Introduction
Pneumothorax is not a rare complication of lung
fibrosis due to progressive systemic sclerosis (PSS); however, a
number of patients with PSS who have extensive pulmonary fibrosis
with enlarged sub-pleural blebs and honeycomb lungs have been shown
to develop pneumothorax. Various treatment options have been
described (1). Surgery is a
treatment option for recurrent and refractory pneumothorax.
Chemical pleurodesis with talc or minocycline is also another
treatment option, but there were complication with deterioration of
pulmonary fibrosis especially in patients with pulmonary fibrosis.
However, the success rate of the of PSS patients with pneumothorax
appeared to be unsatisfactory. A case is reported here following
successful treatment with a blood patch introduced into the chest
via an intercostal chest drain. The purpose of this case report is
to report the usefulness of this successful treatment.
Case report
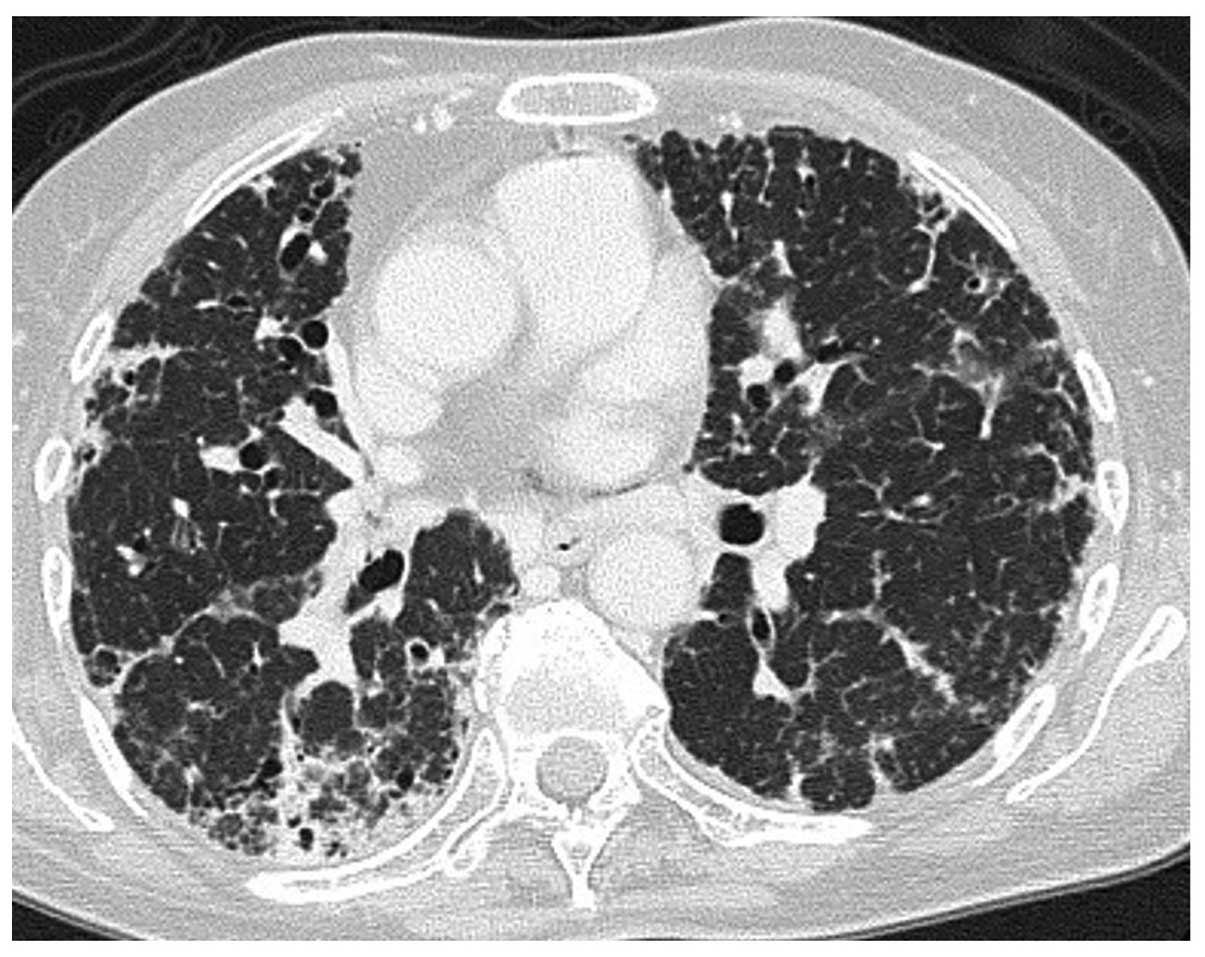
A 69-year-old female was admitted to the Mito
Medical Center (Mito, Japan) due to dyspnea on exertion and right
chest pain lasting all day. Three years previously she was
diagnosed as having PSS with lung fibrosis (Fig. 1). Since then, the patient had
experienced a pneumothorax on the right side several times and had
subsequently received a video-assisted thoracoscopic surgery for
persistent pneumothorax.
