Introduction
Extrapulmonary tuberculosis (TB) refers to TB
involving the extrapulmonary organs of the body. Extrapulmonary TB
accounts for 9.7–11.9% of all TB cases in China, while the
mortality rate caused by extrapulmonary TB accounts for 14.1–17.6%
of the total TB mortalities (1). A
variety of signs and symptoms occur depending on the different
lesion sites. The lesion sites in extrapulmonary TB are scattered
and the detection rate of Mycobacterium tuberculosis (M.
tuberculosis) in the lesions is low. Therefore, the condition
of the patients with extrapulmonary TB is complicated and
frequently overshadowed by other illnesses, thereby having a big
impact on diagnosis and treatment. Functional lesions in local
organs often cause disabilities and even endanger lives due to
missed diagnosis, misdiagnosis and the lack of normative guidance
on treatment protocols (2).
Chest wall TB is a common form of TB on the surface
of the body, and includes TB lesions found in the ribs, sternum and
soft tissue of the chest wall, which are secondary to pulmonary or
pleural TB infection. The area of the lesions is large and the
majority of lesions eventually appear as cold abscesses and ulcers,
which lead to sinus tract or ulcer-induced fistulas (3). When a diagnosis is clinically
confirmed, the abscesses are already formed and even ruptured, or
the sinuses are formed. Treatment methods comprise oral anti-TB
therapy combined with surgery. Although the local blood vessels of
the TB lesions are damaged, the lymph nodes have intact capsules
that are difficult for the TB drugs to penetrate, and a number of
tubercle bacilli are contained within the lymph nodes (4). As the systemic anti-TB drugs are
unable to penetrate into the lymph nodes, it is difficult for the
tissue drug concentration to reach the effective bactericidal
concentration required. Following oral administration of anti-TB
drugs, achieving an effective concentration of the drug in the
local lesions is difficult; thus, the intended antibacterial
effects and sterilization cannot be realized. In addition, surgical
treatment may cause large trauma, and requires combined
intravenous-inhalation anesthesia. Certain patients are unable to
tolerate these conditions, and even if the surgery is a success,
the patient is left with a large surgical scar (5).
Sonophoresis technology is a type of
transdermal-targeted drug delivery technology, whereby the drugs
penetrate the tissue through the skin under the action of
ultrasonic waves (6). The nature
of biological tissues is that of a closed circuit, and sonophoresis
applies high-frequency electromagnetic fields to produce a
cavitation effect, which causes the arrangement of the stratum
corneum lipid bilayer to become disordered and promotes transdermal
drug penetration. A superimposed effect of multiple technologies is
achieved through system integration, in order for the programed
targeted drug delivery to be realized. The sonophoresis mode for
transdermal drug delivery is able to reduce drug degradation in the
liver, stabilize the plasma drug concentration and prevent drug
degradation in the digestive tract. Thus, the tissue cell
permeability is enhanced and the drug absorption is increased
within a short period of time (6).
In the present study, sonophoresis technology was
applied in the treatment of TB on the body surface. Anti-TB drugs
were administered to the lesions by ultrasonic waves to enable the
local lesions to have a higher blood drug concentration compared
with the rest of the body, solving the problem of a lower local
effective drug concentration. The effective control of TB was
consequently assessed by analyzing the improved, cure and efficacy
rates. The present study also investigated the role of transdermal
ultrasound technology in preventing certain patients from requiring
general anesthesia surgery, improving the efficacy of non-surgical
treatment and reducing the requirement rate for surgery.
Materials and methods
General information
A total of 186 patients were recruited from the
Second Department of Thoracic Surgery of Beijing Chest Hospital
(Beijing, China) between August 2009 and August 2011. The patients
selected for the present study were those with chest wall TB who
were treated initially and found to have no rifampicin resistance
following a Löwenstein-Jensen medium test. The patients were
randomly divided into the transdermal ultrasound, surgery and oral
anti-TB drug only groups. There were 62 newly-diagnosed patients in
the transdermal ultrasound group (male, 34; female, 28; age range,
13–78 years; mean age, 39 years). The largest and smallest chest
wall TB abscesses in this group were 12.0×10.0 cm and 3.0×1.5 cm,
respectively. In total, 12 patients were diagnosed with pulmonary
TB, while the remaining 50 patients had chest wall TB. The surface
surgery treatment group included 62 newly-diagnosed patients with
TB (male, 38; female, 24; age range, 17–47 years; mean age, 28.5
years). Of these, 11 patients had pulmonary TB and 51 patients were
diagnosed with chest wall TB.
