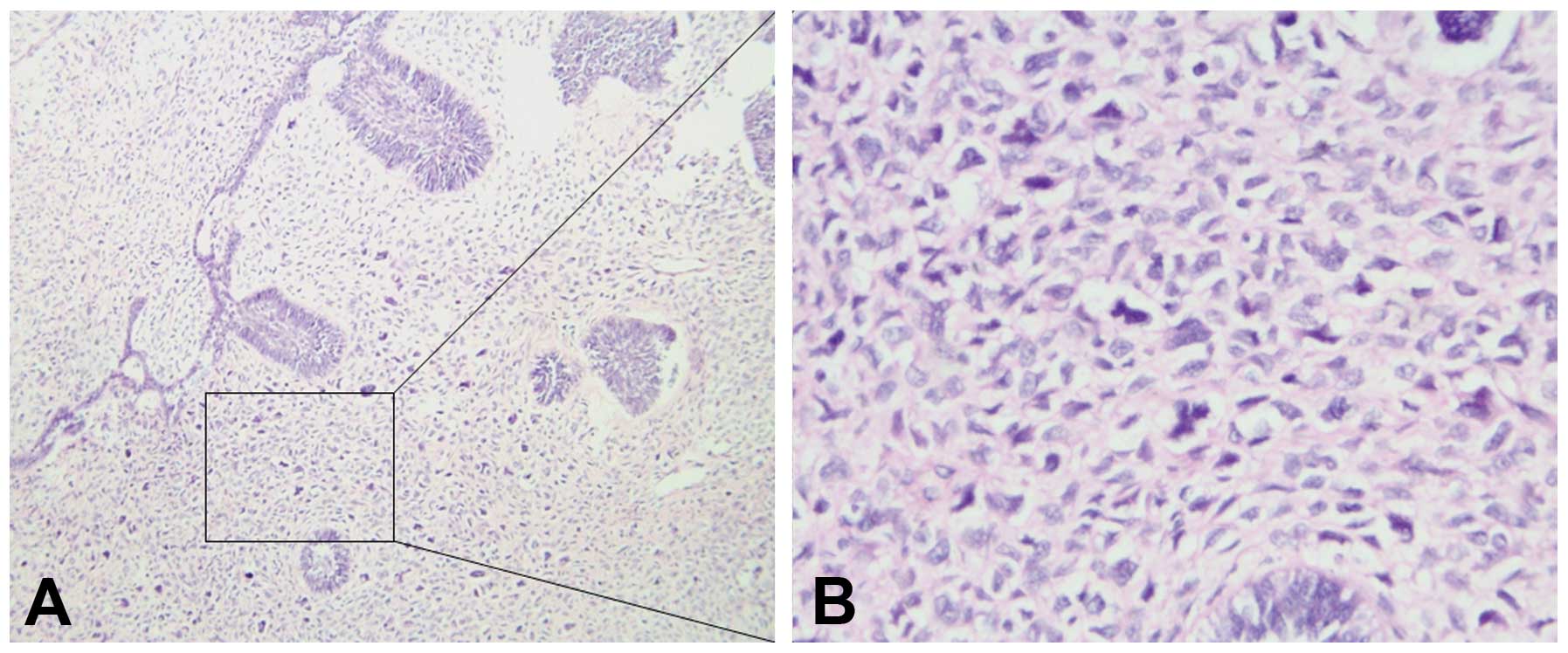
In September 2006, the patient came to our oral and
maxillofacial center at the Department of Stomatology, Taihe
Hospital (Hubei University of Medicine, Shiyan, China) and
complained of the recurrence of the mass and acute pain within the
last five months. Extraoral examination revealed a large, firm
swelling extending from the premolar to the temporomandibular joint
of the left mandible, as well as apparent asymmetry of the face.
