Introduction
A previous epidemiological study has shown that
acute lung injury (ALI) is common in clinical critical diseases.
Despite competent supportive therapy and care having been used, the
mortality rate of ALI remains high and the effectiveness remains
unsatisfactory (1). ALI and its
severe form, multiple organ dysfunction syndrome (MODS), remain a
major public health problem. Therefore, understanding the
pathogenesis of ALI/MODS and the search for novel methods to treat
ALI/MODS has become currently urgent. This study focuses on the
efficacy and the mechanisms of Xuebijing injection in the treatment
of ALI/MODS.
An early characteristic of ALI is the activation and
recruitment of neutrophils in the lungs and the inflammatory effect
induced by neutrophils (2).
Myeloperoxidase (MPO) is a neutrophil-specific reductase, the
intracellular content of which is stable, and the number of
activated neutrophils may be indirectly reflected by the MPO
activity of unit lung tissue (3).
Previous studies (4–6) have
shown that a variety of cytokines play key roles in the progression
of ALI. Cytokines (7) that are
synthesized and secreted by certain immune and non-immune cells are
a type of small molecule protein with broad biological activities
that are mainly involved in regulating immune response, mediating
inflammation and stimulating hematopoietic function and tissue
repair. Cytokines can be divided into pro- and anti-inflammatory
cytokines according to their different roles in inflammatory
reactions (8–10). Interleukin (IL)-6 is a potent
proinflammatory cytokine, which has a crucial effect on the
initiation of inflammation (11)
and plays an important role in processes including host defense,
acute phase response, immune response and blood reactions (12–14).
Moreover, anti-inflammatory cytokines including IL-4 (15), IL-10 (16,17)
and transforming growth factor-β (TGF-β) (18), are also found to be at a relatively
high level in ALI.
Xuebijing injection is a herbal medicine consisting
of Flos Carthami, Salvia miltiorrhiza, Radix Paeoniae Rubra,
Chinese Angelica and Ligusticum chuanxiong Hort. In China,
Xuebijing injection is widely used for treating acute and severe
diseases including systemic inflammatory response syndrome (SIRS)
and MODS (19). A previous study
confirmed that the effectiveness of Xuebijing injection is
associated with regulation of the expression of inflammatory
cytokines at the serum level (20); however, there are limited studies
concerning the regulatory effect of Xuebijing injection on the
expression levels of inflammatory cytokines at the protein and mRNA
levels. Thus, the current study further explored the possible
mechanisms of the effect of Xuebijing injection on ALI at the
protein and mRNA levels.
Materials and methods
Laboratory animals
Sixty healthy adult mixed gender New Zealand rabbits
weighing 250–350 g were obtained from the Experimental Animal
Center of Zhengzhou University (Zhengzhou, China) and used for all
the experiments. They were randomly divided into three groups: the
normal control group (CG; n=20), oleic acid group (model group, MG;
n=20), and oleic acid + Xuebijing injection group (treatment group,
TG; n=20). All rabbits were housed in separate cages under suitable
temperature and humidity and had free access to water and food
prior to the study. All experimental procedures were approved by
the Ethics Committee of Xinxiang Medical University (Xinxiang,
China). The study was performed according to the principles
enunciated in the ethical principles of the Declaration of
Helsinki.
Main reagents and instruments
The main instruments used in this study include the
Leica RM2235 microtome (Leica Biosystems GmbH, Nussloch, Germany),
Labnet polymerase chain reaction (PCR) instrument (Shenzhen Cy-tech
Biotechnology Co., Ltd., Shenzen, China), DG5033A enzyme-linked
immunosorbent assay (ELISA) Analyzer (Nanjing Huadong Electronics
Group Medical Equipment Co., Ltd., Nanjing, China) and the fully
automatic M248 blood gas analyzer (Bayer China Ltd., Shanghai,
China). The main reagents used include oleic acid (purity ≥99.0%,
Sigma-Aldrich, St. Louis, MO, USA), Xuebijing injection (10
ml/vial, Tianjin Chase Sun Pharmaceutical Co., Ltd., Tianjin,
China), 20% urethane (Shanghai Yunqiang Chemical Co., Ltd.,
Shanghai, China), IL-6 and IL-10 goat anti-rabbit polyclonal
antibodies (Beijing Boosen Biological Technology Co., Ltd.,
Beijing, China), ELISA kits (Beijing Zhongshan Golden Bridge
Biological Technology Co., Ltd., Beijing, China), MPO kits (Nanjing
Jiancheng Biological Engineering Institute, Nanjing, China),
TRIzol® and reverse transcription (RT)-PCR kit (Baiyi
Xinchen Biotechnology Co., Ltd., Beijing, China).
Surgery
All rabbits received general anesthesia with 20%
urethane (5 ml/kg) via the ear vein; the trachea and common carotid
artery were isolated and intubated. Rabbits of the CG received 0.9%
saline via the ear vein (0.4 ml/kg). For rabbits of the MG, the
rabbit model of ALI was established according to the method of a
previous study (21); rabbits were
administered oleic acid (0.4 ml/kg) from the ear vein (slowly and
uniformly, 0.1 ml/min). Rabbits of the TG received Xuebijing
injection (10 ml/kg) immediately subsequent to injection with oleic
acid by the same method as was used in the MG. When pink foamy
liquid poured from the tracheal intubation of the rabbits of the MG
and was accompanied by evident shallow frequency breathing, the ALI
model of the MG was considered to have succeeded. Arterial blood
(10 ml) was extracted from the common carotid artery of each rabbit
of each group 1 h after injection of the corresponding reagent
(several preliminary experiments found that it took ~1 h to
establish the ALI model). Measurements of the arterial partial
pressure of oxygen (PaO2) and carbon dioxide
(PaCO2) in arterial blood were made using a blood gas
analyzer. Later, all rabbits were sacrificed by air embolism and
the lungs were removed and fixed with paraformaldehyde solution (1
ml/100 g).