There were 62 newly-diagnosed patients in the oral
anti-TB drug only group (male, 41; female, 21 females; age range,
19–71 years; mean age, 43.5 years). In total, eight patients were
diagnosed with pulmonary TB, while the remaining 54 patients had
chest wall TB. The present study was approved by the Ethics
Committee of Capital Medical University, (Beijing, China); written
informed consent was obtained from each patient prior to their
participation.
Oral anti-TB drug treatment
The transdermal ultrasound treatment, surgery and
oral medication only groups adopted the HREZ anti-TB treatment
program, which included isoniazid (H; 300 mg administered orally
once per day; Shanxi Yunpeng Pharmaceutical Co., Ltd., Linfen,
China), rifampicin (R; 450 mg administered orally once per day;
Chongqing Yaoyou Pharmaceutical Co., Ltd., Chongqing, China),
ethambutol (E; 750 mg administered orally once per day; Chengdu
Jinhua Pharmaceutical Co., Ltd., Chengdu, China) and pyrazinamide
(Z; 500 mg administered orally three times per day; Chengdu Jinhua
Pharmaceutical Co., Ltd.,). Patients in the oral medication only
and transdermal ultrasound groups received anti-TB drugs for 12
months. Patients undergoing surgery received preoperative oral
medication for one month prior to surgery and postoperative anti-TB
medication for 11 months following surgery. The surgical procedure
included tube drainage and debridement of the affected area.
Transdermal ultrasound treatment
Rifampicin was the transdermal ultrasound-delivered
drug. Initially, the patient’s skin was disinfected with
povidone-iodine. Based on the Löwenstein-Jensen medium sensitivity
test results (only patients without rifacampin resistance were able
to take part in ultrasound treatment) a 4×4 cm single piece of
cotton dipped in rifampicin solution [5 ml injectable rifampicin
aqueous solution (0.3 g)] was spread on the tuberculous abscess.
The drug was delivered using an ultrasound transdermal instrument
(Beijing Noah Tongzhou Medical Technology Co., Ltd., Beijing,
China) for 30 min, with the ultrasound intensity adjusted based on
the depth of the lesion (measured by ultrasound). The drug patch
remained in place for an additional 1–2 h following each treatment
to ensure adequate absorption of the drug.
Determination of efficacy
The transdermal ultrasound and oral medication only
groups were examined by chest B-mode ultrasonography or computed
tomography (CT) two months following treatment to confirm the
complete disappearance of TB without the appearance of new lesions.
Patients were assigned to the: cured category, if there was a full
subcision without new lesions; efficacy category, if a size
reduction of >60% was observed without new lesions; or
improvement category, if a size reduction of >30% and occasional
new lesions were observed. The efficacy rate was determined for the
cure and efficacy groups. The patients in the surgery group were
assessed by chest B-mode ultrasonography and chest CT as part of
their routine clinical assessment.
Case inclusion and exclusion
criteria
Patients were included in the study if they met the
following criteria: Aged ≥20 years; diagnosed with latent TB by a
cervical neck biopsy; treatment-naive with no evidence of a
significant cardiac disease; tolerance to ultrasound therapy; and
no known allergy to rifampicin.
The exclusion criteria were as follows: Aged <20
years; diagnosed with active pulmonary TB; undergoing cervical
lymph node TB retreatment; known allergy to rifampicin; and
presence of a significant congenital heart disease that would make
ultrasound treatment difficult to tolerate.
Follow-up period
The follow-up period was 12 months following the
transdermal ultrasound treatment, oral anti-TB therapy or
surgery.
Statistical analysis
SPSS 13.0 software (SPSS, Inc., Chicago, IL, USA)
was used to analyze the experimental data. Results from the
transdermal ultrasound, oral treatment only and surgery groups were
compared using the χ2 test. P<0.05 was considered to
indicate a statistically significant difference.
