Introduction
Non-fasting postprandial triglyceride (TG)
concentrations are more effective at predicting cardiovascular risk
than fasting TG concentrations; this association is independent of
traditional coronary risk factors (1,2).
TG-rich lipoproteins, including chylomicrons assembled by TGs,
dietary cholesterol and apolipoprotein B-48 (apoB-48), are
extremely atherogenic and contribute to coronary heart disease
development (3). Even in
normolipidemic individuals, postprandial hypertriglyceridemia
contributes to the generation of proinflammatory cytokines and
oxidative stress, causing endothelial dysfunction (4,5).
Thus, the identification of novel therapeutic approaches to target
postprandial lipid concentrations is of significant interest.
Vildagliptin is a selective inhibitor of dipeptidyl
peptidase-4 (DPP4) and has been demonstrated to reduce the fasting
and postprandial glucose levels in patients with type 2 diabetes,
possibly by inhibiting the inactivation of glucagon-like peptide-1
(GLP-1) (6–8). Clinical studies have revealed that
the long-term administration of DPP4 inhibitors improves the
postprandial atherogenic levels of TG-rich lipoprotein and/or
endothelial dysfunction in patients with type 2 diabetes and
healthy volunteers (9–11). However, Ayaori et al
reported that the effects of other DPP4 inhibitors attenuated
endothelial dysfunction in patients with type 2 diabetes (12). Thus, the difference in effects on
endothelial function among DPP4 inhibitors remains controversial.
Furthermore, following long-term treatment with DPP4 inhibitors,
the discrimination between the acute and chronic effects of
vildagliptin is difficult.
α-glucosidase inhibitors, which lower postprandial
plasma glucose levels by delaying the absorption of sugars from the
digestive system, are used widely in the treatment of type 2
diabetes. A previous study also showed that treatment with
voglibose improves endothelial function in type diabetes mellitus
(13). Another study investigated
the effect of voglibose on postprandial triglyceridemia following a
meal test, but failed to show the benefit of voglibose compared
with the placebo (14). The aim of
the present study was to examine the postprandial effects of a
single administration of vildagliptin and voglibose, an
