Introduction
Intracranial germ cell tumors are classified into
two fundamental types: Germinomas and nongerminomatous germ cell
tumors. Yolk sac tumor (YST), also known as endodermal sinus tumor,
is a nongerminomatous germ cell tumor (1,2).
Twelve percent of nongerminomatous germ cell tumors are mixed germ
cell tumors with YST elements, and 2% are pure YSTs (3). Intracranial YST usually occurs in
childhood or adolescence and is located in the pineal gland,
suprasellar and posterior third ventricular region, and rarely in
other locations (4). The present
study describes a rare case of pure YST in the anterior third
ventricle that infiltrated into the lateral ventricle in a
middle-aged patient.
Case report
A 45-year-old female patient was admitted to the
Second Hospital of Shandong University (Jinan, China) on October
31, 2012. The patient presented with symptoms of polydipsia and
polyuria for 19 years, menopause for two years, headache for nine
days, gait disturbance and deteriorated mental state, but with no
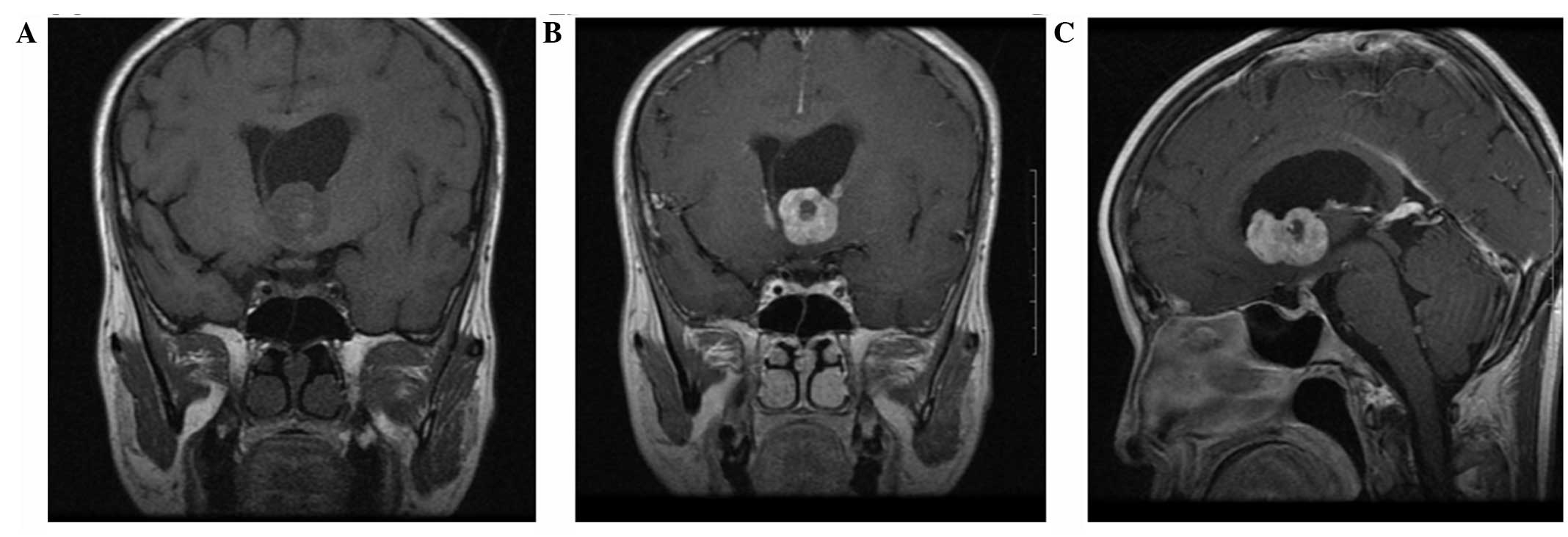
evidence of visual field defects or papilledema. Brain magnetic
resonance imaging (MRI) performed on November 1, 2012 demonstrated
the presence of a mass in the anterior third ventricle with
dimensions of 3.2×2.4×2.3 cm, appearing with low intensity on
T1-weighted images, and hyperintensity on T2-weighted images.
Strong gadolinium enhancement was present with the exception of at
the hemorrhagic center. The tumor had spread to the left section of
the lateral ventricles, and the third and lateral ventricles were
dilated (Fig. 1). The neuroimaging
diagnosis was of craniopharyngioma.
On November 12, 2012, the tumor was excised using a
transfrontal approach from the anterior section of the third
ventricle. The tumor was located in the anterior third ventricle,
blocking the interventricular foramen, and partially invaded the
lateral ventricle through the interventricular foramen.
Immunohistochemical staining of α-fetoprotein (AFP) showed strong
cytoplasmic staining. The histological diagnosis was of
intracranial pure YST. Subsequently, the patient received
whole-brain radiotherapy (30–36 Gy) and focal radiotherapy (45 Gy).
