Introduction
Concurrent contralateral inguinal exploration in
children with unilateral hernia or hydrocele is a subject of
considerable debate. In 1952, Duckett reported that a contralateral
hernia was present in as many as 30% of children presenting with
unilateral hernias (1). In 1955,
Rothenberg and Barnett recommended prophylactic contralateral
exploration in all children (2).
However, a meta-analysis revealed that the risk of contralateral
hernia is only 5.76% (3). In
addition, a previous study by the present authors found that the
incidence was 9.5% (4). Therefore,
it is widely considered that contralateral groin exploration is not
justified in children with unilateral disease due to the low
incidence of contralateral hernia and the potential for operative
complications.
To avoid unnecessary contralateral inguinal
exploration, several preoperative diagnostic tools, such as
physical examination and herniography, have been used. However,
these tests have low accuracy rates and high false positive rates
(5). In 1992, laparoscopy was
introduced as a tool for the diagnosis of contralateral patent
processus vaginalis (CPPV) (6). If
CPPV is observed laparoscopically, the PPV can be repaired through
a groin incision or laparoscopy. Transinguinal laparoscopy
(inguinoscopy) has been shown to be a safe, accurate and effective
method of evaluating the contralateral side (7). Regardless of the convenience and
accuracy of laparoscopy, performing laparoscopy for all patients
with unilateral hernia or hydrocele is unreasonable.
The aim of the present study was to investigate the
incidence of CPPV using inguinoscopy. In order to aid the selection
of appropriate candidates for contralateral examination, the risk
factors for CPPV were evaluated.
Patients and methods
Patients
Patients who presented with a unilateral hydrocele,
inguinal hernia or cryptorchidism between November 2001 and March
2008 were enrolled. All data were collected prospectively. The
study protocol was approved by the Samsung Medical Center
Institutional Review Board (Seoul, Korea), and written informed
consent was obtained from the patient’s relatives. Clinically
bilateral disease and patients older than 6 years were excluded. In
total, 119 patients were enrolled. All patients underwent
concurrent transinguinal laparoscopy (inguinoscopy) during the
initial surgery. The case records were reviewed for each patient
and the variables evaluated included age at surgery; the side
affected by hydrocele, inguinal hernia or cryptorchidism;
gestational age; and birth weight. To define the risk factors for
CPPV, the presence of the following was also assessed: i) previous
history of contralateral hydrocele or hernia, which meant that the
patient had presented with contralateral hydrocele or hernia in the
past but did not have clinical contralateral disease at the time of
the surgery; ii) suspicion of contralateral hydrocele on physical
examination, which meant the patient did not have contralateral
disease clinically but had scanty fluid or sac-like materials
within the scrotum on palpation; and iii) findings suspicious for
contralateral hydrocele (scanty fluid collection within the
scrotum) on ultrasound.
One surgeon performed all the surgeries and physical
examinations. As the herniated contents of the inguinal hernia
included not only peritoneal fluid but also intestine or omentum,
it was postulated that the hernia sac was wider than the hydrocele
sac. The presence of an ipsilateral inguinal hernia was evaluated