Results
Outcome of the transdermal ultrasound
treatment group
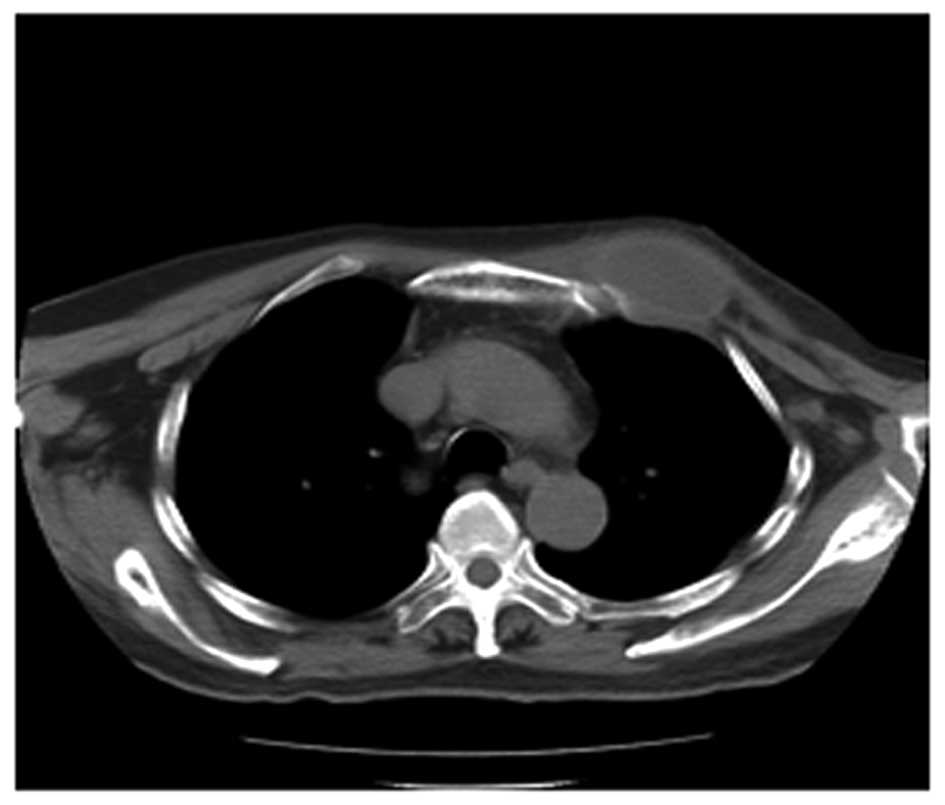
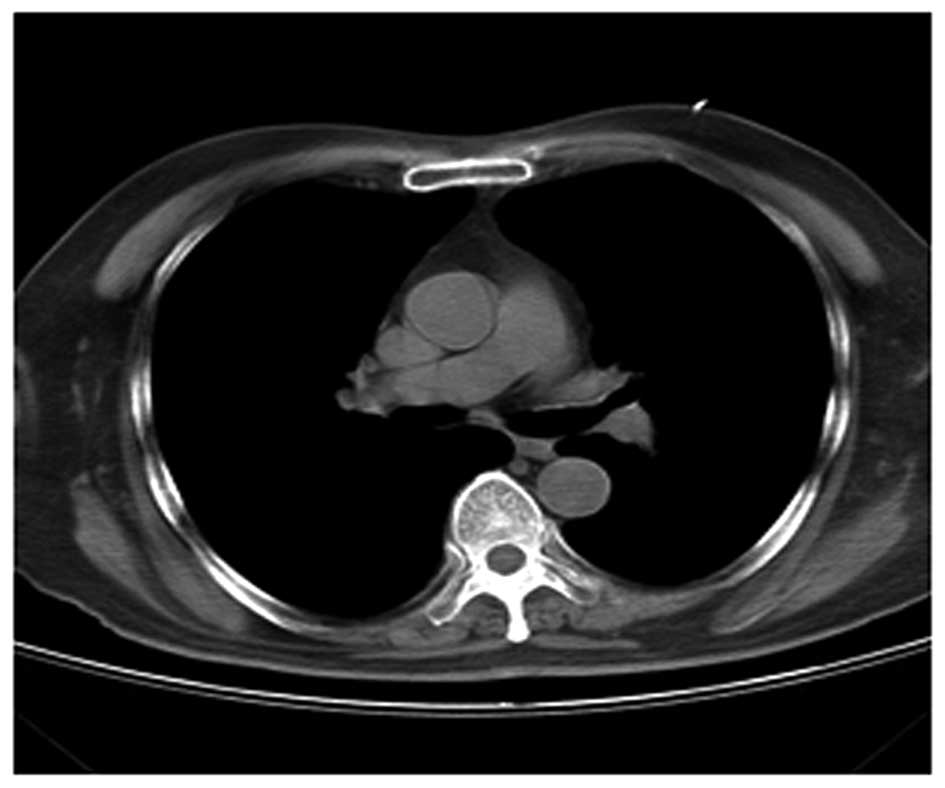
Within the transdermal ultrasound treatment group,
54/62 patients were completely cured, with four patients showing
efficacy and two patients showing improvement. The two patients who
did benefit from the treatment were hospitalized two weeks later
and subsequently discontinued the treatment. The cure rate was
87.10% and the efficiency rate was 93.55% (Figs. 1–4; chest CT scans).
