Introduction
Malignant hyperthermia following severe traumatic
brain injury occurs due to damage to the thermoregulatory centers,
occurring within the first three days after head trauma, a time
frame less likely for hyperthermia to be attributable to infectious
causes (1). Previous studies have
shown that malignant hyperthermia increases mortality and
disability in patients with brain trauma (1–5). In
brain damage such as stroke, hyperthermia acts through several
mechanisms to exacerbate cerebral ischemia (1), including the increased release of
neurotransmitters, excessive production of oxygen radicals,
extensive blood-brain barrier breakdown, increased ischemic
depolarizations in the focal ischemic penumbra, impaired recovery
of energy metabolism, enhanced inhibition of protein kinases and
worsening of cytoskeletal proteolysis (6,7).
Hyperthermia significantly increases the incidence of infection
(1) and elevates the intracranial
pressure, causing brain cell damage (4). Hyperthermia can increase the
metabolism of the body, accelerate organ failure and affect the
efficacy of neuroprotectant and thrombolytic therapy (8,9).
Therefore, the control of hyperthermia is necessary in the
treatment of traumatic brain injury. Therapeutic hypothermia has
become a focus of research in recent years.
Previous studies have shown that hypothermia can
reduce the basal metabolic rate, the consumption of oxygen by brain
cells (5,10) and intracranial pressure, and
protect the blood-brain barrier. Hypothermia has neuroprotective
effects (11), which involve
reduced extracellular glutamate release (12–14),
limited calcium transfer (15),
the reduction of free radicals (12), the inhibition of nitric oxide
(16,17) and reduced brain metabolism.
However, the lower the temperature, the greater the incidence of
side-effects and complications (18), such as shivering, reduced
electrolyte levels, dysregulated acid-base status, insulin
resistance, kidney dysfunction, arrhythmia and impaired immune
function. Currently, the temperature range of therapeutic
hypothermia remains controversial (14). A number of studies have described
the effects of moderate hypothermia (32–35°C); however, due to the
various complications (19),
difficulties in temperature maintenance and damage following
rewarming (20), the clinical
application of hypothermia is limited. Certain studies have
demonstrated that mild hypothermia can help to improve outcomes
(21,22) without clear explanation. Thus, it
is essential to balance the maximum efficacy and minimum
complications of therapeutic hypothermia. The aim of the present
study was to investigate a new therapeutic hypothermia method known
as ‘cool and quiet’ therapy for malignant hyperthermia in patients
following severe traumatic brain injury
Patients and methods
Patient selection
A total of 110 consecutive patients in the 88th
Hospital of PLA (Taian, China) with malignant hyperthermia
following severe traumatic brain injury were enrolled from June
2003 to June 2013. The patients had a Glasgow Coma Scale (GCS)
score of between 3 and 8 points, had spent >6 h in a coma after
injury, or experienced a deterioration of awareness following >6
h in a coma within 24 h after injury. Cases with serious
infections, dehydration fever, transfusion reactions, use of
psychotropic inhibitors or clinical brain death (GCS ≤3 and no
brain-stem reflexes) were excluded. In addition, 110 cases that had
undergone normothermia therapy, in which patients’ temperatures
were maintained between 36–37°C, were retrospectively analyzed as
the control. The present study was conducted according to the
revised Declaration of Helsinki (2008 edition), and the approval of
the ethical committee of the 88th Hospital of PLA was obtained.
Written informed consent was provided by all participants prior to
the study.
Patient assessment
Patients who met the entry criteria were examined by
a continuous CT scan, and the GCS was determined based on ability
of the patient to open their eyes, speak, and use their arms or
legs. Temperature measurement methods were as follows: As there are
numerous blood vessels around the rectum, which more sensitively
reflect changes in body temperature, rectal temperature
measurements were preferred. When using the retention enema, the
temperatures of the patients were measured orally.