as a risk factor for CPPV.
Inguinoscopy
Inguinoscopy was performed during the ipsilateral
surgery. The hernia sac was dissected free from the spermatic cord
and traced to the internal inguinal ring. The sac was opened at the
middle inguinal canal and a 4-mm reusable trocar was introduced
through the hernia sac. CO2 gas was insufflated at a
flow rate of 1 l/min to a pressure of 8–10 mmHg. A 45°-angled
3.3-mm endoscope was then introduced, and the contralateral
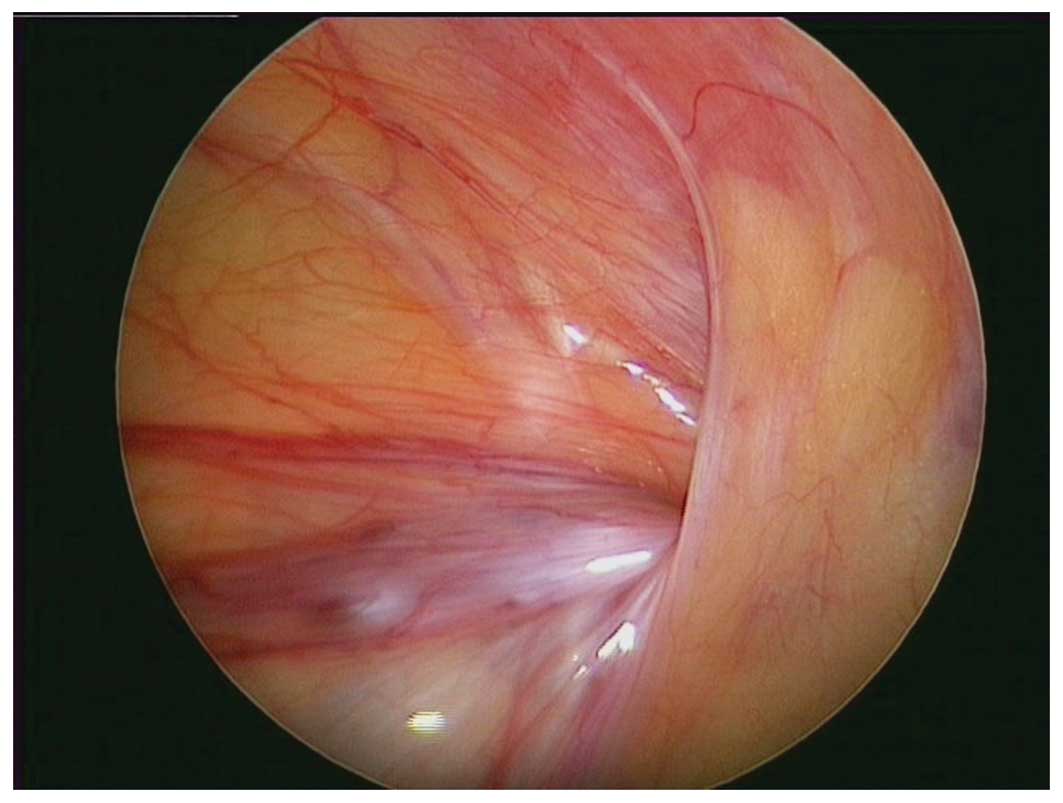
internal inguinal ring was observed. Diagnostic criteria of CPPV
(Fig. 1) on inguinoscopy were as
follows: i) visible CPPV with passage of a guidewire >5 cm into
the inguinal canal by >5 cm; ii) guidewire palpable in the
contralateral scrotum; iii) bulging of the contralateral side
during gas inflation; and iv) crepitus or air bubbles from the
inguinal canal during scrotal manipulation.
Statistical analysis
To evaluate each risk factor, univariate analysis
was performed by Pearson Chi-square or Fisher’s exact tests.
Logistic regression analysis was conducted to evaluate the
association between risk factors and CPPV. Risk factors were
reported with 95% confidence intervals. Data were analyzed using
PASW® Statistics, version 18.0 (SPSS, Inc., Chicago, IL,
USA). A P-value <0.05 was considered to indicate a statistically
significant result.
Results
Patient characteristics
The patients ranged in age from 8 to 72 months
(median, 34 months). The median gestational age was 39.0 weeks
(range, 26–41 weeks) and the mean birth weight was 3.2±0.50 kg
(range, 2.2–4.3 kg). There were 62 children (52.1%) that presented
with disease on the right, and 57 children (47.9%) that presented
with disease on the left (Table
I). Among these children, 87 (73.1%) presented with indirect
inguinal hernia, 19 (16.0%) presented with cryptorchidism, and the
remaining 13 (10.9%) presented with communicating hydrocele. Eight
children (6.7%) had a history of preterm birth (gestational age
<37 weeks), and five children (4.2%) had a history of low birth
weight (birth weight <2.5 kg). There was history of a previous
hydrocele or hernia on the contralateral side in 22 patients
(18.5%), a suspicious physical examination in 46 patients (38.7%),
and a suspicious ultrasound result in 8 patients (6.7%). Of the 119
patients, 29 patients (24.4%) had CPPV confirmed by inguinoscopy.
No operative complications were observed during the
inguinoscopy.
 | Table IPatient characteristics. |
Table I
Patient characteristics.
| Variables | Value |
|---|
| Age at surgery
(median, range, months) | 34 (8–72) |
| Birth weight (mean ±
SD, kg) | 3.2±0.50 |
| Gestational age
(median, range, weeks) | 39 (26–41) |
| Affected side [n
(%)] |
| Right | 62 (52.1) |
| Left | 57 (47.9) |
Risk factors for CPPV
In the univariate analysis, cases with suspicious
ultrasound findings had a higher incidence of CPPV than cases
without suspicious findings (P=0.020). Age, preterm birth, lower
birth weight, the affected side, a previous history of
contralateral disease, a suspicious physical examination, an
ipsilateral hernia, and ipsilateral cryptorchidism did not
influence the incidence of CPPV (Table II). Multivariate analysis revealed
that cases with suspicious ultrasound findings had a greater risk
of CPPV than cases with normal findings (odds ratio, 13.800;
P=0.004; Table III). A previous
history of contralateral disease was also found to be a significant
risk factor (odds ratio, 4.008; P=0.019).