Outcome of the surgical treatment
group
Within the surgery group, 56/62 patients were cured,
with four relapses and two patients that suffered from incision
wounds that did not heal. As recurrences were observed in four
patients, the cure rate was 90.32%. The efficacy rate was not
determined in the surgery group it is known to have a high rate of
effectiveness (7) and the aim of
the present study was to focus on non-invasive treatment
options.
Outcome of the oral drug therapy
group
Within the oral drug treatment only group, 12/62
patients were cured. A total of 14 patients were classified into
the efficacy category, while eight patients demonstrated marked
improvement; 28 patients did not show any improvement. The cure
rate was 19.35% and the efficiency rate was 41.93%.
Statistical significance
No statistically significant difference was observed
in the cure rate between the transdermal ultrasound and surgery
groups (Table I). However, a
statistically significant difference was identified in the cure
rate between the transdermal ultrasound and oral drug only groups
(Table II). The cure and
efficiency rates were significantly higher in the transdermal
ultrasound group when compared with the oral treatment only group
(Table III).
 | Table ICure rate comparison between the
transdermal ultrasound and surgery groups. |
Table I
Cure rate comparison between the
transdermal ultrasound and surgery groups.
| Group (n) | Total cases (n) | Cured cases (%) | Cure rate |
|---|
| Transdermal
ultrasound | 62 | 54 | 87.10 |
| Surgery | 62 | 56 | 90.32 |
| P-value | - | - | 0.57 |
 | Table IICure rate comparison between the
transdermal ultrasound and oral medication only groups. |
Table II
Cure rate comparison between the
transdermal ultrasound and oral medication only groups.
| Group | Total cases (n) | Cured cases (n) | Cure rate (%) |
|---|
| Transdermal
ultrasound | 62 | 54 | 87.10 |
| Oral medication | 62 | 12 | 19.35 |
| P-value | - | - | <0.01 |
 | Table IIIEfficacy rate comparison between the
transdermal ultrasound and oral medication only groups. |
Table III
Efficacy rate comparison between the
transdermal ultrasound and oral medication only groups.
| Group | Total cases (n) | Efficacy cases
(n) | Efficacy rate
(%) |
|---|
| Transdermal
ultrasound | 62 | 58 | 93.55 |
| Oral medication | 62 | 26 | 41.93 |
| P-value | | | <0.01 |
Discussion
TB is a chronic infectious disease caused by M.
tuberculosis. According to World Health Organization
statistics, ~1/3 of the world population is infected with M.
tuberculosis (1). Of the TB
cases and TB mortalities, 95 and 98%, respectively, occur in
developing countries. The TB infection rate in China is 44.5%, with
an estimated 550 million individuals infected with M.
tuberculosis (1,8).
The majority extrapulmonary TB cases are the result
of a lung infection by M. tuberculosis. The incidence rate
of extrapulmonary TB is an important contributor to the TB
epidemic. Although extrapulmonary TB accounts for only 10% of the
total number of TB cases, the infection can exist in numerous parts
of the body with different infection routes and symptoms. As a
result, the diagnoses, examination methods and treatments also
differ (9).
Body surface TB includes chest wall TB and lymphatic
TB, the two of which are common types of extrapulmonary TB. Chest
wall TB is the most common type of chest wall disease, particularly
among individuals aged <30 years (10,11).
Typical symptoms of chest wall TB include abscesses and chronic
sinus formation (12), which are
often secondary to lung, pleura or mediastinal TB. The majority of
patients do not experience symptoms or have mild pain, although
abscesses may rupture spontaneously or eventually form chronic open
sinuses.