Colorimetry
MPO activity provides indirect evidence of
neutrophil infiltration. MPO activity was measured according to the
instructions provided by the manufacturer of the MPO kit; lung
tissues were weighted accurately, 5% homogenate was prepared
(weight by volume: 1:9), without centrifugation, mixed, put in a
60°C water bath for 10 min. Then, at 460 nm with a 1 cm optical
path, and the use of distilled water to zero the colorimeter, the
absorbance value of each tube was measured. Lung MPO activity was
calculated using the following formula: MPO activity (U/g) =
Optical density value of measuring tube - optical density value of
control tube/11.3 × sample size (g)
Immunohistochemistry
To evaluate IL-6 and IL-10 levels, the
formalin-fixed and paraffin-embedded lung tissues were
deparaffinized in xylene and rehydrated using a graded series of
alcohol, quenched with 3% H2O2, blocked with
5% normal goat serum and probed with rat anti-rabbit IL-6/IL-10
antibody. Detection was with biotinylated anti-rat immunoglobulin
G, followed by incubation with avidin-biotin complex and
3,3′-diaminobenzidine (DAB) substrate and hematoxylin
counterstaining. According to the method described in a previous
study (22), the expression levels
of the two proteins were determined semi-quantitatively. Ten
high-power fields were selected and the expression level was
defined as follows: No positive cells, −; 0–25%, +; 25–50%, +;
50–75%, ++; >75%, +++. These experiments were performed in
triplicate.