Treatment protocol
On the basis of actively treating the primary
disease, all patients were treated with mild hypothermia (35–36°C)
in addition to small doses of sedative and muscle relaxant.
Basic treatment
On the basis of actively treating the primary
trauma, patients with severe cerebral edema, extensive cerebral
contusion and brainstem damage that were unconscious were treated
with the programmed cooling therapy as soon as possible. It was
maintained for 3–12 days, over the period at which trauma acute
reactions and edema peak. The therapy was administered in
combination with monitoring of the heart rate, blood pressure,
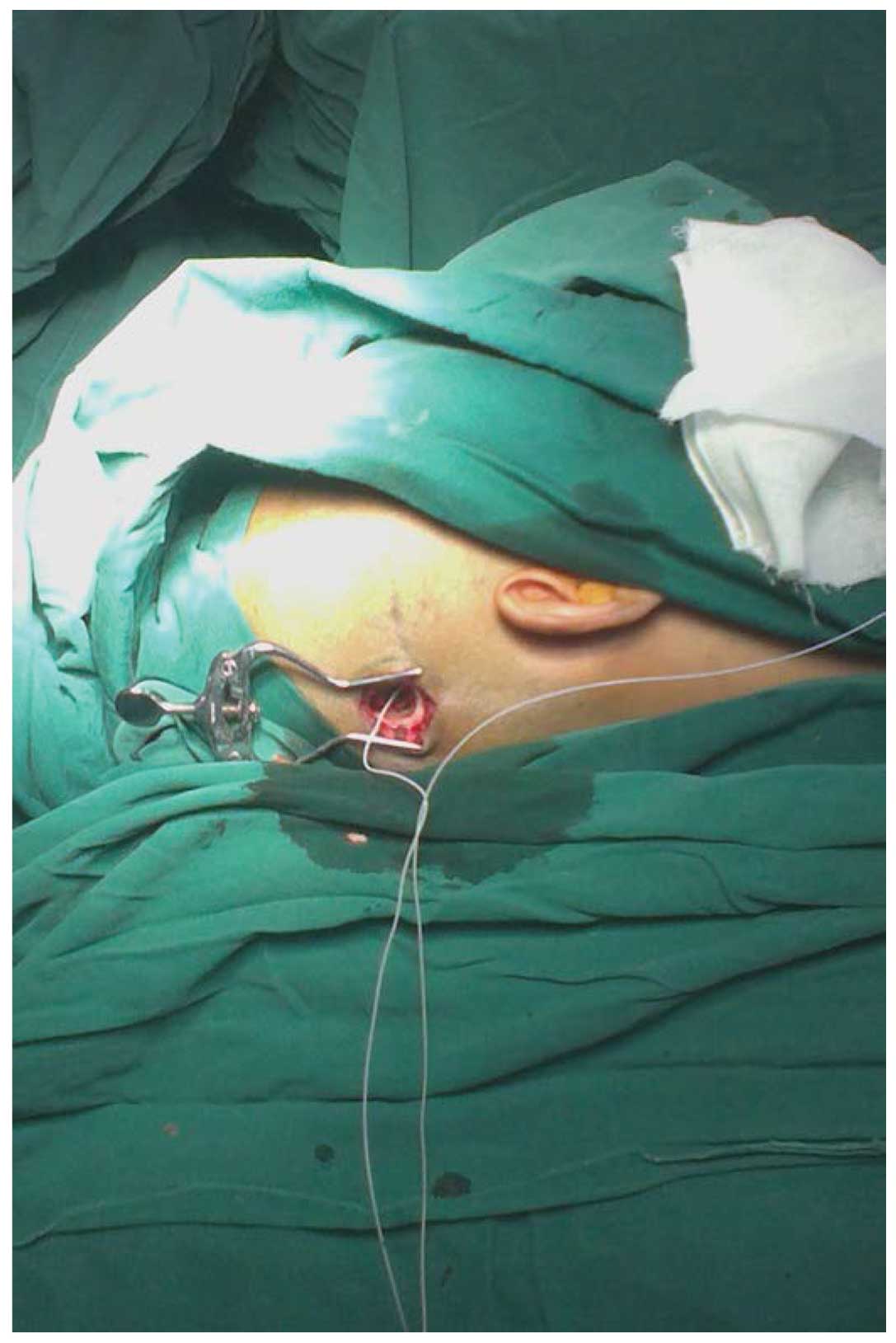
breathing and pulse. The invasive intracranial pressure (ICP) of 40
patients was monitored during surgery or through a probe placed
through a hole drilled in the skull (Fig. 1), with a Codman intracranial
pressure monitor (Codman Neuro, Raynham, MA, USA; Fig. 2) and intracranial pressure
sensor.
