Introduction
Methicillin-resistant Staphylococcus aureus
(MRSA)-induced infections, accounting for >50% of staphylococcal
diseases, have increased rapidly in recent years (1). MRSA is considered to be one of the
most common antibiotic-resistant pathogens causing invasive
infections (2). In the last
decade, epidemiologic studies have illustrated that MRSA-induced
infections have changed from being primarily acquired in hospitals
to also being acquired in the community (3). Between 1999 and 2005, the estimated
number of MRSA infections more than doubled in the United States
(4). This increase was largely
attributed to skin and soft-tissue infections, which are commonly
caused by community-associated MRSA (CA-MRSA) (4).
Prostatic abscess is a rare disease due to the
widespread use of broad-spectrum antibiotics in patients with lower
urinary tract symptoms (LUTS) (5).
It is mainly identified in patients with predisposing factors,
including chronic indwelling catheters, invasion of the lower
urinary tract, diabetes mellitus, human immunodeficiency virus
infection and other causes of compromised immunity (6). In the past, prostatic abscesses were
primarily caused by Neisseria gonorrhoeae and
Staphylococcus aureus. At present, gram-negative bacteria,
particularly Escherichia coli, are the dominant pathogens in
the development of prostatic abscess (5). With the elevated risk of CA-MRSA, a
great emphasis is put on its pathogenicity in prostatic abscess