α-glucosidase inhibitor, on endothelial dysfunction and the lipid
profile in normal individuals.
Materials and methods
Participants and study design
The procedures carried out in the present study were
approved by the Ethics Committee of Okayama Rohsai Hospital
(Okayama, Japan) and written informed consent was obtained from all
volunteers prior to the study commencement. The study procedures
conformed to the ethical guidelines of the 1975 Declaration of
Helsinki, as reflected by the a priori approval of the
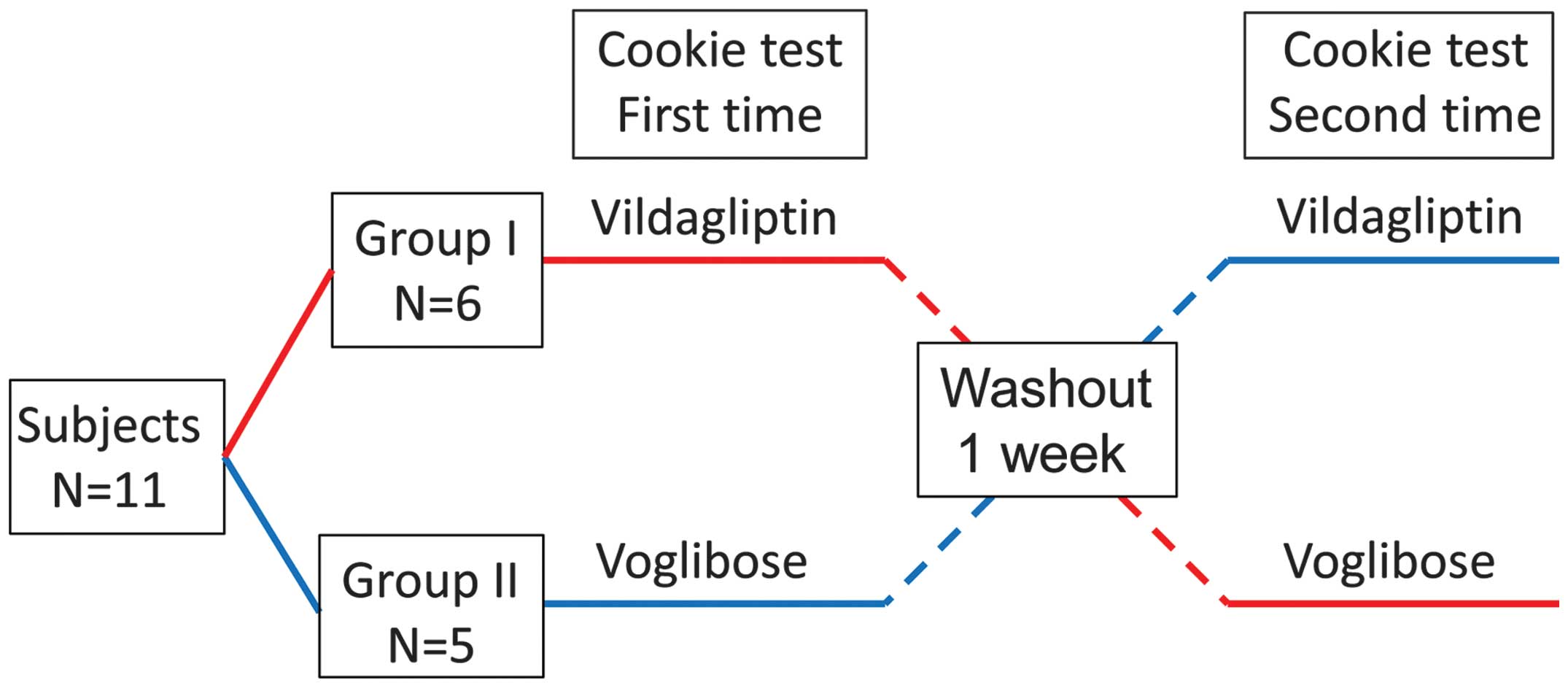
Ethics Committee of the hospital. The study was a randomized,
double-blind, cross-over study (Fig.
1), and all procedures were carried out at the Okayama Rohsai
Hospital. A total of 11 volunteers were recruited through clinical
study sites and community outreach between September and November
2012. A single dose of vildagliptin (50 mg; Novartis
Pharmaceuticals Co., Tokyo, Japan) or voglibose (0.3 mg; Takeda
Pharmaceutical Co Ltd, Tokyo, Japan) was administered and a
one-week washout period was implemented prior to the administration
of the second drug. The drugs were administered in a random order.
All volunteers underwent medical check-ups and family histories
were obtained in medical interviews. None of the 11 participants
had hypertension, impaired glucose tolerance, dyslipidemia, or
cerebrovascular or cardiovascular disease. The pre-specified
primary outcome measure was the difference in the decrease in
brachial artery flow-mediated dilation (FMD) following the
cookie-loading test, and the secondary outcome measure was the
difference in lipids profiles following the cookie-loading
test.
Cookie-loading test procedure
Following overnight fasting for ≥8–12 h, one tablet
of vildagliptin or voglibose was taken 1 h prior to the
cookie-loading test. The cookie consisted of 75 g carbohydrate,
28.5 g fat and 8 g protein with a total of 592 kcal per carton
(Saraya Co., Osaka, Japan). Participants were instructed to consume
the cookie with water within 20 min. Time measurements were
initiated when half the cookie had been consumed. Biological
parameters in the blood and endothelium-dependent FMD were assessed
during fasting and 1.5 and 3 h after the cookie-loading test.