Mild hypothermia with physical
methods
Hypothermia instrument such as an ice blanket. The
efficacy of such a method was significant, and so was considered
first. The body temperature was set to 35–36°C and the water
temperature was set to 8–15°C. The room temperature was maintained
at 20–25°C. When the body temperature was higher than the maximum
of the set temperature, the water cycle started, which then took
heat away and lowered the body temperature.
Simple body surface hypothermia. The patient’s head
(with the exception of the face) was put in an ice cap or ice tank,
setting the temperature of the electronic ice cap at −2 to +2°C.
Concurrently, ice salt or chemical ice bags wrapped in a towel were
placed around both sides of the neck, armpits, groin and other
parts of the body with large vessels. Patients, with the exception
of those with brain herniation were given a retention enema with
500 ml cold saline and 1 g aspirin for 30 min. The temperature was
measured again 30 min after the retention enema and the retention
enema was repeated every 4–6 h. Through the above method, the
temperature was maintained at 35–36°C.
Sedative and muscle relaxant
To avoid shivering with skin reactions and to
eliminate the acute stress reaction of the body to the internal and
external environment, sedative and muscle relaxant administration
was carried out simultaneously with hypothermia. Patients with
increased intracranial pressure accompanied by restlessness, fever,
convulsions and decerebrate rigidity were treated with sedative and
muscle relaxant as early as possible.
Formula I (chlorpromazine, meperidine and
promethazine) was applicable to patients with a high fever and
dysphoria. This formula is recommended to be used with caution in
patients with respiratory failure and those younger than 1 year or
older than 60 years old. Formula II (chlorpromazine, promethazine
and hydergine) was used to treat patients in whom the hyperthermia
was accompanied by respiratory dysfunction or tachycardia. Formula
III (chlorpromazine, promethazine and procaine) was administered to
patients with oliguria. This formula is recommended to be used with
caution in patients with a slow heart rate or arrhythmia. Formula
IV (chlorpromazine and promethazine) was administered to patients
with relatively mild hyperthermia.
When selecting Formula I or II, it was necessary to
consider the condition of the patient. A full or half dose was
required to fully achieve the requirements at the first
administration, with physical cooling applied half an hour after
the administration of the sedative and muscle relaxant. The dose
was sufficient if patients did not undergo shivering with skin
reactions; if it was insufficient, additional medication was
administered. After this treatment, the temperature gradually
decreased. When the desired temperature was reached, the treatment
was transferred to the maintenance phase. Ice application was
reduced and alternative medication at a half to a third of the full
dose was administered every 4–8 h. Formula II was generally used as
an additional medication, since Formula I contained meperidine
which could cause inhibition of respiration.
The duration of hypothermia was 3–12 days, and
rewarming was carried out every 2–3 days. The temperature was
observed and therapeutic hypothermia was administered again if
necessary; in addition, if inhibition of respiration occurred due
to meperidine administration, the treatment was terminated. The
duration of the hypothermia was extended until the edema had gone
for patients with severe cerebral edema.