(7). Seminal vesicle abscess
mostly results from concurrent prostatic abscess. Few cases have
been reported since the first case in 1978 when Machida et
al reported the first case of spermatic cord abscess with
concurrent prostatic abscess involving the seminal vesicle
(8).
To the best of our knowledge, the present study is
the first to describe the use of ultrasound perfusion imaging and
traditional computed tomography (CT) to diagnose a patient with
CA-MRSA prostate abscess involving the seminal vesicle, which was
subsequently treated with adjuvant antibiotics and transrectal
ultrasonography (TRUS)-guided prostate needle aspiration. Written
informed consent was obtained from the patient for publication of
this case report and the accompanying images.
Case report
A 42-year-old male presented to the outpatient
clinic of the First Affiliated Hospital of Zhejiang University
School of Medicine (Hangzhou, China) with 2 weeks of severe dysuria
and pain in the abdomen. The patient had been complaining of
urination difficulty and dribbling for 4 years, but reported no
nocturia, hematuria, fever or chills. The patient then went to the
local hospital. Ultrasonography revealed a 5.6×3.9-cm abnormal
echogenic mass in the prostate, which was considered to be an
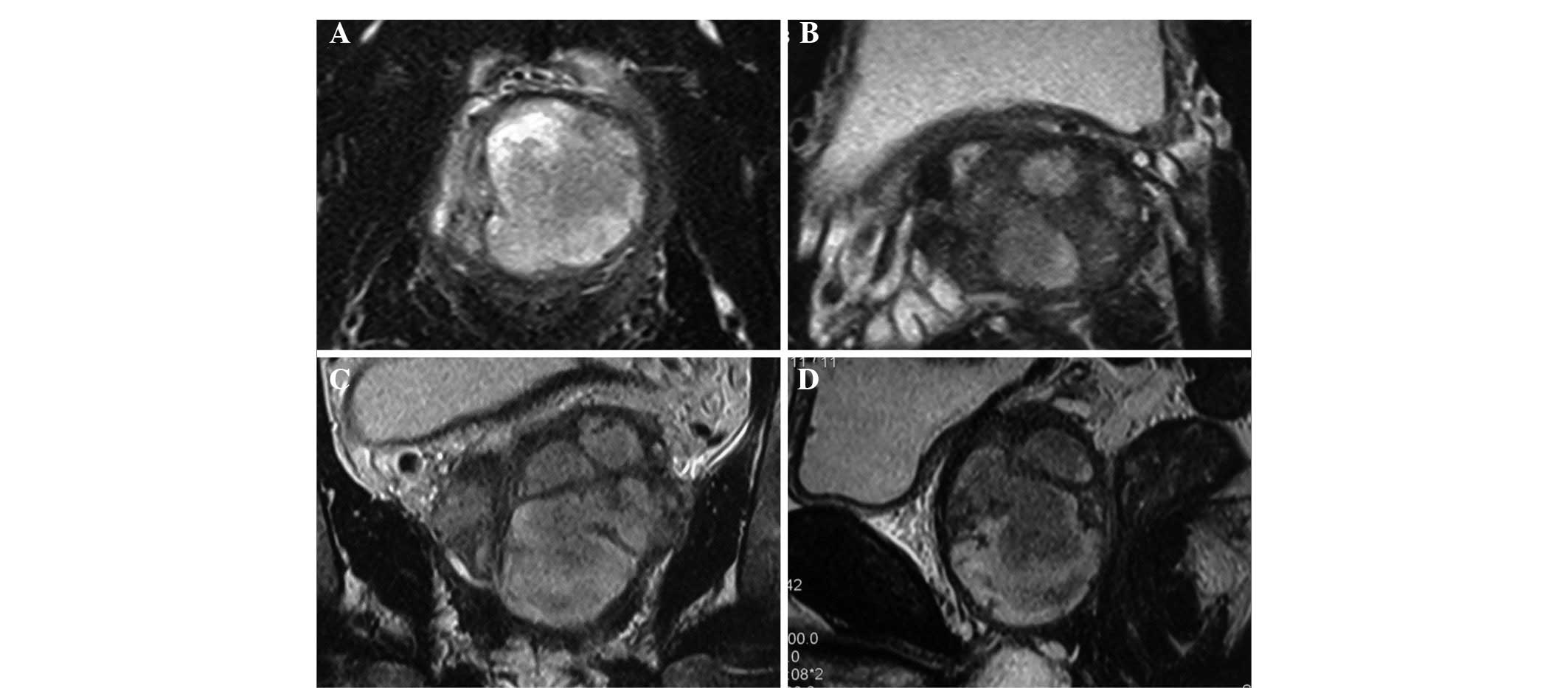
inflammatory mass. Magnetic resonance imaging (MRI) exhibited
abnormal signals in the prostate and left seminal vesicle,