All the procedures carried out in the present study were approved
by the ethics committee of Shandong University (Jinan, China) and
written and informed consent was obtained from the patient prior to
participation. During the 12 months of follow-up, the majority of
the symptoms disappeared with the exception of headache. MRI
revealed chronic hemorrhage but no residual tumor.
Discussion
Since radiological manifestations can be
nonspecific, the preoperative diagnosis of a pure YST is
challenging. In the present case, the mass was irregular and
located in the anterior third ventricle, appearing as an area of
low intensity on T1-weighted images and an area of hyperintensity
on T2-weighted images. Strong gadolinium enhancement was present
with the exception of at the hemorrhagic center. The preoperative
diagnosis in the present case was of craniopharyngioma. Hemorrhage
is not a characteristic radiological feature of craniopharyngioma
(5). The differential diagnosis of
YST in the anterior third ventricle includes craniopharyngiomas,
germ cell tumors, gliomas, pituitary macroadenomas and meningiomas.
Among these, germinomas are the most difficult to distinguish from
YSTs. MRI and advanced MR techniques are useful in distinguishing
between germinomas and YSTs. The solid components of germinomas may
show homogeneous or heterogeneous enhancement, while YSTs show
heterogeneous enhancement with hemorrhage and necrosis (6,7).
Diffusion-weighted imaging (DWI) is reportedly helpful in
differentiating germinoma germ cell tumors from YSTs. YSTs show
facilitated diffusion with a high apparent diffusion coefficient
value (8). The value of DWI and
other functional MRI studies in the diagnosis of YSTs requires
further study. Since there are no specific imaging features of
YSTs, serum or cerebrospinal fluid markers are necessary for
diagnosis. An increased serum AFP level may indicate the presence
of a YST. The AFP level was significantly increased in the present
case.
According to the classification of intracranial germ
cell tumors described by Matsutani et al (3), YST belong to the poor prognosis
group, for which a combination of surgical resection, chemotherapy
and radiotherapy is recommended (9). In the present case, the patient
received radiotherapy alone. One year after the surgery, no tumor
recurrence was observed. However, the long-term effect remains
uncertain and requires further investigation.
In conclusion, to the best of our knowledge, the
present case is the first report of a pure YST in the anterior
third ventricle of a middle-aged patient. Although the definitive
diagnosis of intracranial YST depends on the pathologic examination
(10), MRI may aid the
differential diagnosis. When heterogeneous enhancement and an
irregular mass with surrounding invasion and ventricular dilation
are observed in the anterior third ventricle of an adult,
clinicians should consider the possibility of a YST. A combination
of surgical resection and radiotherapy is recommended.
Acknowledgements
This study was supported by the Second Hospital and
the Provincial Hospital of Shandong University (Jinan, China).
References
|
1
|
Rousseau A, Mokhtari K and Duyckaerts C:
The 2007 WHO classification of tumors of the central nervous system
- what has changed? Curr Opin Neurol. 21:720–727. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Packer RJ, Cohen BH and Cooney K:
Intracranial germ cell tumors. Oncologist. 5:312–320. 2000.
|
|
3
|
Matsutani M, Sano K, Takakura K, et al:
Primary intracranial germ cell tumors: a clinical analysis of 153
histologically verified cases. J Neurosurg. 86:446–455. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Allen JC, Nisselbaum J, Epstein F, Rosen G
and Schwartz MK: Alphafetoprotein and human chorionic gonadotropin
determination in cerebrospinal fluid. An aid to the diagnosis and
management of intracranial germ cell tumors. J Neurosurg.
51:368–374. 1979. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Nada R, Mohan H, Dhir SP, Mukherjee KK and
Kak VK: Suprasellar malignant mixed germ cell tumour presenting as
craniopharyngioma. Neurol India. 48:381–384. 2000.PubMed/NCBI
|
|
6
|
Wang Y, Zou L and Gao B: Intracranial
germinoma: clinical and MRI findings in 56 patients. Childs Nerv
Syst. 26:1773–1777. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Liang L, Korogi Y, Sugahara T, et al: MRI
of intracranial germ-cell tumours. Neuroradiology. 44:382–388.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Macvanski M, Ristić-Balos D, Vasić B, et
al: Intracranial yolk sac tumor in an adult patient: MRI,
diffusion-weighted imaging and 1H MR spectroscopy
features. Vojnosanit Pregl. 69:277–280. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Gaoyu C, Deyu G, Zhi C and Hua F: Yolk sac
tumor in the fourth ventricle: a case report. Clin Neurol
Neurosurg. 111:636–637. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Sato K, Takeuchi H and Kubota T: Pathology
of intracranial germ cell tumors. Prog Neurol Surg. 23:59–75. 2009.
View Article : Google Scholar
|