Intraoral examination showed a firm swelling located in the
retromolar area of the left mandible, with ulceration of the
mucosal membranes. The panoramic radiograph showed an extensive,
ill-defined multilocular radiolucent area from the first premolar
to the ramus of the left mandible (Fig. 2). The computed tomography (CT) scan
revealed a 6.5×5.0 cm destructive lesion with bone resorption of
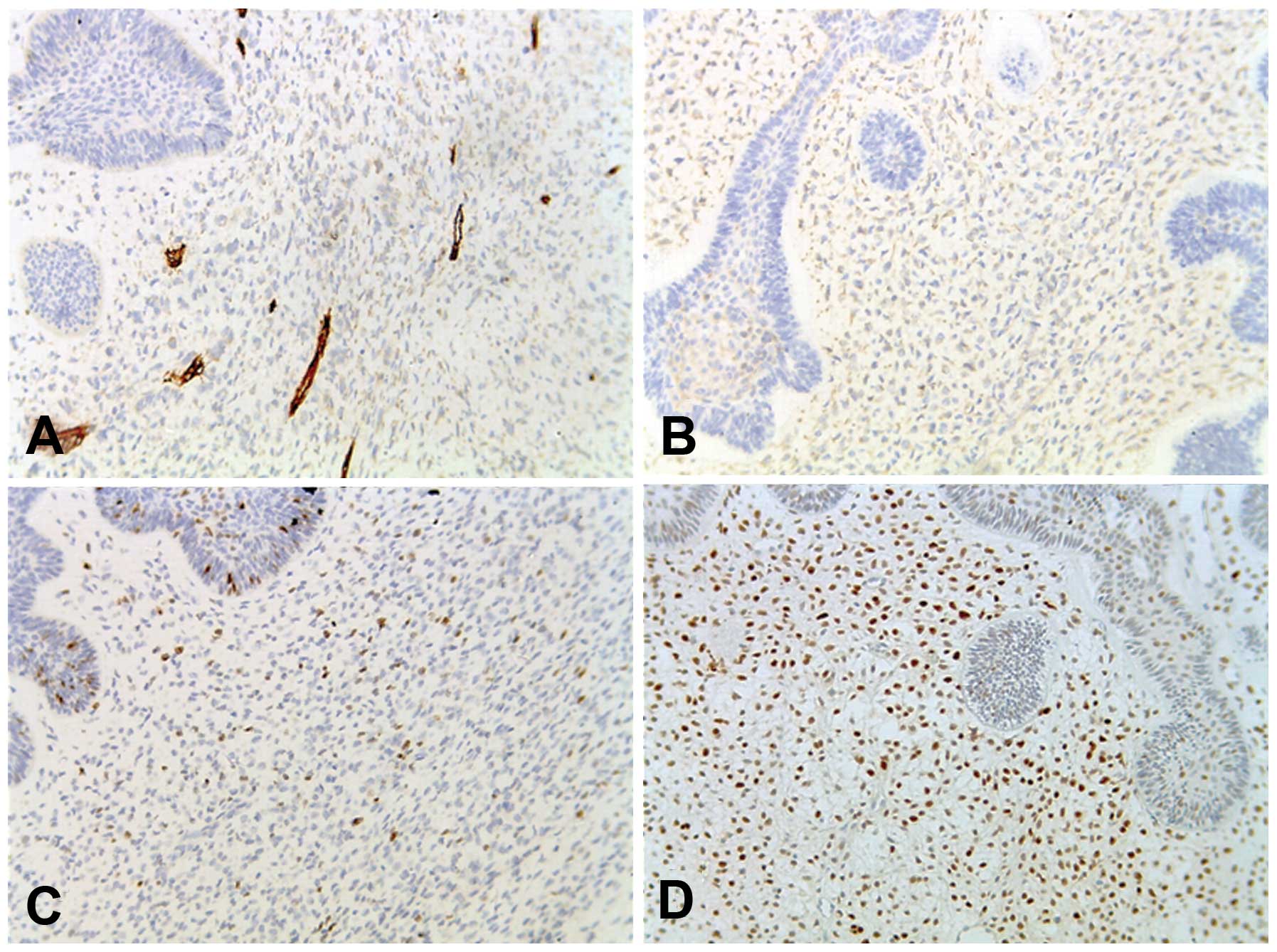
the left mandible. An incisional biopsy was performed and the
pathological diagnosis was consistent with AFS (Fig. 3). Immunohistochemically, the cells
in the sarcomatous areas were positive for cluster of
differentiation (CD) 34, vimentin, p53 protein and Ki-67, with a
labeling index of ~22%, but negative for smooth muscle actin,
S-100, CD68 and desmin (Fig.
4).
The patient underwent a wide left mandibulectomy
including the surrounding soft tissue and destructive bone lesion.
The final histopathological diagnosis was identical to that of the
incisional biopsy. Postoperative radiotherapy with 50 Gy was
implemented after the surgery for five weeks. The patient was under
regular follow-up until 2011 (six years) after the surgery and
showed no signs of recurrence.
Discussion
AFS is a rare malignant neoplasm, consisting of two
components: i) A reductive benign odontogenic epithelium arranged
in an island and net pattern, dispersing in the mesenchymal tissue;
and ii) malignant hypercellular mesenchymal tissue comprised of
spindle and stellate cells, exhibiting nuclear pleomorphism and
hyperchromatism (4,5). In the present case,
immunohistochemical staining showed that the cells were
predominantly positive for p53, Ki-67, CD34 and vimentin but
negative for smooth muscle actin, S-100, CD68 and desmin in the
mesenchymal tissue.