indicating the presence of prostate abscesses involving the seminal
vesicle (Fig. 1). Blood
examinations revealed an elevated blood glucose level (18.62
mmol/l), and urine analysis demonstrated an elevated microscopic
white cell count and the presence of glucose. Therefore, the
patient was diagnosed with prostate abscesses involving the seminal
vesicle, urine retention and diabetes mellitus (type 2). An
indwelling catheter and anti-inflammatory and hypoglycemic therapy
were administered in the local hospital. Eight days later, the
catheter was removed. However, the patient continued to present
with dysuria and odynuria. The patient also complained of
constipation and persistent pain around the anus at this time. No
significant past medical history was identified. Physical
examination was remarkable due to the observation of an enlarged
prostate, with tenderness.
Subsequently, the patient was admitted to the
Department of Urology, First Affiliated Hospital of Zhejiang
University School of Medicine, where a series of examinations were
conducted. Urine culture grew Candida albicans that was
sensitive to fluconazole. Glycosylated hemoglobin analysis showed
an elevation in glycosylated hemoglobin A1 (12.0%) and glycosylated
hemoglobinA1c (10.5%) levels. The examination of a urine smear for
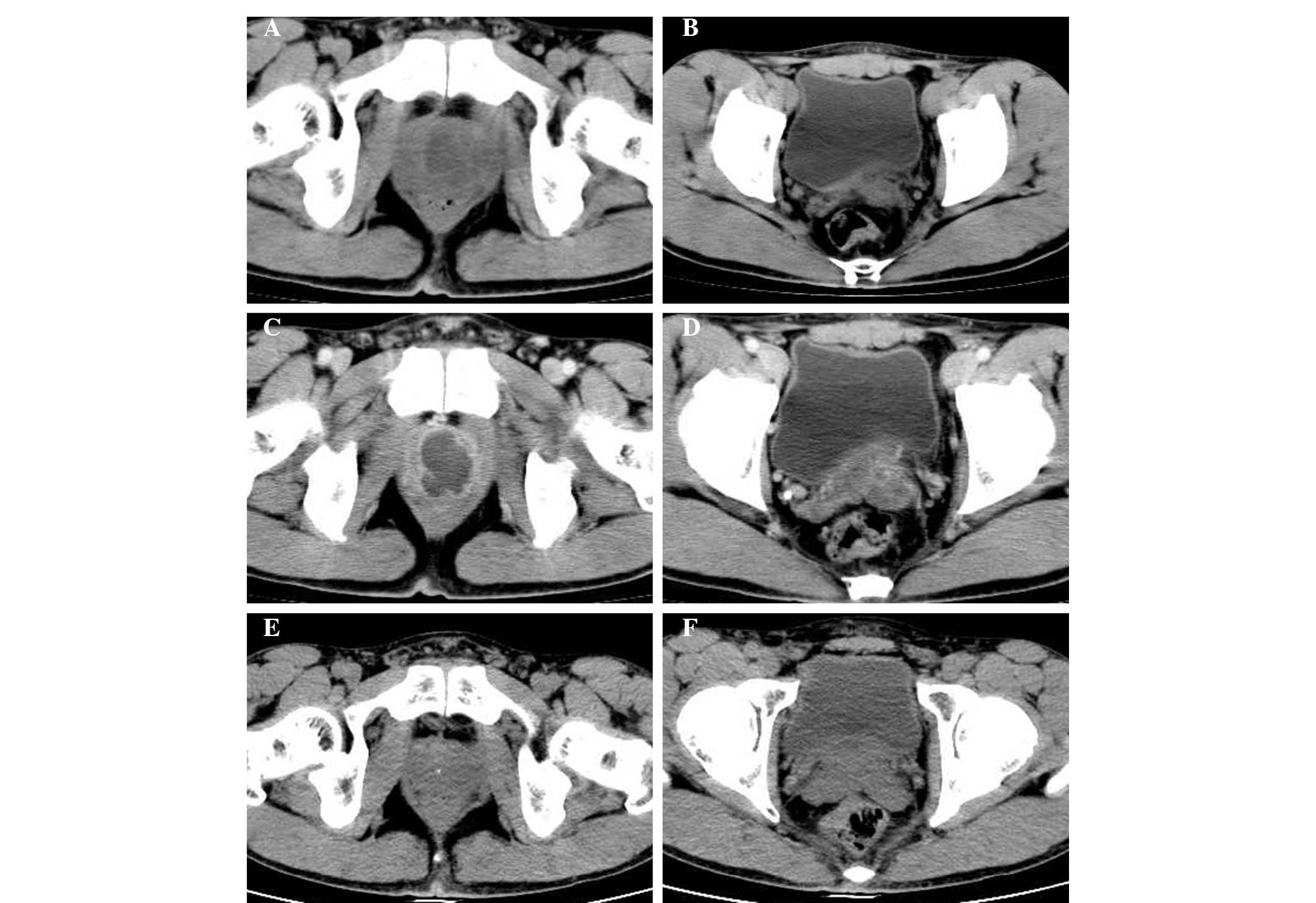
Mycobacterium tuberculosis exhibited a negative result. CT
of the pelvis demonstrated that there were multiple prostate