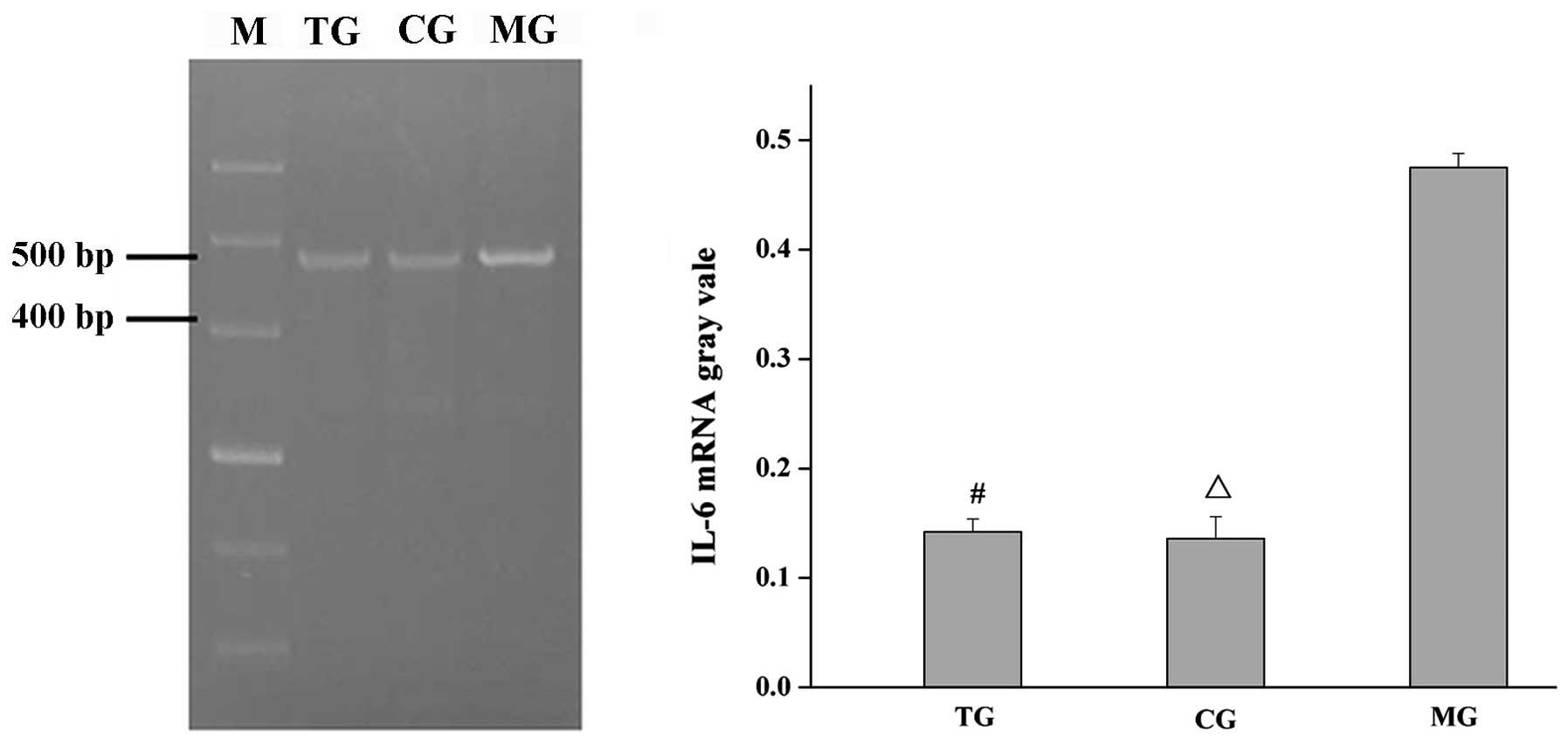
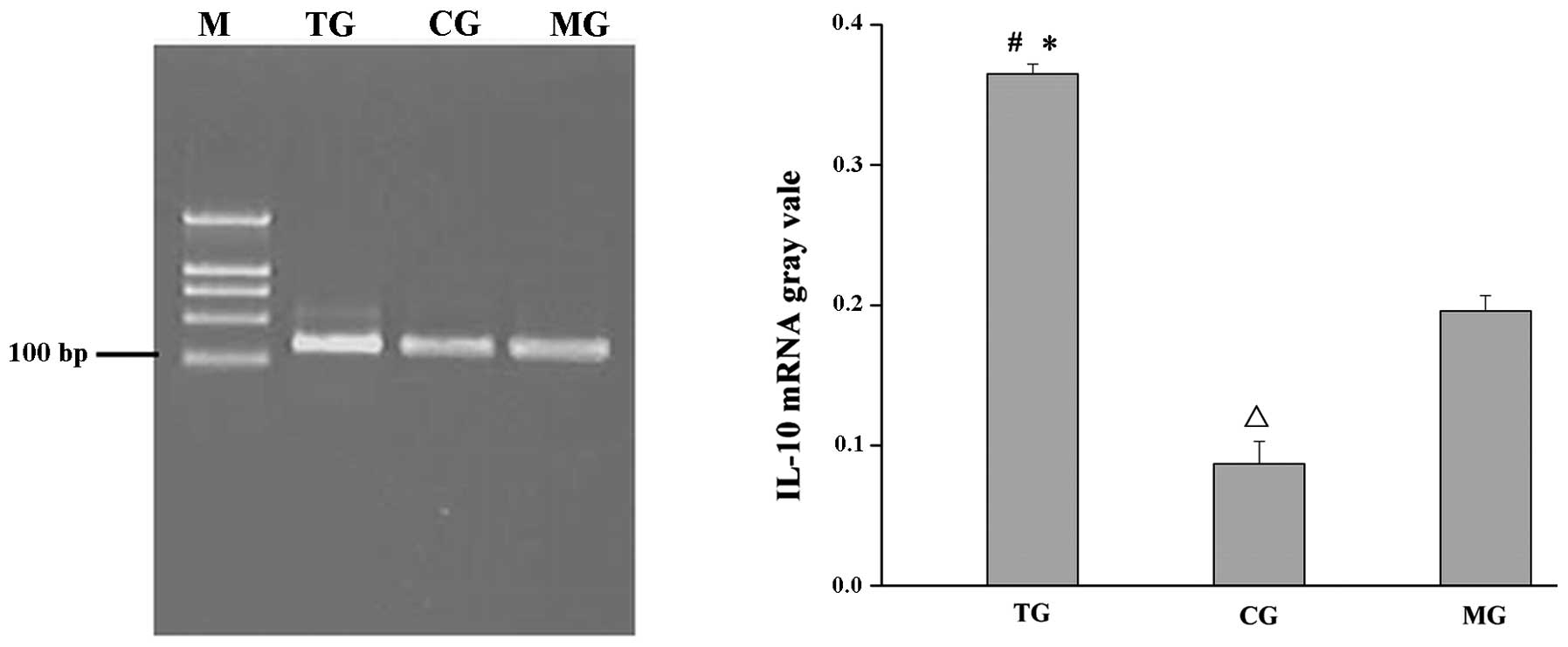
Total RNA extraction and RT-PCR
In order to obtain the relative quantification of
specific gene expression and statistical analysis compared with the
CG, ~100 mg lung tissue was stored at −80°C. Total RNA was
extracted by a one-step method with TRIzol®, and cDNA
was then generated for the RT-PCR analysis, using GAPDH as an
internal reference gene. The following primers (Baiyi Xinchen
Biotechnology Co., Ltd.) were used: GAPDH, forward,
5′-AGTTCAACGGCACAGTCAAGG-3′ and reverse,
5′-AGACTCCACGACATACTCAGC-3′, amplified fragment length 1,622bp;
IL-6, forward, 5′-CTTCCAGCCAGTTGCCTTCT-3′ and reverse, 5′-GAG
AGCATTGGAAGTTGGG-3′, amplified fragment length 496 bp; IL-10,
forward, 5′-CAGACCCACATGCTCCG AGA-3′ and reverse,
5′-CAAGGCTTGGCAACCCAAGTA-3′, amplified fragment length 141 bp. The
gray ratio of the PCR target band and internal reference band was
analyzed using Band Leader 3.0 software (Magnitec Ltd., Tel Aviv,
Israel).
Statistical analysis
Statistical analysis was performed using SPSS
statistical software, version 11.0 (SPSS, Inc., Chicago, IL, USA).
Measurement data are expressed as mean ± standard deviation, and
were tested using the independent samples Student’s t-test. Count
data were analyzed using the χ2 test. Spearman’s rank
correlation analysis was used to analyze the correlation of IL-6
and IL-10 of rabbit lung tissue in the three groups. P<0.05 was
considered to indicate a statistically significant result.