The rate of temperature lowering in adults was at
1–2°C/h, to the final temperature of 35–36°C, while that of
children was maintained at 2–3°C/h. Rapid cooling may cause
shivering and increase oxygen consumption, which should be avoided.
In certain cases, corticosteroids were used at an early stage to
protect the blood-brain barrier. Short-range high-dose shock
therapy was used, firstly with dexamethasone and
methylprednisolone. The dose of methylprednisolone was 5 mg/kg,
repeated every 6 h. The dose was decreased to 1 mg/kg after 24 h
and maintained for three days. Intrathecal medications were given
for hemorrhagic cerebrospinal fluid replacement once a day.
Hemorrhagic cerebrospinal fluid was slowly replaced at a volume of
30–50 ml each time. The cerebrospinal fluid turned clear in
approximately a week.
Statistical analysis
The Statistical Package for Social Sciences (SPSS,
Inc., Chicago, IL, USA), version 16.0 was used for data analysis.
Continuous variables are expressed as the mean ± standard
deviation, and categorical variables are expressed as proportions.
Comparisons between continuous variables were performed using
independent-samples t-test or variance analysis; comparisons
between categorical variables were performed by the χ2
test. P≤0.05 was considered to indicate a statistically significant
result.
Results
Characteristics of the patients
A total of 110 patients were enrolled in the study,
and the duration of hyperthermia ranged from 3 to 7 days. There
were 42 cases with hyperthermia within 12 h after injury and 68
cases within 24 h.
There were 73 cases with extensive cerebral
contusion including serious brain tissue swelling with obliteration
of the basal cisterns of the brain and fissures, 44 cases with
multiple intracranial hematoma, 71 cases with brainstem contusion
and hemorrhage, 26 cases with diffuse axonal injuries, 38 cases
with herniation, 85 cases with subarachnoid hemorrhage and 90 cases
with contrecoup injuries. In addition, there were 70 cases
requiring emergency craniotomy and hematoma surgery, including 34
cases with unilateral craniotomy, 35 cases with bilateral
craniotomy, and one case with removal of a hematoma in three parts
in three separate surgeries.
Outcomes
Of the 110 cases treated with mild hypothermia, 25
cases succumbed following a persistent fever of >40°C, and
certain cases were accompanied by severe complications, including
12 cases with acute renal function failure, 5 cases with
convulsions, 15 cases with gastrointestinal bleeding, 24 cases with
severe pulmonary infection, 13 cases with high blood sugar and 4
cases with pseudomembranous enteritis. A total of 85 cases
survived, including 13 cases of vegetative state, 12 cases with
living disability and 60 cases that were restored to a good state
of health. In the mild hypothermia group, the recovery rate was
54.5% and mortality rate was 22.7%. The severe and mild disability
rates were 11.8 and 10.9%, respectively.
The GCS scores and ICP data of the hypothermia group
showed no significant difference compared with those of the
normothermia group, (P>0.05; Tables
I and II). The mortality
rates of the patients in the hypothermia group and normothermia
group exhibited a significant difference (P=0.038; Table III). The mortality rates of
patients with GCS scores of between 3 and 5 revealed a
statistically significant difference between the two groups
(P=0.011; Table III). No
significant difference was observed in the mortality rates of
patients with GCS scores of between 6 and 8 between the two groups
(P>0.05; Table III).
 | Table IClinical observations of the two types
of therapy. |
Table I
Clinical observations of the two types
of therapy.
| | Prior to
treatment | Following
treatment |
|---|
| |
|
|
|---|
| Groups | Cases | T (°C) | GCS score | T (°C) | GCS score |
|---|
| Normothermia | 110 | 39.54±1.9 | 5.7±2.1 | 37.37±1.2 | 8.4±1.8 |
| Mild hypothermia | 110 | 39.62±1.6 | 5.5±1.9 | 37.73±1.6 | 8.7±1.5 |
 | Table IIICP statistics of the two types of
therapy. |
Table II
ICP statistics of the two types of
therapy.