abscesses, involving the left seminal vesicle (Fig. 2A–D). Transabdominal ultrasonography
revealed multi-hypoechogenic masses in the prostate, which were
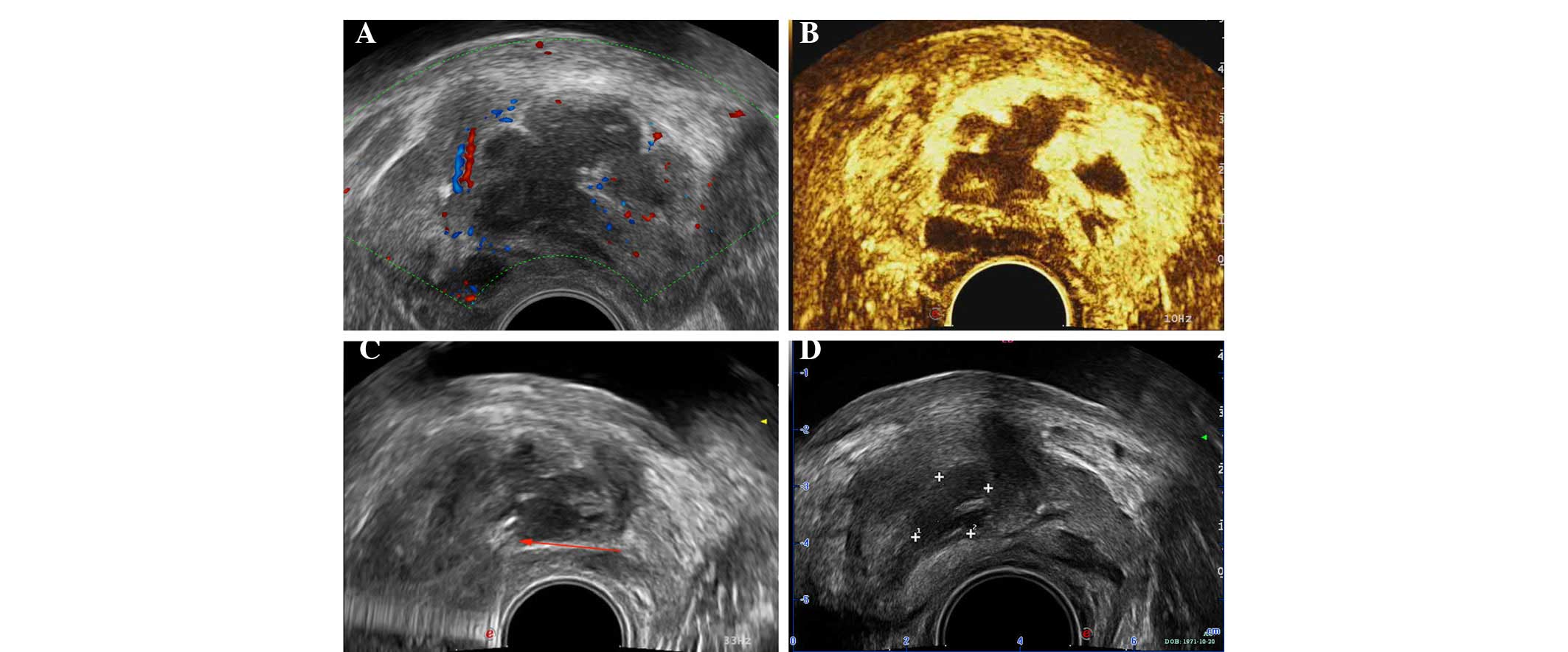
considered to be abscesses. Transrectal ultrasonography was also
conducted, which revealed similar results (Fig. 3A). Transrectal ultrasound perfusion
imaging illustrated no enhancement in the hypoechogenic area and
irregular fluid dark space of the prostate (Fig. 3B).
Therefore, the patient received levofloxacin,
metronidazole and fluconazole for a total of 3 days before
transrectal prostate puncture was performed (Fig. 3C). A total of 17 ml purulent fluid
was extracted. Purulent fluid culture grew MRSA (sensitive to all
antibiotics with the exception of penicillin, oxacillin and
erythromycin), and levofloxacin and metronidazole were given for
another 2 days prior to withdrawal. The patient was reexamined by
transrectal ultrasonography, which revealed a great improvement in
the prostate, with a 1.6×1.0-cm hypoechogenic area (Fig. 3D). The result of a C-reactive
protein test was normal at 3.10 mg/l. The patient was discharged
the next day.
A follow-up CT scan and ultrasonography 1 month
after the initial presentation revealed a marked improvement in the
prostate and the symptoms were greatly improved (Fig. 2E and F).
Discussion
Prostatic abscess is considered to be an uncommon
disease due to the widespread use of broad-spectrum antibiotics in
patients with LUTS (5).