Since chest wall TB exhibits no clinical symptoms in
the majority of patients with the early form of the disease, chest
wall TB frequently has multiple variants and affects a large
percentage of the population (13). When chest wall TB is diagnosed,
abscesses and sinuses have already formed or ruptured. Since blood
vessels adjacent to the chest wall TB area are damaged and M.
tuberculosis resides within the lymph nodes (lymph nodes have
intact membranes), it is difficult for anti-TB drugs to achieve an
effective concentration in the system. Therefore, systemic
treatment with anti-TB drugs often does not achieve desirable
results and long-term anti-TB drug treatment is frequently combined
with surgery (14,15). Surgical treatment is able to
completely remove the necrotic lesions and M. tuberculosis.
However, since chest wall TB can affect multiple locations, the
surgical approach may be difficult. Surgical procedures for chest
wall TB vary based on the condition of the patient, and often
require a rib resection and a muscle flap (16). Such surgeries generally require
intravenous anesthesia and endotracheal intubation, and the
affected area is significant. Thus, elderly patients and patients
in a poor physical condition are often unable to tolerate surgery.
During surgery, the lesions must be thoroughly cleaned, along with
the removal of all the tuberculous tissue. In addition to the
surgical removal of the skin and subcutaneous soft tissue, a rib
resection, partial thoracoplasty, clavicle resection and a
pleurectomy are performed. The wound is subsequently bandaged and
compressed for a long period of time, and poor healing may often
lead to early infection. Due to the large postoperative skin damage
and slow-healing of the wounds, tension reduction or free flap
incisions are often used, which can cause serious and unsightly
scars (3,17).
The recurrence rate from chest wall TB surgery is
high. Although there have been significant improvements in
preoperative diagnosis, debridement and surgical techniques, due to
the low concentration of anti-TB drugs in the tuberculous area and
the poor tolerance of oral anti-TB drugs by certain patients, the
recurrence rate of TB remains at 7–8% (12). The high recurrence rate also
reflects other factors, including the residual TB tissue, patients
with diabetes and drug-resistant TB strains. In certain cases,
complete curative effects are difficult to achieve even following
multiple surgeries; thus, chest wall TB is a debilitating
disease.
Transdermal ultrasound-mediated drug delivery is a
targeted drug delivery technology. The technique takes advantage of
the principle of high-frequency electromagnetic fields and the
closed-circuit nature of biological tissues to deliver a drug
quickly and directly toward the diseased areas, increasing tissue
cell permeability (18). Since
skin functions as a natural barrier, the majority of drugs, even
low-dose, highly efficacious drugs, are unable to permeate the skin
sufficiently to meet the treatment requirements. Thus, overcoming
the skin barrier and promoting drug penetration to achieve a
therapeutic transdermal concentration is one of the key challenges
in transdermal drug delivery research (19,20).
Electromagnetic field effects have been demonstrated to activate
drug activity and efficacy (21).
The drug is introduced into the body without damage to the skin,
pain, gastrointestinal irritation or other side-effects. Currently,
significant progress has been made to use ultrasound-mediated
physical therapy to increase the sensitivity of localized
chemotherapy and radiation in the treatment of cancer, alleviate
pain from cancer and improve the synergy between frozen and heat
therapy (22,23). However, to the best of our
knowledge, the present study introduced transdermal
ultrasound-mediated anti-TB drug delivery for the treatment of
chest wall TB for the first time. The outcome was superior to that
of oral anti-TB only treatment, and the procedure did not require
surgical intervention for a number of patients.
In conclusion, the current study demonstrated that
transdermal ultrasound technology may be applied for the treatment
of body surface TB. Ultrasonography quickly and directly delivered
the anti-TB drugs to the diseased area and achieved a high local
plasma concentration. The transdermal ultrasound method overcame
the low local drug concentration problem and was demonstrated to be
an effective method to control TB. As a result, a number of
patients may no longer have to undergo surgery with general
anesthesia. The efficacy of this new method was significantly
improved compared with the administration of oral anti-TB drugs
only. Therefore, transdermal ultrasound-mediated drug delivery
provides an important non-surgical therapeutic option for patients
with chest wall TB.
Acknowledgements
The study was supported by a grant from the Beijing
Municipal Science and Technology Commission (no. Z121107001012065)
as part of the Capital Characteristic Clinical Application Research
project.