Measurement of biochemical
parameters
The following parameters were measured in the blood
by SRL Inc., (Tokyo, Japan) in the state of fasting prior to cookie
ingestion: Serum total cholesterol (total-C), TG, low-density
lipoprotein cholesterol (LDL-C), high-density lipoprotein
cholesterol (HDL-C), apoB-48, glucagon, GLP-1, insulin, hemoglobin
A1c and glucose levels. Serum levels of total-C, TG, LDL-C,
apoB-48, GLP-1, glucagon, insulin and glucose were measured 1.5 and
3 h after the cookie-loading test.
Measurement of FMD
During fasting and 1.5 and 3 h after cookie
ingestion, measurements of FMD were performed by the same
technician who was blinded to the study design and medication
status. FMD was assessed as a parameter of vasodilation according
to the guidelines for ultrasound assessment of FMD of the brachial
artery using a 10-MHz linear array transducer probe (Unex Co.,
Nagoya, Japan) (11). Longitudinal
images of the brachial artery at baseline were recorded with a
stereotactic arm and the artery diameter was measured following
supine rest for ≥5 min. The diameter of the artery was measured
from the clear anterior (media-adventitia) and posterior
(intima-media) interfaces, which were manually determined.
Suprasystolic compression (50 mmHg higher than the systolic blood
pressure) was subsequently performed on the right forearm for 5 min
and measurements of the artery diameter were made continuously from
30 sec before to ≥2 min after cuff release. Maximum vasodilation
was evaluated from the change in artery diameter following release
from occlusion (%FMD).
Statistical analysis
The sample size was determined based on the
estimated FMD reported in a recent study (11). It was assumed that the mean