Nevertheless, accurate diagnosis and treatment remain of great
importance due to the possibility of progression to sepsis and
mortality (9). Prostatic abscess
is challenging to diagnose due to its non-specific signs, symptoms
and physical examination findings, including fever, chills, urinary
frequency, dysuria, acute urinary retention (AUR) or lower back
pain, which is easily misdiagnosed as acute bacterial prostatitis
(10). Imaging examination such as
transrectal ultrasonography (TRUS), CT and MRI is critical for
accurate diagnosis. TRUS can be applied as an initial examination
and easily make a diagnosis of prostatic abscess. CT of the pelvis
and abdomen area brings no extra pain to patients, and can help to
confirm the scope of infection in the adjacent organs (11).
Seminal vesicle abscess usually results from
concurrent prostatic abscess. The diagnosis is commonly made by CT
or TRUS. The CT characteristics of a seminal vesicle abscess
include: i) enlargement of the seminal vesicle unilaterally or
bilaterally; ii) an area of low attenuation in the seminal vesicle;
iii) inflammatory alterations in surrounding fat; and iv)
thickening of the bladder wall focally or diffusely (12).
Ultrasound contrast can enhance the visualization of
perfusion changes associated with prostate cancer, and is regarded
as a promising tool in distinguishing between benign prostatic
hyperplasia and prostate cancer (13,14).
To the best of our knowledge, the present study is the first to
report the use of ultrasound perfusion imaging and traditional CT
to diagnose a patient with CA-MRSA prostate abscess involving the
seminal vesicle. In this case, transrectal ultrasound perfusion
imaging exhibited no enhancement in the hypoechogenic area and
irregular fluid dark space of the prostate.
Treatments of prostatic abscess have changed greatly
in recent years. Surgeries such as perineal incision or
transurethral resection were traditionally recommended as the
first-line therapy (15). By
contrast, minimally invasive treatments such as TRUS-guided needle
aspiration transrectally or transperineally under local anesthesia
are more popular at present. Becker et al first reported
that needle aspiration and adjuvant antibiotic therapy could
achieve a superior therapeutic efficacy (16). Thereafter, many studies were
conducted to evaluate the efficacy of needle aspiration (9,17–19).
Gan suggested that TRUS-guided needle aspiration is a feasible
alternative to traditional transurethral drainage (17). Collado et al reported that a
combination of TRUS-guided needle aspiration and adjuvant
antibiotic therapy was effective in the treatment of prostatic
abscess (18). Aravantinos et
al and Lim et al demonstrated similar results in the
treatment of prostatic abscess via TRUS-guided needle aspiration
(9,19). In the present case, a 42-year-old
diabetic male with CA-MRSA prostate abscess involving the seminal
vesicle was successfully treated via adjuvant antibiotics and
TRUS-guided prostate needle aspiration.
Prostatic abscess involving the seminal vesicle is a
rare disease with potential risk of mortality if the appropriate
treatment is not administered, and thus deserves considerable
attention. Ultrasound perfusion imaging plays an important role in
diagnosing prostatic abscess involving the seminal vesicle. In the
present case, early treatment with appropriate antibiotics and
TRUS-guided needle aspiration of the prostatic abscess resulted in
a shorter hospital stay, and lower risk of local recurrence and
mortality.
Acknowledgements
The study was supported by grants from the National
Key Clinical Specialty Construction Project of China, Key Medical
Disciplines of Zhejiang Province, Combination of Traditional
Chinese and Western Medicine Key Disciplines of Zhejiang Province
(2012-XK-A23), the Health Sector Scientific Research Special
Project (201002010) and the Scientific Research Foundation of the
Ministry of Publica Health (2012-KY1-001-155).