 | Table IIUnivariate analysis of risk factors
for contralateral patent processus vaginalis. |
Table II
Univariate analysis of risk factors
for contralateral patent processus vaginalis.
| Variables | N (%) | Contralateral patent
processus vaginalis [n (%)] | P-value |
|---|
| Age | | | |
| ≤2 years | 34 (28.6) | 6 (17.6) | 0.280 |
| >2 years | 85 (71.4) | 23 (27.1) | |
| Laterality | | | |
| Right | 62 (52.1) | 13 (21.0) | 0.399 |
| Left | 57 (47.9) | 16 (28.1) | |
| Gestestional age | | | |
| <37 weeks | 8 (6.7) | 2 (25) | 0.625a |
| ≥37 weeks | 111 (93.3) | 27 (24.3) | |
| Birth weight | | | |
| <2.5 kg | 5 (4.2) | 2 (40) | 0.594a |
| ≥2.5 kg | 114 (95.8) | 27 (23.7) | |
| Previous history | | | |
| Yes | 22 (18.5) | 9 (40.9) | 0.057 |
| No | 97 (81.5) | 20 (20.6) | |
| Physical
examination | | | |
| Abnormal | 46 (38.7) | 14 (30.4) | 0.221 |
| Normal | 73 (61.3) | 15 (20.5) | |
| Ipsilateral
hernia | | | |
| Yes | 19 (16.0) | 2 (10.5) | 0.154a |
| No | 100 (84.0) | 27 (27.0) | |
| Ipsilateral
undescended testis | | | |
| Yes | 13 (10.9) | 2 (15.4) | 0.732a |
| No | 106 (89.1) | 27 (25.5) | |
| Ultrasound | | | |
| Abnormal | 8 (6.7) | 5 (62.5%) | 0.020 |
| Normal | 111 (93.3) | 24 (20.2) | |
 | Table IIIMultivariate analysis of risk factors
for contralateral patent processus vaginalis. |
Table III
Multivariate analysis of risk factors
for contralateral patent processus vaginalis.
| Risk factors | Odds ratio | 95% confidence
interval | P-value |
|---|
| Age ≤2 years | 0.411 | 0.108–0.559 | 0.191 |
| Right laterality | 0.674 | 0.253–1.797 | 0.430 |
| Preterm | 1.327 | 0.139–12.671 | 0.806 |
| Low birth weight | 0.702 | 0.056–8.723 | 0.783 |
| Previous history | 4.008 | 1.254–12.805 | 0.019 |
| Abnormal physical
examination | 2.839 | 0.992–8.123 | 0.052 |
| Ipsilateral
hernia | 0.419 | 0.078–2.251 | 0.310 |
| Ipsilateral
undescended testis | 0.583 | 0.092–3.694 | 0.567 |
| Suspicious ultrasound
findings | 13.800 | 2.311–82.390 | 0.004 |
Discussion
There has been ongoing debate regarding concurrent
contralateral inguinal exploration in children with unilateral
inguinal hernia or hydrocele. The benefits of contralateral
inguinal exploration include prevention of additional anesthesia
and surgeries, minimizing parental and patient inconvenience,
elimination of the possibility of incarceration, and reduced costs
(8). By contrast, the dissenting
opinion is that the true incidence of contralateral inguinal hernia
is low (9). Recent studies have
indicated that the incidence of metachronous contralateral inguinal
hernia may be lower than originally expected. Meta-analyses have
revealed an incidence rate of 5.76–7.2% (3,10,11).
In addition, there is the potential for complications, including
testicular atrophy and injury of the vas deferens or spermatic
vessel, during the exploration (12).
As a result of this debate, there have been many
efforts to identify appropriate candidates for exploration of the
contralateral groin. The goal is to uncover the presence of CPPV. A
PV is formed during the descent of the testis from the abdominal
cavity to the scrotum (13). It is
an extension of the peritoneum that is created by the pulling-down
effect of the migrating testis on the lower abdominal peritoneal
surface. Normally, the processus vaginalis is eradicated from the
internal inguinal ring to the upper scrotum. However, if the
processus vaginalis persists, peritoneal fluid is able to freely
communicate with the scrotal limits of the processus, resulting in
a communicating hydrocele. Inguinal hernias also develop due to the
same anatomic defect that is seen in cases of a communicating
hydrocele (13). The sac may
contain small intestine, omentum, bladder or genital contents. As
the majority of undescended testes, when examined, are found to
have an accompanying patent processus, it is important that a
cryptorchid testis is not missed when a child with a communicating
hydrocele is examined (14).
