Introduction
Blastic plasmacytoid dendritic cell neoplasm (BPDCN)
is a rare neoplasm, previously termed as blastic natural killer
(NK)-cell lymphoma. BPDCN is included in the acute myeloid leukemia
(AML) category of the latest World Health Organization (WHO)
classification of tumors (1).
BPDCN often involves the skin, lymph nodes, peripheral blood and
bone marrow. Blast cells are generally found to be positive for
CD4, CD56 and CD123 in patients with BPDCN (2). The disease is not sensitive to
traditional chemotherapy treatment, and the median survival time is
~12–14 months (1). ETS variant
gene 6 (ETV6) gene-involved chromosomal translocations have been
observed in numerous hematological malignancies (3). Several studies exist on BPDCN;
however, to the best of our knowledge, BPDCN with ETV6
rearrangement has not been previously reported. Initially, BPDCN
usually affects the skin and then involves the lymph nodes and bone
marrow, ultimately proliferating in the peripheral blood (4,5).
BPDCN has numerous characteristics that are similar to leukemia.
Thus, lumbar punctures and preventive intrathecal chemotherapy are
indispensable measures for the treatment of acute leukemia patients
in the remission stage. Lumbar punctures and preventive intrathecal
chemotherapy may be required in BPDCN patients with leukemia
manifestation during the remisson stage. In the present study, a
case of BPDCN with leukemic manifestation without cutaneous
involvement was reported.
Case report
A 48-year-old male, who was previously healthy, was
admitted to the Affiliated Hospital of Binzhou Medical University
Hospital (Binzhou, China) in December 2012, due to experiencing
left cervical lymphadenopathy for two months. Physical examination
revealed a number of superficial lymphadenopathies and
splenomegaly. The patient did not present hepatomegaly or skin
lesions. In a preliminary blood test, the patient was found to have
a hemoglobin level of 12.8 g/dl, white blood cell count of
2.8×109/l, platelet count of 129×109/l and
erythrocyte sedimentation rate of 33 mm/h. No abnormalities were
observed in the liver function and biochemical assays, while blood
coagulation and urine tests were found to be unremarkable. In
addition, a human immunodeficiency virus antibody test was
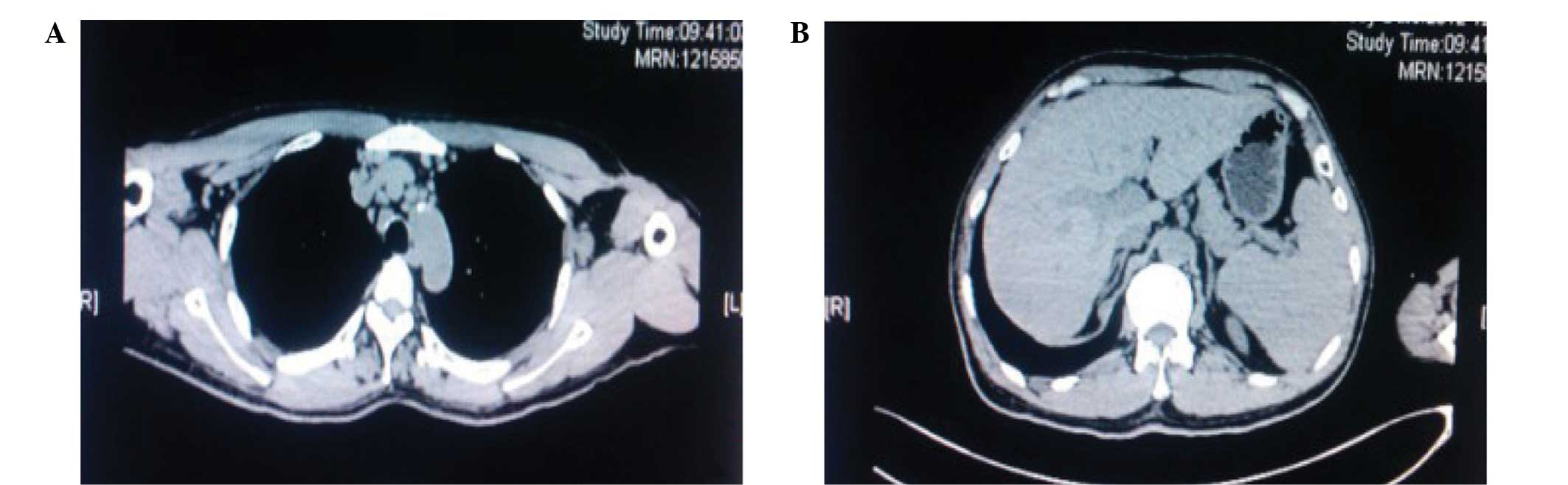
negative. Computed tomography (CT) scans of the chest and abdomen
revealed splenomegaly and multiple deep lymphadenopathies (Fig. 1).