| Groups | Cases | ICP prior to
treatment (mmHg) | ICP following
treatment (mmHg) |
|---|
| Normothermia | 40 | 26.8±17.5 | 12.3±8.5 |
| Mild hypothermia | 40 | 27.5±16.9 | 13.8±7.8 |
 | Table IIIMortality of patients with different
coma scores in the two groups. |
Table III
Mortality of patients with different
coma scores in the two groups.
| Initial GCS
group | Mild hypothermia | Normothermia | χ2 | P-value |
|---|
| All patients |
| Mortality, n
(%) | 25 (22.7)a | 39 (35.5) | 4.319 | 0.038 |
| Total, n | 110 | 110 | | |
| Patients with coma
scores of 3–5 |
| Mortality, n
(%) | 18 (40.9)a | 28 (68.3) | 6.409 | 0.011 |
| Total, n | 44 | 41 | | |
| Patients with coma
scores of 6–8 |
| Mortality, n
(%) | 7 (10.6) | 11 (15.9) | 0.831 | 0.362 |
| Total, n | 66 | 69 | | |
Discussion
During the clinical treatment, it was observed that
simply using head ice caps and ice bags on the surface of large
vessels, did not provide a satisfactory cooling effect. There were
four reasons: Unreasonably placed ice bags or caps, a limited
contact area and a gap between the cooling device and the skin
resulted in insufficient heat conduction; patients in a lateral
position had a reduced contact area with the ice blanket; the cold
stimulation exacerbated blood capillary contraction, which
decreased heat dissipation; and shivering caused by the cold
increased the production of heat. Therefore, it was considered
necessary to combine this treatment with other physical cooling
treatments.
A sponge bath using tepid water mixed with alcohol
was found to be a simple, safe and efficacious method. Not only
could the alcohol and water stimulate the capillaries in the skin
to dilate and increase the heat dissipation, but also evaporation
was able to take heat away. This could be used as a rapid
therapeutic method during the initial stage of stepwise
cooling.
The sedative and muscle relaxant were administered
to reduce cellular metabolism, block the acute stress response,
control muscle spasms and shivering, prevent convulsions and expand
peripheral vessels. The formulations used were unrestricted;
however, it is recommended that the dose and rate of administration
are strictly controlled. In the present study, three cases
experienced a sudden drop in blood pressure due to the intravenous
therapy being administered too rapidly. Due to the reduced heart
rate and blood pressure, low body temperature and weak breathing,
the medication was discontinued. No fatal complications such as
cardiac arrhythmia were observed during the cooling process and the
related nursing care was easy to carry out. With a lower mortality
rate compared with that of normothermia therapy, the mild
hypothermia therapy was demonstrated to be safe, convenient and
efficacious.
Short-range high-dose shock therapy with
corticosteroids (23,24) acts by stabilizing ion channels in
the cell membrane and promoting the outward flow of Ca2+
ions, thereby reducing phosphate kinase activity and cell
metabolism, which is conducive to the functional recovery of the
temperature regulating center. However, it is necessary to pay
attention to side-effects such as gastrointestinal bleeding
(25,26), glucose (27) and nitrogen metabolism disorders
(28) and immunosuppression
(29).
The initiation and duration times of hypothermia
remain controversial (5), due to
the different types and severities of traumatic brain injury. A
review of 13 clinical studies (30) found that treatment was started 6–22
h from onset and was maintained for an average of 40.9 h (range,
24–67 h). The mean duration in the present study was >7 days and
the longest case had a duration of 12 days; this patient awoke from
a coma 36 days after the injury and the brain function recovered
well.
Formula II of sedative and muscle relaxants was
found to be the optimum choice. Hydergine is able to expand blood
vessels, has a relatively low inhibitory effect on the respiratory
center and does not inhibit the adenosine triphosphate enzyme
system, which is beneficial to further regulate metabolism
disorders, ensure the effective circulating blood volume of the
heart, brain and kidneys and facilitate the recovery of central
nervous system functioning (31).