The simplest and noninvasive method of diagnosis is
physical examination using the silk glove sign. This involves
detecting thickening and silkiness on palpating the spermatic cord
as it crosses the pubic tubercle. Luo and Chao reported high
sensitivity and specificity for this method (15). However, the results may vary
depending on the examiner. Although the silk glove sign was not
used in the present study, the physical examination by an
experienced physician was not able to anticipate CPPV in the
present study.
Laparoscopic examination is a recently introduced
tool for the diagnosis of CPPV. Laparoscopy enables the direct
visualization of anatomic defects of the contralateral internal
inguinal ring. The sensitivity and specificity have been calculated
to be 99.4 and 99.5%, respectively (5). Studies have shown that the additional
time required for laparoscopic inspection is only 2–17 min
(16). Laparoscopic evaluation may
be performed using one of two methods. One method uses an umbilical
approach (17); the other uses a
transinguinal approach. The latter is performed more commonly and
was the approach used in the present study. A trocar was inserted
through the ipsilateral sac without a separate skin incision.
Therefore, inguinoscopy may have a reduced risk of complications,
as compared with an umbilical approach, particularly those
associated with trocar placement. In the present study, no
complications related to inguinoscopy were observed.
However, inguinoscopy has certain limitations. Since
the peritoneal veil sometimes partially covers the internal
inguinal ring, a direct view of the inguinal ring can be
interrupted. The failure rates are reported as 3–8% (5). Although it was not always possible to
observe the opened ring directly, bulging of the contralateral
scrotum during gas inflation or air bubbles from the inguinal canal
during scrotal manipulation are also evidence of PPV. Thus, it is
considered that these diagnostic observations can overcome the
limited visibility.
Controversy exists concerning whether the PPV should
be closed. Not all PPVs develop into clinical inguinal hernia or
hydrocele, and the PPV is sometimes obliterated spontaneously.
Although ~80–94% of newborn infants have a PPV, ~60% will have
disappeared by the time the child is 2 years old (18). In addition, the PPV may not cause
the patient any problems. Autopsy data suggest that 15–30% of
adults without a hernia have a PPV (19). The reported incidence of
metachronous contralateral inguinal hernia is lower than the
incidence of CPPV. The reported incidence of CPPV is 22–48%
(7,20–27),
which is similar to the incidence observed in the present
study.
Laparoscopic examination is important for avoiding
unnecessary inguinal exploration; however, the selection of
appropriate patients is important in order to prevent unnecessary
laparoscopy. In the present study, the significant risk factors for
CPPV were found to be suspicious ultrasound findings and a history
of contralateral disease. Therefore, it is concluded that it is
beneficial to perform inguinoscopy in children with these risk
factors. In addition to the risk factors identified in the present
study, children with other well-known risk factors may also be
candidates for inguinoscopy. As children with peritoneal dialysis,
ventriculo-peritoneal shunts or ascites have increased
intra-abdominal pressure, their risk of developing symptomatic
disease is high. Children with contraindications for general
anesthesia may benefit from inguinoscopy as it may avoid a second
surgery.
In the present study, the incidence of CPPV was
24.4%. The significant risk factors for CPPV were suspicious
ultrasound findings and a history of contralateral disease.
Therefore, it is concluded that it is beneficial to perform
inguinoscopy in children with these risk factors.
References
|
1
|
Duckett JW: Treatment of congenital
inguinal hernia. Ann Surg. 135:879–885. 1952. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Rothenberg RE and Barnett T: Bilateral
herniotomy in infants and children. Surgery. 37:947–950.
1955.PubMed/NCBI
|
|
3
|
Nataraja R and Mahomed A: Systematic
review for paediatric metachronous contralateral inguinal hernia: a
decreasing concern. Pediatr Surg Int. 27:953–961. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Lee DG, Park KH and Baek M: The
possibility of contralateral occurrence after unilateral hydrocele
or inguinal hernia repair in children. Korean J Ped Urol. 2:43–46.
2010.(In Korean).
|
|
5
|
Miltenburg DM, Nuchtern JG, Jaksic T, et
al: Laparoscopic evaluation of the pediatric inguinal hernia - a
meta-analysis. J Pediatr Surg. 33:874–879. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Lobe TE and Schropp KP: Inguinal hernias
in pediatrics: initial experience with laparoscopic inguinal
exploration of the asymptomatic contralateral side. J Laparoendosc
Surg. 2:135–141. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Chu CC, Chou CY, Hsu TM, et al:
Intraoperative laparoscopy in unilateral hernia repair to detect a
contralateral patent processus vaginalis. Pediatr Surg Int.