References
|
1
|
Gupta R, Espinal MA and Raviglione MC:
Tuberculosis as a major global health problem in the 21st century:
a WHO perspective. Semin Respir Crit Care Med. 25:245–253. 2004.
View Article : Google Scholar
|
|
2
|
Golden MP and Vikram HR: Extrapulmonary
Tuberculosis: an overview. Am Fam Physician. 72:1761–1768.
2005.PubMed/NCBI
|
|
3
|
Gaude GS and Reyas A: Tuberculosis of the
chest wall without pulmonary involvement. Lung India. 25:135–137.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Grosset J: Mycobacterium tuberculosis in
the extracellular compartment: an underestimated adversary.
Antimicrob Agents Chemother. 47:833–836. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Mitragotri S, Edwards DA, Blankschtein D
and Langer R: A mechanistic study of ultrasonically-enhanced
transdermal drug delivery. J Pharm Sci. 84:697–706. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Packer JL, Krall B and Torabinejad M: The
effect of sonophoresis on topical anesthesia: a pilot project.
Anesth Prog. 60:37–41. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kuzucu A, Soysal O and Günen H: The role
of surgery in chest wall tuberculosis. Interact Cardiovasc Thorac
Surg. 3:99–103. 2004. View Article : Google Scholar
|
|
8
|
Kurth R and Haas WH: Epidemiology,
diagnostic possibilities, and treatment of tuberculosis. Ann Rheum
Dis. 61(Suppl 2): ii59–ii61. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Sia IG and Wieland ML: Current concepts in
the management of tuberculosis. Mayo Clin Proc. 86:348–361. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Sharma SK and Mohan A: Extrapulmonary
tuberculosis. Indian J Med Res. 120:316–353. 2004.PubMed/NCBI
|
|
11
|
Smith I: Mycobacterium tuberculosis
pathogenesis and molecular determinants of virulence. ClinMicrobiol
Rev. 16:463–496. 2003.
|
|
12
|
Gözübüyük A, Ozpolat B, Gürkök S, et al:
Surgical management of chest wall TB. J Cutan Med Surg. 13:33–39.
2009.
|
|
13
|
Keum DY, Kim JB and Park CK: Surgical
treatment of a tuberculous abscess of the chest wall. Korean J
Thorac Cardiovasc Surg. 45:177–182. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Deng B, Tan QY, Wang RW, et al: Surgical
strategy for tubercular abscess in the chest wall: experience of
120 cases. Eur J Cardiothorac Surg. 41:1349–1352. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Tanaka S, Aoki M, Nakanishi T, et al:
Retrospective case series analysing the clinical data and treatment
options of patients with a tubercular abscess of the chest wall.
Interact Cardiovasc Thorac Surg. 14:249–252. 2012. View Article : Google Scholar :
|
|
16
|
Zhang N, Xu QZ, Fu XN and Sun W: Use of a
pedicled omental flap in the treatment of chest wall TB. Ann Thorac
Surg. 93:1010–1012. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lim SY, Pyon JK, Mun GH, Bang SI and Oh
KS: Reconstructive surgical treatment of tuberculosis abscess in
the chest wall. Ann Plast Surg. 64:302–306. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Lavon I, Grossman N and Kost J: The nature
of ultrasound-SLS synergism during enhanced transdermal transport.
J Control Release. 107:484–494. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Simonetti LD, Gelfuso GM, Barbosa JC and
Lopez RF: Assessment of the percutaneous penetration of cisplatin:
the effect of monoolein and the drug skin penetration. Eur J Pharm
Biopharm. 73:90–94. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Dubey V, Mishra D and Jain NK: Melatonin
loaded ethanolic liposomes: physicochemical characterization and
enhanced transdermal delivery. Eur J Pharm Biopharm. 67:398–405.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Funk RH, Monesees T and Ozkucur N:
Electromagnetic effects - From cell biology to medicine. Prog
Histochem Cytochem. 43:177–264. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Schoellhammer CM, Polat BE, Mendenhall J,
et al: Rapid skin permeabilization by the simultaneous application
of dual-frequency, high-intensity ultrasound. J Control Release.
163:154–160. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Polat BE, Figueroa PL, Blankschtein D and
Langer R: Transport pathways and enhancement mechanisms within
localized and non-localized transport regions in skin treated with
low-frequency sonophoresis and sodium lauryl sulfate. J Pharm Sci.
100:512–529. 2011. View Article : Google Scholar :
|