Radiographic examination is important to ascertain
the correct diagnosis. Panoramic radiography can manifest a
macroscopical, effective and low-cost image for the lesions
involving the destructed bones. Furthermore, CT scans can provide
more detailed information about the lesion and the association with
the adjacent organs.
In this case, AFS was believed to show recurrence
potential following conservative treatment. Compared with the
initial lesions, recurrent lesions exhibit decreased epithelial
components and increased pleomorphic and mitotic mesenchymal
components (3,5,6). AFS
is usually characterized by local invasiveness rather than regional
or distant metastasis.
Previously, curettage, nucleation and local excision
have typically been utilized in the surgical procedure (7). Since the proliferative potential and
malignant degree of the mesenchymal component is elevated in the
recurrent neoplasm, the eventual result is sarcomatous
transformation (3,8). In this case, the inadequacy of the
surgical boundary may have induced the recurrence of the tumor.
Therefore, local control is strongly dependent on the extent of the
initial resection, and conservative surgery must be abandoned and
replaced by wide surgical resection with the surrounding soft
tissue, particularly when the cortical plates have been perforated.
Adjuvant postoperative radiotherapy and chemotherapy remain
disputed. A number of cases involving chemotherapeutic medicines,
such as cyclophosphamide and fluorouracil, have exhibited a
positive result (9). Furthermore,
the administration of radiotherapy (40–60 Gy) following surgery can
produce effective results (4,10,11).
In conclusion, AFS is a rare malignant odontogenic
tumor. It is difficult to discriminate AFS from AF when relying
only on the histopathological results and clinical features.
Resection with a wide margin is the optimal treatment strategy, and
adjuvant chemotherapy and radiotherapy may additionally be used to
reduce the recurrence rate and enhance the quality of life.
References
|
1
|
Heath C: Lectures on certain disease of
the jaws. Br Med J. 2:5–13. 1887. View Article : Google Scholar
|
|
2
|
Dallera P, Bertoni F, Marchetti C,
Bacchini P and Campobassi A: Ameloblastic fibrosarcoma of the jaw:
report of five cases. J Craniomaxillofac Surg. 22:349–354. 1994.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kobayashi K, Murakami R, Fujii T and
Hirano A: Malignant transformation of ameloblastic fibroma to
ameloblastic fibrosarcoma: case report and review of the
literature. J Craniomaxillofac Surg. 33:352–355. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Zabolinejad N, Hiradfar M, Anvari K and
Razavi AS: Ameloblastic fibrosarcoma of the maxillary sinus in an
infant: a case report with long-term follow-up. J Pediatr Surg.
43:e5–e8. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Bregni RC, Taylor AM and García AM:
Ameloblastic fibrosarcoma of the mandible: report of two cases and
review of the literature. J Oral Pathol Med. 30:316–320. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kousar A, Hosein MM, Ahmed Z and Minhas K:
Rapid sarcomatous transformation of an ameloblastic fibroma of the
mandible: case report and literature review. Oral Surg Oral Med
Oral Pathol Oral Radiol Endod. 108:e80–e85. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Muller S, Parker DC, Kapadia SB, et al:
Ameloblastic fibrosarcoma of the jaws. A clinicopathologic and DNA
analysis of five cases and review of the literature with discussion
of its relationship to ameloblastic fibroma. Oral Surg Oral Med
Oral Pathol Oral Radiol Endod. 79:469–477. 1995.PubMed/NCBI
|
|
8
|
Chen Y, Wang JM and Li TJ: Ameloblastic
fibroma: a review of published studies with special reference to
its nature and biological behavior. Oral Oncol. 43:960–969. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Goldstein G, Parker FP and Hugh GS:
Ameloblastic sarcoma: pathogenesis and treatment with chemotherapy.
Cancer. 37:1673–1678. 1976. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
de Nogueira TO, Carvalho YR, Rosa LE and
Dos Santos LM: Possible malignant transformation of an ameloblastic
fibroma to ameloblastic fibrosarcoma: a case report. J Oral
Maxillofac Surg. 55:180–182. 1997.PubMed/NCBI
|
|
11
|
Demoor-Goldschmidt C, Minard-Colin V,
Cassagneau E, et al: Ameloblastic fibrosarcoma of the mandible:
report of 2 chemosensitive pediatric cases. J Pediatr Hematol
Oncol. 34:e72–e76. 2012. View Article : Google Scholar : PubMed/NCBI
|