Physical examination on admission revealed decreased
respiratory sound in the right lung and diffuse fine crackles in
both lungs. Skin thickening and tightness were observed on the
fingers of both hands. Laboratory data on admission were as
follows: White blood cell, 4,900/μl; C-reactive protein, 3.77
mg/dl; anti-nuclear antibody, 1:640; anti-centromere antibody,
1:640; rheumatoid factor, 4 U/ml. Tests for anti-neutrophil
cytoplasmic antibodies to proteinase 3 and myeloperoxidase and
anti-ribonucleoprotein and -topoisomerase 1 antibodies were
negative. A chest radiograph revealed pneumothorax in the right
lung, and reticulonodular opacities predominant in the bilateral
lower lungs (Fig. 2). A 20 French
intercostal chest tube (Argyle thoracic catheter, Covidien, Tokyo,
Japan) was inserted into the pleural cavity, but the air leak
continued and no improvement of the pneumothorax was obtained. The
patient declined surgery; therefore, considering the deterioration
of her respiratory condition following pleurodesis by other
chemical agents, pleurodesis through the instillation of an
autologous blood-patch was selected. A total of 50 ml autologous
blood was injected via the chest tube. The tube was clamped for 3 h
and connected to suction. The procedure was repeated twice over the
next two days. Discontinuation of the air leak was achieved in
three days and the chest tube was removed. Eight months later the
patient was still well and attending the outpatient clinic without
any recurrent pneumothorax (Fig.
3). This therapy was approved by the National Health Insurance
of Japan as a postoperative persistent air leak therapy and by the
Ethics Committee of the Mito Medical Center, University of
Tsukuba-Mito Kyodo General Hospital (Mito, Japan). Informed consent
was obtained from the patient.
Discussion
PSS is a systemic disease that sometimes affects the
lungs, resulting in lung fibrosis (1). Diffuse interstitial fibrosis is the
most common pulmonary manifestation and pneumothorax is usually
associated with the pulmonary complication of interstitial fibrosis
(1). The underlying mechanism of
pneumothorax is believed to result from the rupture of acquired
subpleural cystic spaces associated with the diffuse interstitial
fibrosis (2). In patients with PSS
with interstitial fibrosis, the distinctive rigidity of lung
parenchyma may prevent pre-expansion of the ruptured lung.
Additionally, immunosuppressants including corticosteroids, which
are frequently used for PSS, may aggravate persistent air leak;
therefore, pneumothorax in patients with PSS often presents as a
difficult-to-treat disease and prognosis is predicted to be poor.
Chemical pleurodesis with tetracycline or talc has been
successfully used (3–5), but pleurodesis is more usually
performed once the air leak has resolved. Chemical pleurodesis
using such agents can contribute to the onset of acute exacerbation
of the interstitial fibrosis (4).
Furthermore, if pleurodesis can be successfully achieved, the
development of constrictive respiratory impairment may occur due to
pleural thickening as a result of the chemical pleurodesis. If
there is no improvement despite conservative treatment, a more
invasive approach may be necessary. Video-assisted thoracic surgery
is the next option for patients with recurrent pneumothorax and
those for whom conservative treatment was not successful (5,6). Due
to the severity of their underlying disease itself and their
respiratory condition, these patients are often not suitable
candidates for surgical treatment. As a consequence, their optimal
management may be eventful. As an alternative therapy, autologous
blood-patch pleurodesis has been used for the treatment of
pneumothorax (7–9). Blood outside its own environment is
an irritant; therefore, chest physicians must watch closely for an
allergic reaction. The injection is simple, painless, causes no
side effects and is an inexpensive treatment for pneumothorax
available not only for patients with persistent air leak but also
those with residual air space (10). In the case reported here, recurrent
pneumothorax developed shortly after surgical therapy for the
disease and there was persistent air leak as well as residual air
space. Due to the high risk of deterioration of the respiratory
condition of the patient by tight chemical pleurodesis, we selected
to seal the pleural space with the injection of autologous blood as
a successful pleurodesis agent in the treatment of recurrent
pneumothorax.
In conclusion, as an alternative therapy for
difficult-to-treat pneumothorax in patients with PSS with
persistent air leak and residual air space, autologous blood-patch
pleurodesis would be one of the treatment options.
References
|
1
|
Le Pavec J, Launay D, Mathai SC, Hassoun
PM and Humbert M: Scleroderma lung disease. Clin Rev Allergy
Immunol. 40:104–116. 2011.
|
|
2
|
Sripavatakul K and Foocharoen C:
Spontaneous pneumothorax from cryptococcal pneumonia in systemic
sclerosis: a case report. J Med Case Rep. 5:3092011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Light RW and Vargas FS: Pleural sclerosis
for the treatment of pneumothorax and pleural effusion. Lung.
175:213–223. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Rodriguez-Panadero F and Montes-Worboys A:
Mechanisms of pleurodesis. Respiration. 83:91–98. 2012. View Article : Google Scholar
|
|
5
|
Ramos-Izquierdo R, Moya J, Macia I, et al:
Treatment of primary spontaneous pneumothorax by videothoracoscopic
talc pleurodesis under local anesthesia: a review of 133
procedures. Surg Endosc. 24:984–987. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Shaikhrezai K, Thompson AI, Parkin C,
Stamenkovic S and Walker WS: Video-assisted thoracoscopic surgery
management of spontaneous pneumothorax - long-term results. Eur J
Cardiothorac Surg. 40:120–123. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Manley K, Coonar A, Wells F and Scarci M:
Blood patch for persistent air leak: a review of the current
literature. Curr Opin Pulm Med. 18:333–338. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Cagirici U, Sahin B, Cakan A, Kayabas H
and Buduneli T: Autologous blood patch pleurodesis in spontaneous
pneumothorax with persistent air leak. Scand Cardiovasc J.
32:75–78. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Dumire R, Crabbe MM, Mappin FG and
Fontenelle LJ: Autologous ‘blood patch’ pleurodesis for persistent
pulmonary air leak. Chest. 101:64–66. 1992.
|
|
10
|
Mallen JK, Landis JN and Frankel KM:
Autologous ‘blood patch’ pleurodesis for persistent pulmonary air
leak. Chest. 103:326–327. 1993.
|