In conclusion, therapy using mild hypothermia
associated with sedative and muscle relaxant was beneficial in
reducing the mortality of patients with malignant hyperthermia
following severe traumatic brain injury, particularly in patients
with GSC scores of between 3 and 5 on admission. Due to the low
incidence of complications and ease of nursing care, the mild
hypothermia therapy was considered to be efficacious, safe and
convenient. However, a retrospective study was used to explore the
mild hypothermia therapy, without a randomized controlled trial.
Prospective rigorous randomized clinical trials are required to
provide evidence of the efficacy of ‘cool and quiet’ therapy in the
treatment of hyperthermia.
References
|
1
|
Li J and Jiang JY: Chinese Head Trauma
Data Bank: effect of hyperthermia on the outcome of acute head
trauma patients. J Neurotrauma. 29:96–100. 2012. View Article : Google Scholar :
|
|
2
|
Ginsberg MD and Busto R: Combating
hyperthermia in acute stroke: a significant clinical concern.
Stroke. 29:529–534. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Wang CX, Stroink A, Casto JM and Kattner
K: Hyperthermia exacerbates ischaemic brain injury. Int J Stroke.
4:274–284. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Cairns CJ and Andrews PJ: Management of
hyperthermia in traumatic brain injury. Curr Opin Crit Care.
8:106–110. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Childs C, Wieloch T, Lecky F, Machin G,
Harris B and Stocchetti N: Report of a consensus meeting on human
brain temperature after severe traumatic brain injury: its
measurement and management during pyrexia. Front Neurol. 1:1462010.
View Article : Google Scholar
|
|
6
|
Jiang JY, Gao GY, Li WP, et al: Early
indicators of prognosis in 846 cases of severe traumatic brain
injury. J Neurotrauma. 19:869–874. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Natale JE, Joseph JG, Helfaer MA and
Shaffner DH: Early hyperthermia after traumatic brain injury in
children: risk factors, influence on length of stay, and effect on
short-term neurologic status. Crit Care Med. 28:2608–2615. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Tokutomi T, Morimoto K, Miyagi T, et al:
Optimal temperature for the management of severe traumatic brain
injury: effect of hypothermia on intracranial pressure, systemic
and intracranial hemodynamics, and metabolism. Neurosurgery.
52:102–112. 2003.
|
|
9
|
Stiefel MF, Spiotta A, Gracias VH, et al:
Reduced mortality rate in patients with severe traumatic brain
injury treated with brain tissue oxygen monitoring. J Neurosurg.
103:805–811. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Dietrich WD and Bramlett HM: The evidence
for hypothermia as a neuroprotectant in traumatic brain injury.
Neurotherapeutics. 7:43–50. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Yokobori S, Frantzen J, Bullock R,
Gajavelli S, Burks S, Bramlett H and Dietrich WD: The use of
hypothermia therapy in traumatic ischemic/reperfusional brain
injury: review of the literatures. Ther Hypothermia Temp Manag.
1:185–192. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Globus MY, Alonso O, Dietrich WD, Busto R
and Ginsberg MD: Glutamate release and free radical production
following brain injury: effects of posttraumatic hypothermia. J
Neurochem. 65:1704–1711. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Maeda T, Katayama Y, Kawamata T and
Yamamoto T: Mechanisms of excitatory amino acid release in contused
brain tissue: effects of hypothermia and in situ administration of
Co2+ on extracellular levels of glutamate. J
Neurotrauma. 15:655–664. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Mori K, Maeda M, Miyazaki M and Iwase H:
Effects of mild (33 degrees C) and moderate (29 degrees C)
hypothermia on cerebral blood flow and metabolism, lactate, and
extracellular glutamate in experimental head injury. Neurol Res.