improvement in postprandial %FMD was 2.7% and that the standard
deviation was 2.0%. To use a two-sided test for differences, a
minimal sample size of 10 individuals was required in each group to
detect statistical differences in %FMD with a power of 80% and an
α-type error of 5%. Results are expressed as the mean ± standard
error. Differences in lipid profile and endothelial function
between the two groups were compared using the Wilcoxon signed-rank
test. P<0.05 was considered to indicate a statistically
significant difference.
Results
A total of 11 volunteers (seven males and four
females) were recruited. The mean age and body mass index of the
volunteers was 32±2 years and 22.0±0.7 kg/m2,
respectively. Participants maintained their weight throughout the
study period.
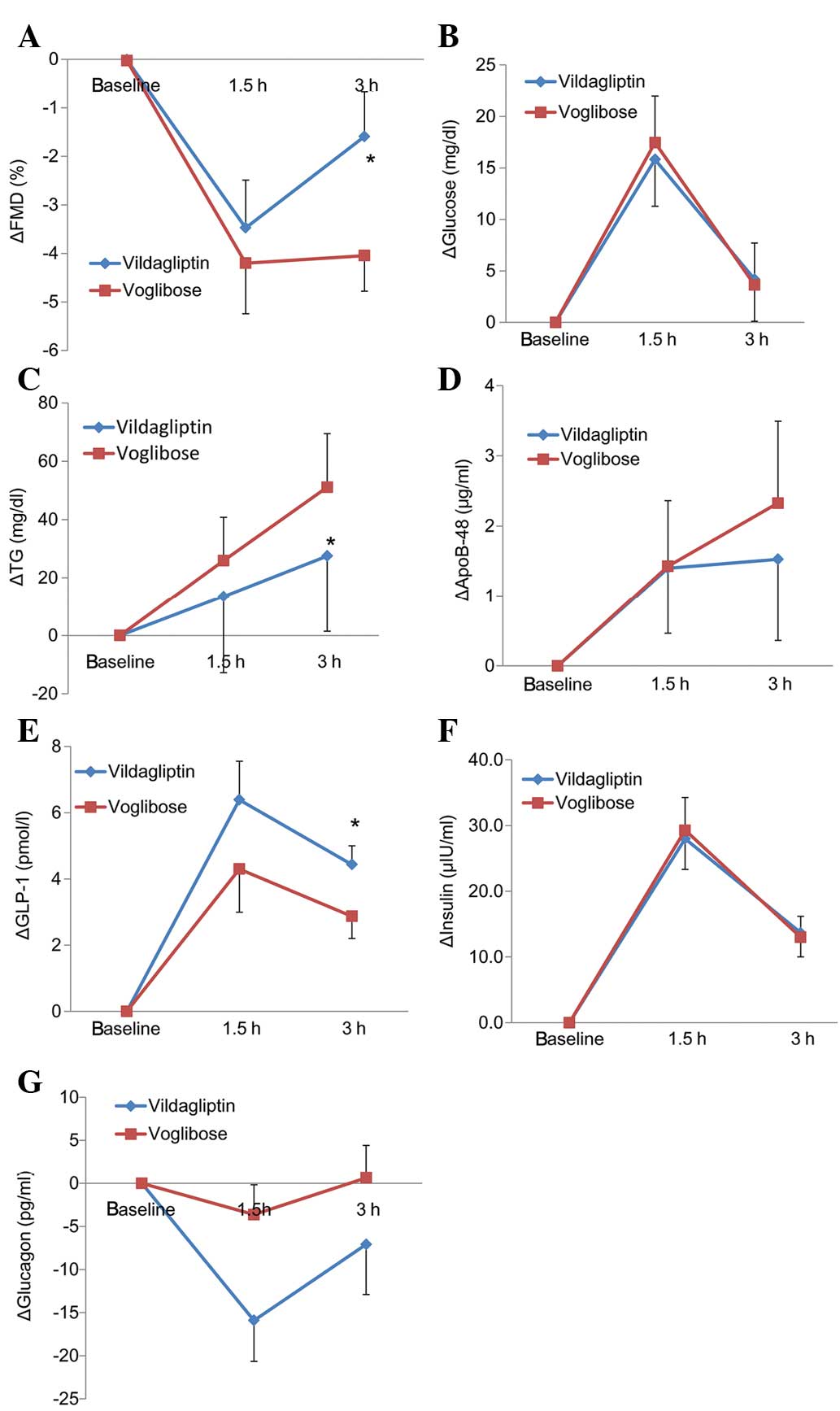
The comparison of postprandial endothelial function,
which was assessed as the %FMD, between the vildagliptin and
voglibose groups is shown in Table
I. In the voglibose group, the postprandial %FMD decreased
significantly until 3 h; however, the decrease in postprandial %FMD
in the vildagliptin group was higher compared with that in the
voglibose group (9.7±0.9 vs. 7.2±0.7%, respectively; Table I). The changes in the %FMD are
shown in Table I and Fig. 2A. The change in the %FMD from
baseline to 3 h was significantly lower in the vildagliptin group
compared with that in the voglibose group (−1.6±0.9 vs. −4.0±0.7%,
respectively; P=0.01; Fig.
2A).
 | Table ILipid profile, apolipoprotein B-48,
glucose, glucagon, GLP-1, insulin and %FMD measurements after the
cookie test. |
Table I
Lipid profile, apolipoprotein B-48,
glucose, glucagon, GLP-1, insulin and %FMD measurements after the
cookie test.