Results
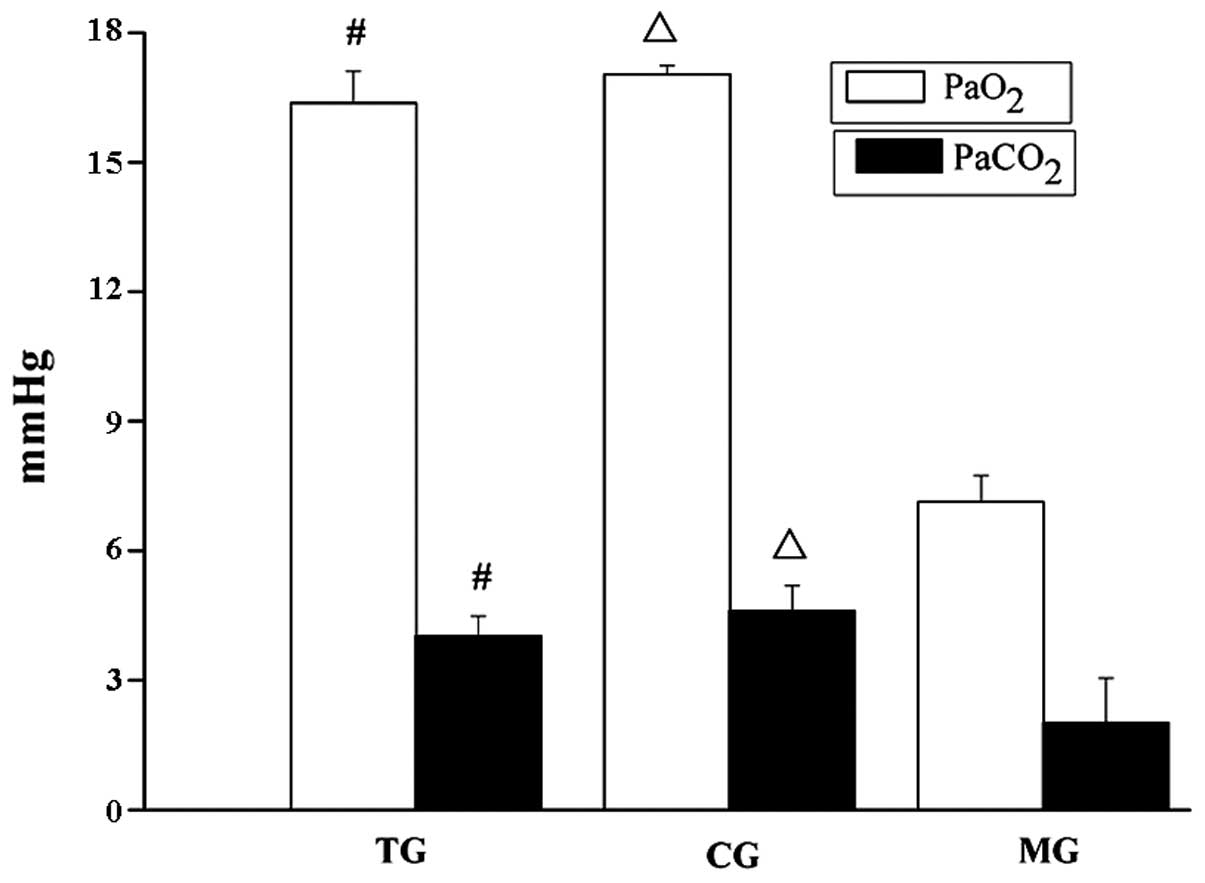
Xuebijing injection improves the
PaO2 and PaCO2 of rabbits with oleic
acid-induced ALI
PaCO2 and PaO2 are used to
evaluate respiratory function. PaO2 reduces with/without
increases in PaCO2 during respiratory dysfunction.
PaCO2 and PaO2 were measured using a blood
gas analyzer. As shown in Fig. 1,
PaO2 and PaCO2 in the TG were higher compared
with that in the MG (P<0.001) and lower compared with those in
the CG (P≥0.05) and PaO2 and PaCO2 in the MG
were lower compared with those in the CG (P<0.001), which
suggests that respiratory function improved when rabbits with ALI
were treated with Xuebijing injection.
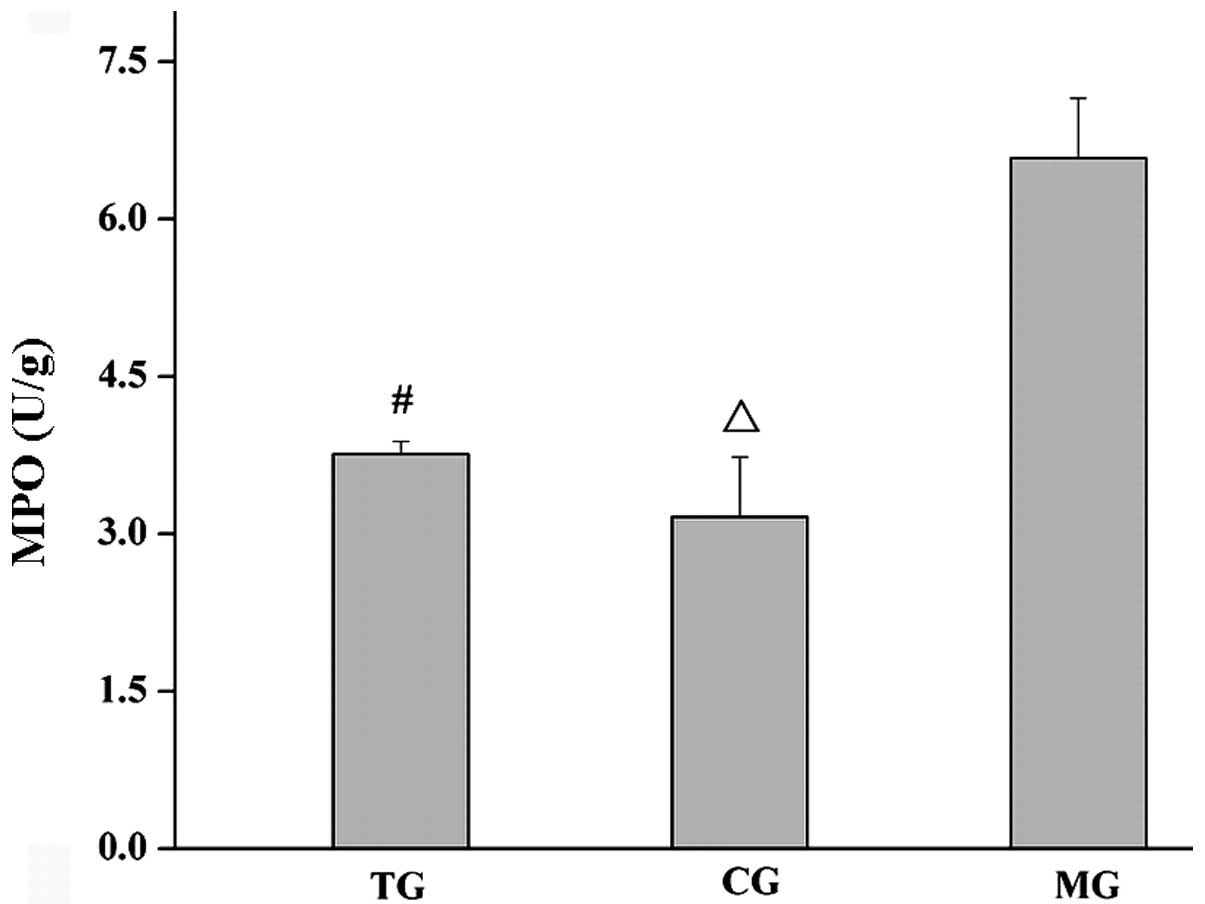
Xuebijing injection decreases MPO
activity in the lung tissue of rabbits with oleic acid-induced
ALI
To elucidate the underlying mechanisms by which
Xuebijing injection promotes respiratory function, the MPO activity
per unit of lung tissue, which is an index of neutrophil
infiltration, was analyzed. It was found that the MPO activity in
the lung tissue of the TG was lower compared with that of the MG
(P<0.001) and higher compared with that of the CG (P≥0.05), and
the MPO activity in the lung tissue of the MG was higher compared
with that of the CG (P<0.001), as shown in Fig. 2.