20:719–726. 1998.PubMed/NCBI
|
|
15
|
Mitani A, Kadoya F and Kataoka K:
Temperature dependence of hypoxia-induced calcium accumulation in
gerbil hippocampal slices. Brain Res. 562:159–163. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Chatzipanteli K, Wada K, Busto R and
Dietrich WD: Effects of moderate hypothermia on constitutive and
inducible nitric oxide synthase activities after traumatic brain
injury in the rat. J Neurochem. 72:2047–2052. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Sakamoto KI, Fujisawa H, Koizumi H,
Tsuchida E, Ito H, Sadamitsu D and Maekawa T: Effects of mild
hypothermia on nitric oxide synthesis following contusion trauma in
the rat. J Neurotrauma. 14:349–353. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Choi HA, Badjatia N and Mayer SA:
Hypothermia for acute brain injury - mechanisms and practical
aspects. Nat Rev Neurol. 8:214–222. 2012.PubMed/NCBI
|
|
19
|
Clifton GL, Miller ER, Choi SC, et al:
Lack of effect of induction of hypothermia after acute brain
injury. N Engl J Med. 344:556–563. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Clifton MG, Valadka PA, Aisuku IP and
Okonkwo DO: Future of rewarming in therapeutic hypothermia for
traumatic brain injury: a personalized plan. Ther Hypothermia Temp
Manag. 1:3–7. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Tokutomi T, Morimoto K, Miyagi T,
Yamaguchi S, Ishikawa K and Shigemori M: Optimal temperature for
the management of severe traumatic brain injury: effect of
hypothermia on intracranial pressure, systemic and intracranial
hemodynamics, and metabolism. Neurosurgery. 52:102–112. 2003.
|
|
22
|
Soukup J, Zauner A, Doppenberg EM, Menzel
M, Gilman C, Young HF and Bullock R: The importance of brain
temperature in patients after severe head injury: relationship to
intracranial pressure, cerebral perfusion pressure, cerebral blood
flow, and outcome. J Neurotrauma. 19:559–571. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Dearden NM, Gibson JS, McDowall DG, Gibson
RM and Cameron MM: Effect of high-dose dexamethasone on outcome
from severe head injury. J Neurosurg. 64:81–88. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Cooper PR, Moody S, Clark WK, Kirkpatrick
J, Maravilla K, Gould AL and Drane W: Dexamethasone and severe head
injury. A prospective double-blind study. J Neurosurg. 51:307–316.
1979. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Piek J, Chesnut RM, Marshall LF, et al:
Extracranial complications of severe head injury. J Neurosurg.
77:901–907. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Halloran LG, Zfass AM, Gayle WE, Wheeler
CB and Miller JD: Prevention of acute gastrointestinal
complications after severe head injury: a controlled trial of
cimetidine prophylaxis. Am J Surg. 139:44–48. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Jeremitsky E, Omert LA, Dunham CM,
Wilberger J and Rodriguez A: The impact of hyperglycemia on
patients with severe brain injury. J Trauma. 58:47–50. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Clifton GL, Robertson CS, Grossman RG,
Hodge S, Foltz R and Garza C: The metabolic response to severe head
injury. J Neurosurg. 60:687–696. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Mayumi H, Zhang QW, Nakashima A, Masuda M,
Kohno H, Kawachi Y and Yasui H: Synergistic immunosuppression
caused by high-dose methylprednisolone and cardiopulmonary bypass.
Ann Thorac Surg. 63:129–137. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Groysman LI, Emanuel BA, Kim-Tenser MA,
Sung GY and Mack WJ: Therapeutic hypothermia in acute ischemic
stroke. Neurosurg Focus. 30:E172011. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Geffroy A, Bronchard R, Merckx P, Seince
PF, Faillot T, Albaladejo P and Marty J: Severe traumatic head
injury in adults: which patients are at risk of early hyperthermia?
Intensive Care Med. 30:785–790. 2004. View Article : Google Scholar : PubMed/NCBI
|