References
|
1
|
Klevens RM, Morrison MA, Nadle J, Petit S,
Gershman K, Ray S, Harrison LH, Lynfield R, Dumyati G, Townes JM,
et al; Active Bacterial Core surveillance (ABCs) MRSA
Investigators. Invasive methicillin-resistant Staphylococcus aureus
infections in the United States. JAMA. 298:1763–1771. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Dantes R, Mu Y, Belflower R, Aragon D,
Dumyati G, Harrison LH, Lessa FC, Lynfield R, Nadle J, Petit S, et
al: Emerging Infections Program-Active Bacterial Core Surveillance
MRSA Surveillance Investigators: National burden of invasive
methicillin-resistant Staphylococcus aureus infections, United
States, 2011. JAMA Intern Med. 173:1970–1978. 2013.PubMed/NCBI
|
|
3
|
Klein EY, Sun L, Smith DL and Laxminarayan
R: The changing epidemiology of methicillin-resistant
Staphylococcus aureus in the United States: a national
observational study. Am J Epidemiol. 177:666–674. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Klein E, Smith DL and Laxminarayan R:
Hospitalizations and deaths caused by methicillin-resistant
Staphylococcus aureus, united states, 1999–2005. Emerg Infect Dis.
13:1840–1846. 2007. View Article : Google Scholar
|
|
5
|
Weinberger M, Cytron S, Servadio C, Block
C, Rosenfeld JB and Pitlik SD: Prostatic abscess in the antibiotic
era. Rev Infect Dis. 10:239–249. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Granados EA, Riley G, Salvador J and
Vincente J: Prostatic abscess: diagnosis and treatment. J Urol.
148:80–82. 1992.PubMed/NCBI
|
|
7
|
Naboush A, Abou Yassine A, Yasmin M and
Mobarakai N: Community-acquired methicillin-resistant
Staphylococcus aureus prostatic abscess presenting as acute urinary
retention: a case report and review of the literature. Case Rep
Infect Dis. 2013:7617932013.PubMed/NCBI
|
|
8
|
Machida H, Ueno E, Nakazawa H, Fujimura M
and Ito F: Spermatic cord abscess with concurrent prostatic abscess
involving the seminal vesicle. Radiat Med. 26:81–83. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Aravantinos E, Kalogeras N, Zygoulakis N,
Kakkas G, Anagnostou T and Melekos M: Ultrasound-guided transrectal
placement of a drainage tube as therapeutic management of patients
with prostatic abscess. J Endourol. 22:1751–1754. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Oliveira P, Andrade JA, Porto HC, Filho JE
and Vinhaes AF: Diagnosis and treatment of prostatic abscess. Int
Braz J Urol. 29:30–34. 2003. View Article : Google Scholar
|
|
11
|
Thornhill BA, Morehouse HT, Coleman P and
Hoffman-Tretin JC: Prostatic abscess: CT and sonographic findings.
AJR Am J Roentgenol. 148:899–900. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kang YS, Fishman EK, Kuhlman JE and
Goldman SM: Seminal vesicle abscesses: spectrum of computed
tomographic findings. Urol Radiol. 11:182–185. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Frauscher F, Pallwein L, Klauser A, Berger
AP, Koppelstaetter F, Gradl J, Schurich M, Bektic J, Pinggera GM,
Halpern EJ, et al: Ultrasound contrast agents and prostate cancer.
Radiologe. 45:544–551. 2005.(In German). View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zhao HX, Xia CX, Yin HX, Guo N and Zhu Q:
The value and limitations of contrast-enhanced transrectal
ultrasonography for the detection of prostate cancer. Eur J Radiol.
82:e641–e647. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Dajani AM and O’Flynn JD: Prostatic
abscess. A report of 25 cases. Br J Urol. 40:736–739. 1968.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Becker LE and Harrin WR: Prostatic
abscess: a diagnostic and therapeutic approach. J Urol. 91:582–585.
1964.PubMed/NCBI
|
|
17
|
Gan E: Transrectal ultrasound-guided
needle aspiration for prostatic abscesses: an alternative to
transurethral drainage? Tech Urol. 6:178–184. 2000.PubMed/NCBI
|
|
18
|
Collado A, Palou J, Garcia-Penit J,
Salvador J, de la Torre P and Vicente J: Ultrasound-guided needle
aspiration in prostatic abscess. Urology. 53:548–552. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Lim JW, Ko YT, Lee DH, Park SJ, Oh JH,
Yoon Y and Chang SG: Treatment of prostatic abscess: value of
transrectal ultrasonographically guided needle aspiration. J
Ultrasound Med. 19:609–617. 2000.PubMed/NCBI
|