| A, Biochemical
parameters |
|---|
|
|---|
| Parameter | Fasting | 1.5 h | 3 h |
|---|
| Total-cholesterol
(mg/dl) |
| Voglibose | 188±11 | 180±11 | 175±15 |
| Vildagliptin | 190±13 | 192±13 | 187±12 |
| LDL-cholesterol
(mg/dl) |
| Voglibose | 114±11 | 107±10 | 110±10 |
| Vildagliptin | 110±13 | 113±14 | 107±12 |
| HDL-cholesterol
(mg/dl) |
| Voglibose | 58±3 | 57±3 | 56±3 |
| Vildagliptin | 60±3 | 60±3 | 59±3 |
| Triglyceride
(mg/dl) |
| Voglibose | 98±17 | 124±26 | 149±26 |
| Vildagliptin | 94±15 | 108±15 | 122±18 |
| Apolipoprotein B-48
(μg/ml) |
| Voglibose | 4.9±1.0 | 6.3±0.9 | 7.2±1.2 |
| Vildagliptin | 4.0±0.6 | 5.4±0.7a | 5.5±0.7 |
| Glucose (mg/dl) |
| Voglibose | 98±2 | 115±6 | 101±4 |
| Vildagliptin | 97±2 | 113±5 | 101±5 |
| Glucagon (pg/ml) |
| Voglibose | 71±8 | 68±9 | 72±9 |
| Vildagliptin | 76±8 | 61±8 | 69±9 |
| GLP-1 (pmol/l) |
| Voglibose | 3.4±0.7 | 7.7±1.5 | 6.3±1.1 |
| Vildagliptin | 4.6±0.9 | 11.0±1.7a | 9.0±1.1a |
| Insulin (μU/ml) |
| Voglibose | 5.2±0.7 | 34.5±5.2 | 18.2±3.5 |
| Vildagliptin | 6.3±0.9 | 34.3±5.4 | 20.0±4.3 |
|
| B, Endothelial
function |
|
| Parameter | Fasting | 1.5 h | 3 h |
|
| FMD (%) |
| Voglibose | 11.2±1.2 | 7.0±1.0 | 7.2±0.7a |
| Vildagliptin | 11.3±1.3 | 7.8±1.0 | 9.7±0.9 |
The levels of lipid/lipoprotein, glucose, glucagon,
GLP-1 and insulin in the postprandial state are shown in Table I and Fig. 2. The level of apoB-48 1.5 h after
the cookie-loading test in the vildagliptin group was significantly
lower compared with that in the voglibose group. The levels of
GLP-1 1.5 and 3 h after cookie ingestion in the vildagliptin group
were significantly higher than those in the voglibose group.
Changes in the levels of lipid/lipoprotein, glucose, glucagon,
GLP-1 and insulin following the cookie-loading test are shown in
Fig. 2 and Table I. The change in the level of TG
from baseline to 3 h was significantly lower in the vildagliptin
group compared with that in the voglibose group. The change in the
level of GLP-1 from baseline to 3 h was significantly higher in the
vildagliptin group than that in the voglibose group. The changes in
the levels of apoB-48, glucose, glucagon and insulin from baseline
to 3 h did not significantly differ between the vildagliptin and
voglibose groups.
Discussion
The results of the present study demonstrated that a
single administration of vildagliptin significantly attenuated
postprandial endothelial dysfunction (which was induced by a
standard meal loading test) when compared with voglibose and that
vildagliptin reduced postprandial levels of TG.
Our previous study revealed that alogliptin
treatment for one week ameliorated postprandial
hypertriglyceridemia and endothelial dysfunction in non-diabetic
individuals (11). Other studies
have demonstrated that treatment with vildagliptin for four weeks
and sitagliptin for six weeks decreased the postprandial levels of
TG and apoB-48 following a fat-loading test in patients with type 2
diabetes (9,10). However, the present study is, to
the best of our knowledge, the first to demonstrate that a single
administration of vildagliptin reduces the postprandial increase in
TG that accompanies postprandial endothelial dysfunction in healthy
individuals. Following long-term treatment with DPP4 inhibitors,
the discrimination between the acute and chronic effects of
vildagliptin is difficult. The present study clearly demonstrated
the acute effects of vildagliptin on postprandial endothelial
dysfunction and hypertriglyceridemia.
There are several possible mechanisms underlying the
effect of vildagliptin on postprandial endothelial dysfunction and
hypertriglyceridemia. Regarding the attenuation of endothelial
dysfunction, the increased expression of GLP-1 induced by
vildagliptin may directly protect endothelial cells from
hypertriglyceridemia. Clinical studies have demonstrated that GLP-1
analogs improve endothelial function in patients with type 2
diabetes (15–17). An experimental study reported that
GLP-1 activated endothelial nitric oxide synthase in endothelial
cells (18). Regarding the
attenuation of hypertriglyceridemia, one study demonstrated that
GLP-1 affected intestinal TG absorption (19), possibly by inhibiting gastric
lipase (20). Another study has
shown that GLP-1 may directly regulate lipoprotein assembly or the
secretion of chylomicron in enterocytes (21).