Xuebijing injection reduces the
expression of IL-6 and increased the expression of IL-10 at the
protein and mRNA levels in the lung tissue of rabbits with oleic
acid-induced ALI
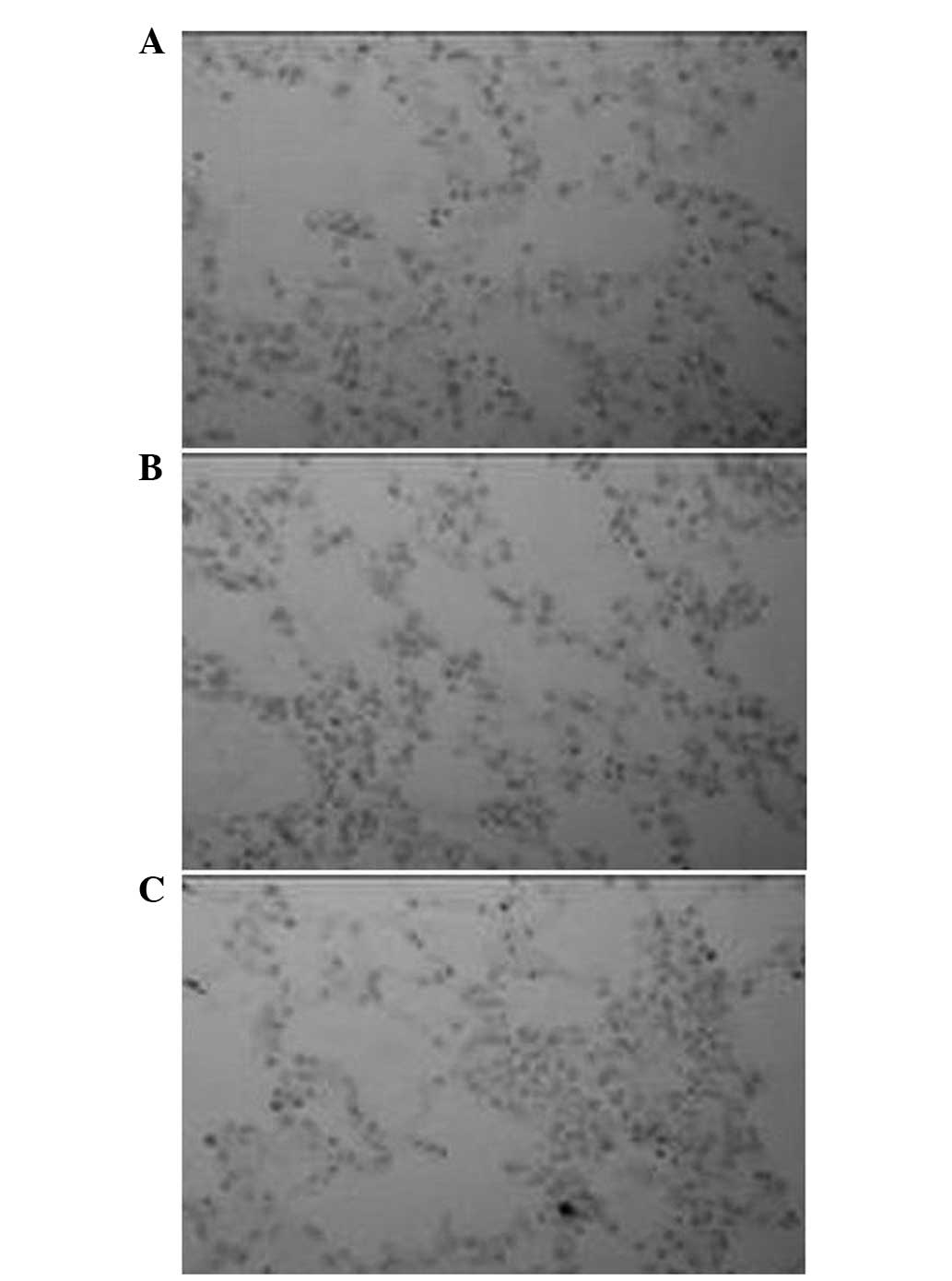
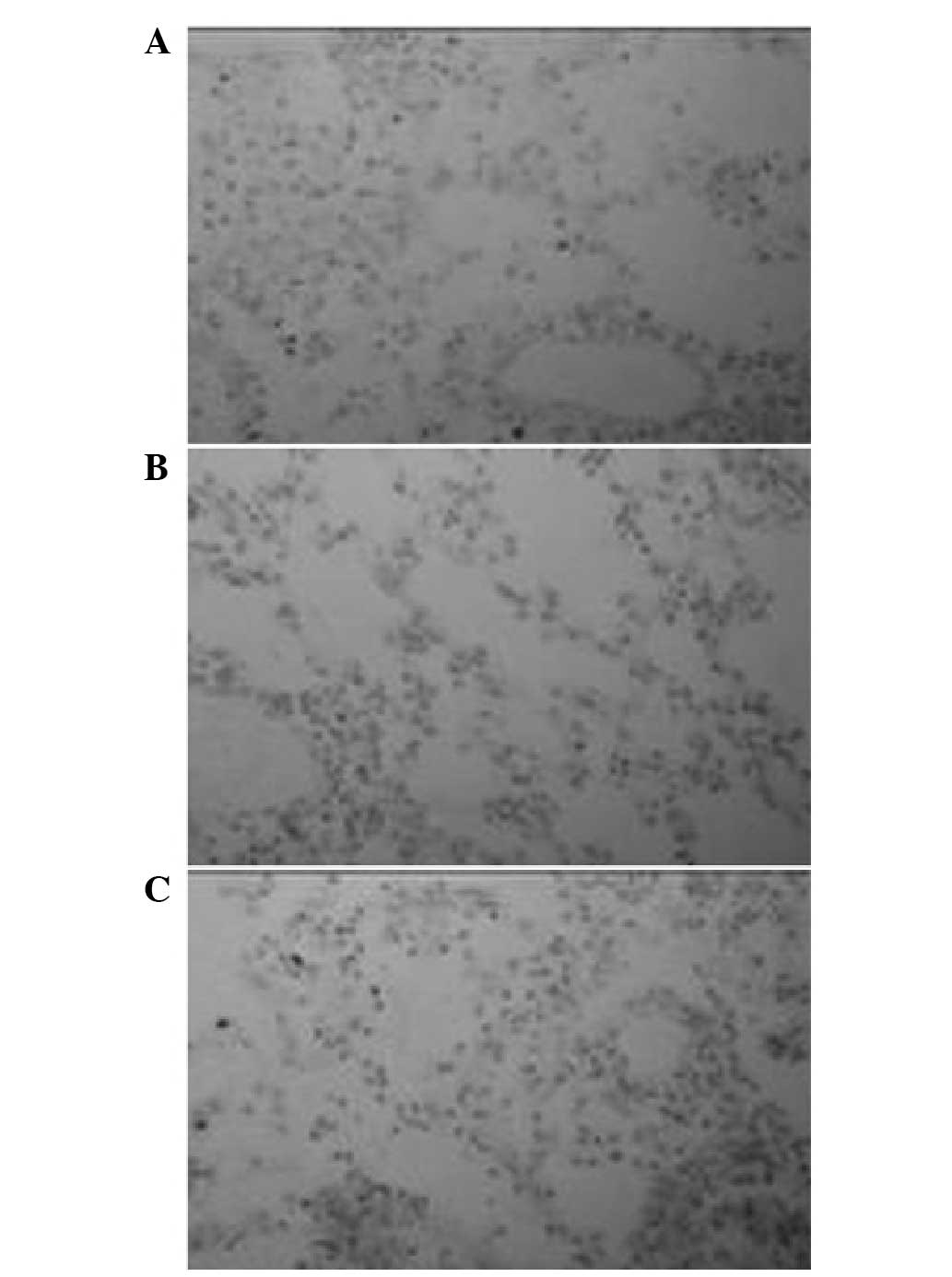
The immune response products comprising the
proinflammatory cytokine IL-6 and the anti-inflammatory cytokine
IL-10, which are mainly located in the cytoplasm were examined by
immunohistochemistry. Positively immunoreactive products with DAB
staining were observed as brown-yellow granules. Examples of
staining in each of the groups are shown in Figs. 3 and 4. By the χ2 test, the
expression level of IL-6 protein in the TG was lower than that in
the MG (P<0.05) and higher than that in the CG (P≥0.05), and the
expression levels of the proinflammatory cytokine IL-6 and
anti-inflammatory cytokine IL-10 in the TG were higher than those
in the MG (P<0.05) and CG (P≥0.05), as shown in Tables I and II.
 | Table IComparison of the protein expression
of interleukin 6 in the lung tissue of the rabbits in the three
groups (n=20). |
Table I
Comparison of the protein expression