8:385–388. 1993. View Article : Google Scholar
|
|
8
|
Lee SL, Sydorak RM and Lau ST:
Laparoscopic contralateral groin exploration: is it cost effective?
J Pediatr Surg. 45:793–795. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Sözübir S, Ekingen G, Senel U, Kahraman H
and Güvenç BH: A continuous debate on contralateral processus
vaginalis: evaluation technique and approach to patency. Hernia.
10:74–78. 2006. View Article : Google Scholar
|
|
10
|
Ron O, Eaton S and Pierro A: Systematic
review of the risk of developing a metachronous contralateral
inguinal hernia in children. Br J Surg. 94:804–811. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Miltenburg DM, Nuchtern JG, Jaksic T, et
al: Meta-analysis of the risk of metachronous hernia in infants and
children. Am J Surg. 174:741–744. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Godbole PP and Stringer MD: Patent
processus vaginalis. Pediatric Urology. Gearhart JP, Rink RC and
Mouriquand PDE: Saunders/Elsevier; Philadelphia: pp. 577–584. 2010,
View Article : Google Scholar
|
|
13
|
Nguyen HT: Hernia, hydroceles, testicular
torsion, and varicocele. The Kelalis-King-Belman Textbook of
Clinical Pediatric Urology. Docimo SG, Canning DA and Khoury AE:
Informa Healthcare: London: pp. 1271–1293. 2007
|
|
14
|
Burgu B, Baker LA and Docimo SG:
Cryptorchidism. Pediatric Urology. Gearhart JP, Rink RC and
Mouriquand PDE: Saunders; Philadelphia: pp. 563–576. 2010,
View Article : Google Scholar
|
|
15
|
Luo CC and Chao HC: Prevention of
unnecessary contralateral exploration using the silk glove sign
(SGS) in pediatric patients with unilateral inguinal hernia. Eur J
Pediatr. 166:667–669. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Mollen KP and Kane TD: Inguinal hernia:
what we have learned from laparoscopic evaluation of the
contralateral side. Curr Opin Pediatr. 19:344–348. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Schier F, Danzer E and Bondartschuk M:
Incidence of contralateral patent processus vaginalis in children
with inguinal hernia. J Pediatr Surg. 36:1561–1563. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Rowe MI, Copelson LW and Clatworthy HW:
The patent processus vaginalis and the inguinal hernia. J Pediatr
Surg. 4:102–107. 1969. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Rathauser F: Historical overview of the
bilateral approach to pediatric inguinal hernias. Am J Surg.
150:527–532. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Lotan G, Efrati Y, Stolero S and Klin B:
Transinguinal laparoscopic examination: an end to the controversy
on repair of inguinal hernia in children. Isr Med Assoc J.
6:339–341. 2004.PubMed/NCBI
|
|
21
|
Bhatia AM, Gow KW, Heiss KF, et al: Is the
use of laparoscopy to determine presence of contralateral patent
processus vaginalis justified in children greater than 2 years of
age? J Pediatr Surg. 39:778–781. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Eller Miranda M and Duarte Lanna JC:
Videolaparoscopy of the contralateral internal inguinal ring via
the hernia sac in children with unilateral inguinal hernia-initial
experience in Brazil, with a meta-analysis. Pediatr Surg Int.
18:463–469. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Geisler DP, Jegathesan S, Parmley MC, et
al: Laparoscopic exploration for the clinically undetected hernia
in infancy and childhood. Am J Surg. 182:693–696. 2001. View Article : Google Scholar
|
|
24
|
Pavlovich CP, Gmyrek GA, Gardner TA, et
al: Flexible transinguinal laparoscopy to assess the contralateral
ring in pediatric inguinal hernias. Tech Urol. 4:141–144.
1998.PubMed/NCBI
|
|
25
|
Rescorla FJ, West KW, Engum SA, et al: The
‘other side’ of pediatric hernias: the role of laparoscopy. Am
Surg. 63:690–693. 1997.PubMed/NCBI
|
|
26
|
Zitsman JL: Transinguinal diagnostic
laparoscopy in pediatric inguinal hernia. J Laparoendosc Surg.
6(Suppl): S15–S20. 1996.PubMed/NCBI
|
|
27
|
Liu C, Chin T, Jan SE and Wei C:
Intraoperative laparoscopic diagnosis of contralateral patent
processus vaginalis in children with unilateral inguinal hernia. Br
J Surg. 82:106–108. 1995. View Article : Google Scholar : PubMed/NCBI
|