A number of previous studies have demonstrated that
treatment with α-glucosidase inhibitors, including acarbose or
miglitol, for >3 months improves postprandial endothelial
dysfunction in patients with diabetes or coronary artery disease
(22,23). However, only one study reported
that a single administration of miglitol significantly improved
postprandial glucose and lipid metabolism and incretin secretion,
and attenuated endothelial dysfunction in patients with diabetes
following a standard meal loading; no favorable effects were
observed following the administration of voglibose or a placebo
(14). Despite the fact that the
present study lacked a placebo group, the previous results support
the findings of the current study that a single administration of
vildagliptin significantly reduced the increase in TG following the
cookie-loading test.
The present study had several important limitations.
Firstly, the number of participants was small and therefore
selection bias may have occurred. Secondly, no standardized method
for assessing postprandial hypertriglyceridemia has been
established. Thus, a range of fat-loading tests, including an oral
fat meal, fat cream intake and intravenous fat loading, have been
used in previous studies (14,24).
The present study utilized the cookie-loading test, which provided
sufficient information regarding glucose intolerance and
postprandial hypertriglyceridemia (11). Although the cookie provided a fixed
amount of fat (28.5 g) per individual, the amount of fat
administered per body surface area was not regulated. Therefore,
the contribution of the fat metabolism of each individual cannot be
excluded as an influential factor.
In conclusion, the present study compared the
postprandial effects of vildagliptin and voglibose on endothelial
dysfunction and lipid profiles. It was demonstrated that a single
administration of the DPP4 inhibitor vildagliptin was effective at
ameliorating the postprandial endothelial dysfunction, accompanied
by a reduction in the postprandial elevation of TG. Vildagliptin
shows potential as a drug to target cardiovascular disease by
ameliorating endothelial dysfunction in the postprandial state,
even in low-risk individuals.
References
|
1
|
Bansal S, Buring JE, Rifai N, et al:
Fasting compared with nonfasting triglycerides and risk of
cardiovascular events in women. JAMA. 298:309–316. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Nordestgaard BG, Benn M, Schnohr P and
Tybjaerg-Hansen A: Nonfasting triglycerides and risk of myocardial
infarction, ischemic heart disease, and death in men and women.
JAMA. 298:299–308. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Véniant MM, Pierotti V, Newland D, et al:
Susceptibility to atherosclerosis in mice expressing exclusively
apolipoprotein B48 or apolipoprotein B100. J Clin Invest.
100:180–188. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Bae JH, Bassenge E, Kim KB, et al:
Postprandial hypertriglyceridemia impairs endothelial function by
enhanced oxidant stress. Atherosclerosis. 155:517–523. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
van Oostrom AJ, Sijmonsma TP, Verseyden C,
et al: Postprandial recruitment of neutrophils may contribute to
endothelial dysfunction. J Lipid Res. 44:576–583. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
DeFronzo RA, Fleck PR, Wilson CA and Mekki
Q: Alogliptin Study 010 Group: Efficacy and safety of the
dipeptidyl peptidase-4 inhibitor alogliptin in patients with type 2
diabetes and inadequate glycemic control: a randomized,
double-blind, placebo-controlled study. Diabetes Care.
31:2315–2317. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Feng J, Zhang Z, Wallace MB, et al:
Discovery of alogliptin: a potent, selective, bioavailable, and
efficacious inhibitor of dipeptidyl peptidase IV. J Med Chem.
50:2297–2300. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Moritoh Y, Takeuchi K, Asakawa T, Kataoka
O and Odaka H: Chronic administration of alogliptin, a novel,
potent, and highly selective dipeptidyl peptidase-4 inhibitor,
improves glycemic control and beta-cell function in obese diabetic
ob/ob mice. Eur J Pharmacol. 588:325–332. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Matikainen N, Mänttäri S, Schweizer A, et
al: Vildagliptin therapy reduces postprandial intestinal
triglyceride-rich lipoprotein particles in patients with type 2
diabetes. Diabetologia. 49:2049–2057. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Tremblay AJ, Lamarche B, Deacon CF,
Weisnagel SJ and Couture P: Effect of sitagliptin therapy on
postprandial lipoprotein levels in patients with type 2 diabetes.