of interleukin 6 in the lung tissue of the rabbits in the three
groups (n=20).
| Interleukin 6 |
|---|
|
|
|---|
| Group | − | + | ++ | +++ | P-value |
|---|
| TG | 8 | 8 | 3 | 1 | <0.05a |
| MG | 2 | 4 | 9 | 5 | <0.05b |
| CG | 7 | 9 | 4 | 0 | ≥0.05c |
 | Table IIComparison of the protein expression
of interleukin 10 in the lung tissue of rabbits in the three groups
(n=20). |
Table II
Comparison of the protein expression
of interleukin 10 in the lung tissue of rabbits in the three groups
(n=20).
| Interleukin 6 |
|---|
|
|
|---|
| Group | − | + | ++ | +++ | P-value |
|---|
| TG | 0 | 4 | 7 | 9 | <0.05a |
| MG | 1 | 2 | 6 | 11 | <0.05b |
| CG | 9 | 5 | 4 | 2 | ≥0.05c |
RT-PCR was used to further clarify the effect of
Xuebijing injection on IL-6 and IL-10 protein expression levels in
the lung tissue of rabbits with ALI induced by oleic acid. The
results of the RT-PCR were highly consistent with the results of
the immunohistochemistry, as shown in Figs. 5 and 6. Subsequent to the administration of the
Xuebijing injection, the expression level of IL-6 mRNA clearly
decreased, while the expression level of IL-10 MRNA further
increased.