Diabetes Obes Metab. 13:366–373. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Noda Y, Miyoshi T, Oe H, et al: Alogliptin
ameliorates postprandial lipemia and postprandial endothelial
dysfunction in non-diabetic subjects: a preliminary report.
Cardiovasc Diabetol. 12:82013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ayaori M, Iwakami N, Uto-Kondo H, et al:
Dipeptidyl peptidase-4 inhibitors attenuate endothelial function as
evaluated by flow-mediated vasodilatation in type 2 diabetic
patients. J Am Heart Assoc. 2:e0032772013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Nakamura K, Oe H, Kihara H, et al: DPP-4
inhibitor and alpha-glucosidase inhibitor equally improve
endothelial function in patients with type 2 diabetes: EDGE study.
Cardiovasc Diabetol. 13:1102014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Hiki M, Shimada K, Kiyanagi T, et al:
Single administration of alpha-glucosidase inhibitors on
endothelial function and incretin secretion in diabetic patients
with coronary artery disease - Juntendo University trial: effects
of miglitol on endothelial vascular reactivity in type 2 diabetic
patients with coronary heart disease (J-MACH). Circ J.
74:1471–1478. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Basu A, Charkoudian N, Schrage W, et al:
Beneficial effects of GLP-1 on endothelial function in humans:
dampening by glyburide but not by glimepiride. Am J Physiol
Endocrinol Metab. 293:E1289–E1295. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ceriello A, Esposito K, Testa R, et al:
The possible protective role of glucagon-like peptide 1 on
endothelium during the meal and evidence for an ‘endothelial
resistance’ to glucagon-like peptide 1 in diabetes. Diabetes Care.
34:697–702. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Nyström T, Gutniak MK, Zhang Q, et al:
Effects of glucagon-like peptide-1 on endothelial function in type
2 diabetes patients with stable coronary artery disease. Am J
Physiol Endocrinol Metab. 287:E1209–E1215. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Hattori Y, Jojima T, Tomizawa A, et al: A
glucagon-like peptide-1 (GLP-1) analogue, liraglutide, upregulates
nitric oxide production and exerts anti-inflammatory action in
endothelial cells. Diabetologia. 53:2256–2263. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Qin X, Shen H, Liu M, et al: GLP-1 reduces
intestinal lymph flow, triglyceride absorption, and apolipoprotein
production in rats. Am J Physiol Gastrointest Liver Physiol.
288:G943–G949. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Wøjdemann M, Wettergren A, Sternby B, et
al: Inhibition of human gastric lipase secretion by glucagon-like
peptide-1. Dig Dis Sci. 43:799–805. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hsieh J, Longuet C, Baker CL, et al: The
glucagon-like peptide 1 receptor is essential for postprandial
lipoprotein synthesis and secretion in hamsters and mice.
Diabetologia. 53:552–561. 2010. View Article : Google Scholar
|
|
22
|
Kato T, Inoue T and Node K: Postprandial
endothelial dysfunction in subjects with new-onset type 2 diabetes:
an acarbose and nateglinide comparative study. Cardiovasc Diabetol.
9:122010. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Kitano D, Chiku M, Li Y, et al: Miglitol
improves postprandial endothelial dysfunction in patients with
acute coronary syndrome and new-onset postprandial hyperglycemia.
Cardiovasc Diabetol. 12:922013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Masuda D, Nakagawa-Toyama Y, Nakatani K,
et al: Ezetimibe improves postprandial hyperlipidaemia in patients
with type IIb hyperlipidaemia. Eur J Clin Invest. 39:689–698. 2009.
View Article : Google Scholar : PubMed/NCBI
|