Discussion
The objective of this study was to investigate the
possible mechanisms by which Xuebijing injection exerts its effects
in the treatment of ALI. The results showed that the improvement of
respiratory function in ALI by Xuebijing injection may be
associated with the inhibition of the mRNA and protein expression
of the proinflammatory cytokine IL-6, and the enhancement of the
mRNA and protein expression of the anti-inflammatory cytokine
IL-10.
First, a classic model of ALI induced by oleic acid
was established, and the pathophysiological changes and the
response process of the oleic acid-induced ALI were close to
clinical. The key to replicating the model of ALI was to accurately
inject a specific amount of oleic acid. Oleic acid was injected
into the ear vein of rabbits slowly and uniformly (0.1 ml/per min).
The method was simple, with low trauma and the effect was
significant. One hour subsequent to oleic acid being injected into
the rabbits, the breathing of the rabbits significantly quickened,
cyanosis of the lips was observed, inspiratory and expiratory
crackles were clearly audible in the anterior right lung field, and
the most typical phenomenon was that pink foamy liquid poured from
the intubation.
Secondly, PaO2 and PaCO2,
which are used to evaluate respiratory function, were measured.
Blood gas analysis showed that the PaO2 and
PaCO2 of rabbits in the MG were lower than those in the
CG (Fig. 1), and the difference
was statistically significant. This suggested that oleic acid
impaired the lung and its effects were similar to the clinical
changes associated with ALI, including progressive dyspnea and
hypoxemia that are difficult to correct. The PaO2 and
PaCO2 of rabbits in the TG were higher than those in the
MG (Fig. 1), and were lower than
those in the CG, although not statistically significantly, which
implied that Xuebijing injection alleviated lung injury and improve
respiratory function.
Thirdly, MPO activity, a marker of neutrophil
activation, was detected. Activation and migration of neutrophils
are regarded key events in the progression of ALI. Neutrophils are
the first cells to be recruited to the sites of injury or infection
(23,24) once an inflammatory response is
initiated. An appropriate amount of neutrophils has a potent
antimicrobial effect; however, an excessive amount of neutrophils
can damage host tissues. MPO activity is used to quantify the
amount of neutrophil infiltration. The present study demonstrated
that MPO activity in the MG was higher than that in the TG and CG,
and the differences were statistically significant (Fig. 2), which identified that numerous
neutrophils were activated by oleic acid in the pulmonary
circulation of the MG rabbits, and activated neutrophils led to ALI
and respiratory dysfunction (decreased PaO2 and
PaCO2; Fig. 1).
Xuebijing injection effectively reduced the number of activated
neutrophils (decreased MPO activity; Fig. 2), and the respiratory function
improved (increased PaO2 and PaCO2; Fig. 1).
Fourthly, the protein and mRNA expression levels of
the proinflammatory cytokine IL-6 and the anti-inflammatory
cytokine IL-10 in the lung tissue were detected by
immunohistochemistry and the RT-PCR technique. The results
demonstrated that the protein and mRNA expression levels of IL-6
and IL-10 in the lung tissue of the MG were increased. Oleic acid
exerted an effect on the body; inflammatory cells and immune cells
were in a highly activated state, large quantities of IL-6 and
IL-10 were released into the blood, the rabbits showed rapid
shallow breathing, the PaCO2 decreased, the number of
activated white blood cells increased (increased MPO activity) and
other typical clinical signs of ALI were observed. However,
Xuebijing injection is able to regulate the expression of
inflammatory cytokines (25–27).
Xuebijing injection reduced the number of neutrophils (reduced MPO
activity; Fig. 2), reduced the
expression of the proinflammatory cytokine IL-6 (Figs. 3 and 5, Table
I), and increased the expression of the anti-inflammatory
cytokine IL-10 (Figs. 4 and
6, Table II) at the mRNA and protein levels.
The inflammation was localized.
In the oleic-induced pathogenesis of ALI, oleic
acid, a harmful factor, invaded the pulmonary circulation and
neutrophils were activated. Activated neutrophils underwent
chemotaxis, aggregation and release reaction, and the
proinflammatory cytokine IL-6 was over-secreted, which resulted in
imbalanced metabolic pathways and tissue damage. To prevent severe
damage, the anti-inflammatory cytokine IL-10 was released and an
vigorous, uncontrolled inflammatory response occurred, which led to
lung tissue damage and function injury. Xuebijing injection
effectively reduced neutrophil adhesion, aggregation and release
reaction (MPO activity weakened), reduced the levels of the
proinflammatory cytokine IL-6 and increased the levels of the
anti-inflammatory cytokine IL-10. Thus, inflammation was
effectively controlled and respiratory function improved.
Acknowledgements
This study was supported by grants from the
Foundation of Henan Educational Commission (no. 2011GGJS-127),
Henan Science and Technology Bureau to Mingli Ji (no. 132300410160)
and Henan Natural Science to Yuxia Wang (no. 12B310017).
Abbreviations:
|
IL-6
|
interleukin 6
|
|
IL-10
|
interleukin 10
|
|
TG
|
treatment group
|
|
MG
|
model group
|
|
CG
|
control group
|
|
MODS
|
multiple organ dysfunction
syndrome
|
|
PaO2
|
arterial partial pressure of
oxygen
|
|
PaCO2
|
arterial partial pressure of carbon
dioxide
|
|
MPO
|
myeloperoxidase
|
|
ALI
|
acute lung injury
|
|
TGF-β
|
transforming growth factor-β
|
|
SIRS
|
systemic inflammatory response
syndrome
|
|
ELISA
|
enzyme-linked immunosorbent assay
|
|
RT-PCR
|
reverse transcription-polymerase chain
reaction
|
|
DAB
|
3,3′-diaminobenzidine
|
References
|
1
|
Liu W and Jin FG: New progress of acute
lung injury and acute respiratory distress syndrome. Chin J Lung
Dis (Electronic Edition). 1:61–64. 2013.(In Chinese).
|
|
2
|
Chang HM, Ji ML, Song XR, et al: Effect of
inflammatory cell adhesion molecules-1 on acute lung injury in
infant rats following meconium aspiration. Shi Yong Er Ke Lin
Chuang Za Zhi. 27:1835–1836. 2012.(In Chinese).
|
|
3
|
Saraiva M and O’Garra A: The regulation of
IL-10 production by immune cells. Nat Rev Immunol. 10:170–181.
2010. View
Article : Google Scholar : PubMed/NCBI
|
|
4
|
Rittirsch D, Flierl MA and Ward PA:
Harmful molecular mechanisms in sepsis. Nat Rev Immunol. 8:776–787.
2008. View
Article : Google Scholar : PubMed/NCBI
|
|
5
|
Porter JC and Hall A: Epithelial ICAM-1
and ICAM-2 regulate the egression of human T cells across the
bronchial epithelium. FASEB J. 23:492–502. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Grommes J and Soehnlein O: Contribution of
neutrophils to acute lung injury. Mol Med. 17:293–307. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Orlikowsky T, Wang ZQ, Dudhane A, et al:
Two distinct pathways of human macrophage differentiation are
mediated by interferon-gamma and interleukin-10. Immunology.
91:104–108. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kylänpää L, Rakonczay Z Jr and O’Reilly
DA: The clinical course of acute pancreatitis and the inflammatory
mediators that drive it. Int J Inflam. 2012:3606852012.PubMed/NCBI
|
|
9
|
Favarin DC, de Oliveira JR, de Oliveira CJ
and de Rogerio AP: Potential effects of medicinal plants and
secondary metabolites on acute lung injury. Biomed Res Int.
2013:5764792013.PubMed/NCBI
|
|
10
|
Welty-Wolf KE, Carraway MS, Ortel TL and
Piantadosi CA: Coagulation and inflammation in acute lung injury.
Thromb Haemost. 88:17–25. 2002.PubMed/NCBI
|
|
11
|
Tanaka T and Kishimoto T: Targeting
interleukin-6: all the way to treat autoimmune and inflammatory
diseases. Int J Biol Sci. 8:1227–1236. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Frisdal E, Lesnik P, Olivier M, et al:
Interleukin-6 protects human macrophages from cellular cholesterol
accumulation and attenuates the proinflammatory response. J Biol
Chem. 286:30926–30936. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Steiner MK, Syrkina OL, Kolliputi N, et
al: Interleukin-6 overexpression induces pulmonary hypertension.
Circ Res. 104:236–244. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Pedroza M, Schneider DJ, Karmouty-Quintana
H, et al: Interleukin-6 contributes to inflammation and remodeling
in a model of adenosine mediated lung injury. PLoS One.
6:e226672011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Seki T, Kumagai T, Kwansa-Bentum B, et al:
Interleukin-4 (IL-4) and IL-13 suppress excessive neutrophil
infiltration and hepatocyte damage during acute murine
schistosomiasis japonica. Infect Immun. 80:159–168. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hedrich CM and Bream JH: Cell
type-specific regulation of IL-10 expression in inflammation and
disease. Immunol Res. 47:185–206. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
D’Alessio FR, Tsushima K, Aggarwal NR, et
al: CD4+CD25+Foxp3+ Tregs resolve
experimental lung injury in mice and are present in humans with
acute lung injury. J Clin Invest. 119:2898–2913. 2009.
|
|
18
|
Poe SL, Arora M, Oriss TB, et al:
STAT1-regulated lung MDSC-like cells produce IL-10 and efferocytose
apoptotic neutrophils with relevance in resolution of bacterial
pneumonia. Mucosal Immunol. 6:189–199. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Jiang M, Zhou M, Han Y, et al:
Identification of NF-κB inhibitors in Xuebijing injection for
sepsis treatment based on bioactivity-integrated UPLC-Q/TOF. J
Ethnopharmacol. 147:426–433. 2013.
|
|
20
|
He XD, Wang Y, Wu Q, et al: Xuebijing
protects rats from sepsis challenged with Acinetobacter
baumannii by promoting annexin A1 expression and inhibiting
proinflammatory cytokines secretion. Evid Based Complement Alternat
Med. 2013:8049402013.PubMed/NCBI
|
|
21
|
Song XR: Regulation of breathing exercises
and experimental acute respiratory failure. Medical Function
Experiment. Chang QZ: 2nd edition. People’s Medical Publishing
House; Beijing: pp. 124–125. 2007
|
|
22
|
Yu P, Bu H, Wang H, et al: Comparative
study on image analysis and manual counting of
immunohistochemistry. Sheng Wu Yi Xue Gong Cheng Xue Za Zhi.
20:288–290. 2003.(In Chinese).
|
|
23
|
Jiang H, Meng F, Li W, et al: Splenectomy
ameliorates acute multiple organ damage induced by liver warm
ischemia reperfusion in rats. Surgery. 141:32–40. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Smith JA: Neutrophils, host defense, and
inflammation: a double-edged sword. J Leukoc Biol. 56:672–686.
1994.PubMed/NCBI
|
|
25
|
Li YP, Qiao YJ, Wu ZX, et al: Effects of
Xuebijing injection on protein C and tumor necrosis factor-alpha
mRNA in rats with sepsis. Zhongguo Wei Zhong Bing Ji Jiu Yi Xue.
19:488–491. 2007.(In Chinese).
|
|
26
|
Qi F, Liang ZX, She DY, et al: A clinical
study on the effects and mechanism of xuebijing injection in severe
pneumonia patients. J Tradit Chin Med. 31:46–49. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Zhang P, Cao SH, Cui KL, et al: The
influences of Xuebijing on the expression of human leukocyte
antigen-DR on monocytes in patients with multiple organ dysfunction
syndrome. Zhong Guo Zhong Xi Yi Jie He Za Zhi. 9:21–23. 2002.(In
Chinese).
|