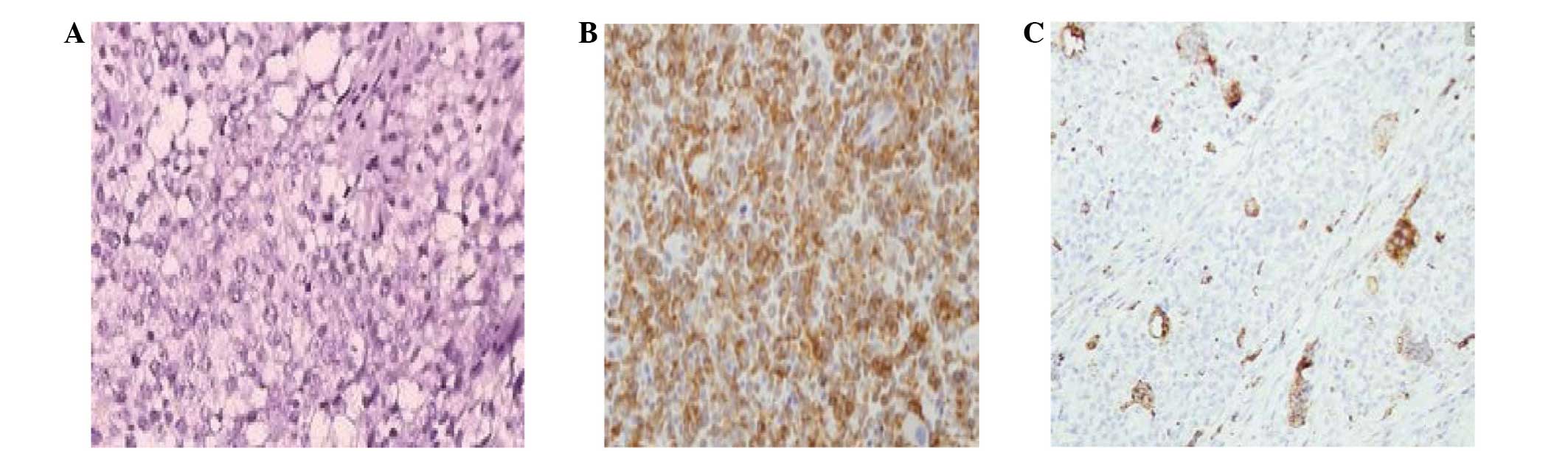
Lymph node biopsy revealed that the normal lymph
node structure was destroyed and replaced by an abnormal diffuse
infiltration of lymphocytes. Immunohistochemical staining revealed
that the infiltrated lymphocytes were CD43, CD123 and CD68-positive
(Fig. 2), a small scattering of
cells were positive for CD20 and 40% of cells were Ki-67-positive.
However, the cells were found to be CD10 and terminal
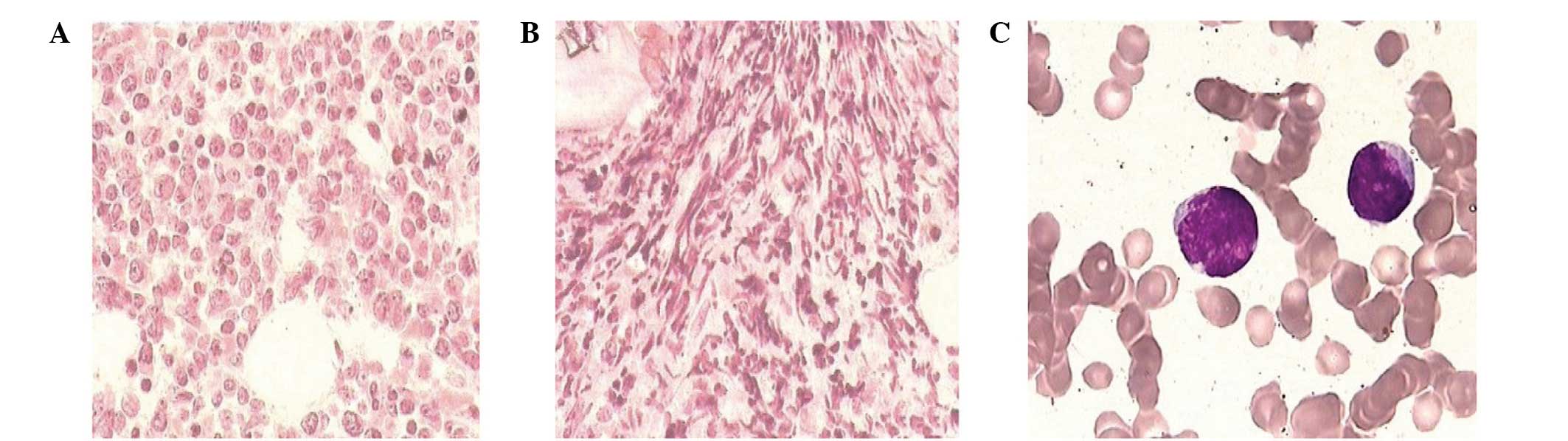
deoxynucleotidyl transferase (TdT)-negative. Bone marrow aspiration
analysis demonstrated that the blast cells consisted of 52%
mononuclear cells and had variable sizes, agranular cytoplasm and
irregular nuclei (Fig. 3). Bone
marrow biopsy revealed hypercellularity with diffuse infiltration
of tumor cells, accompanied by evident hyperplasia of fibrous
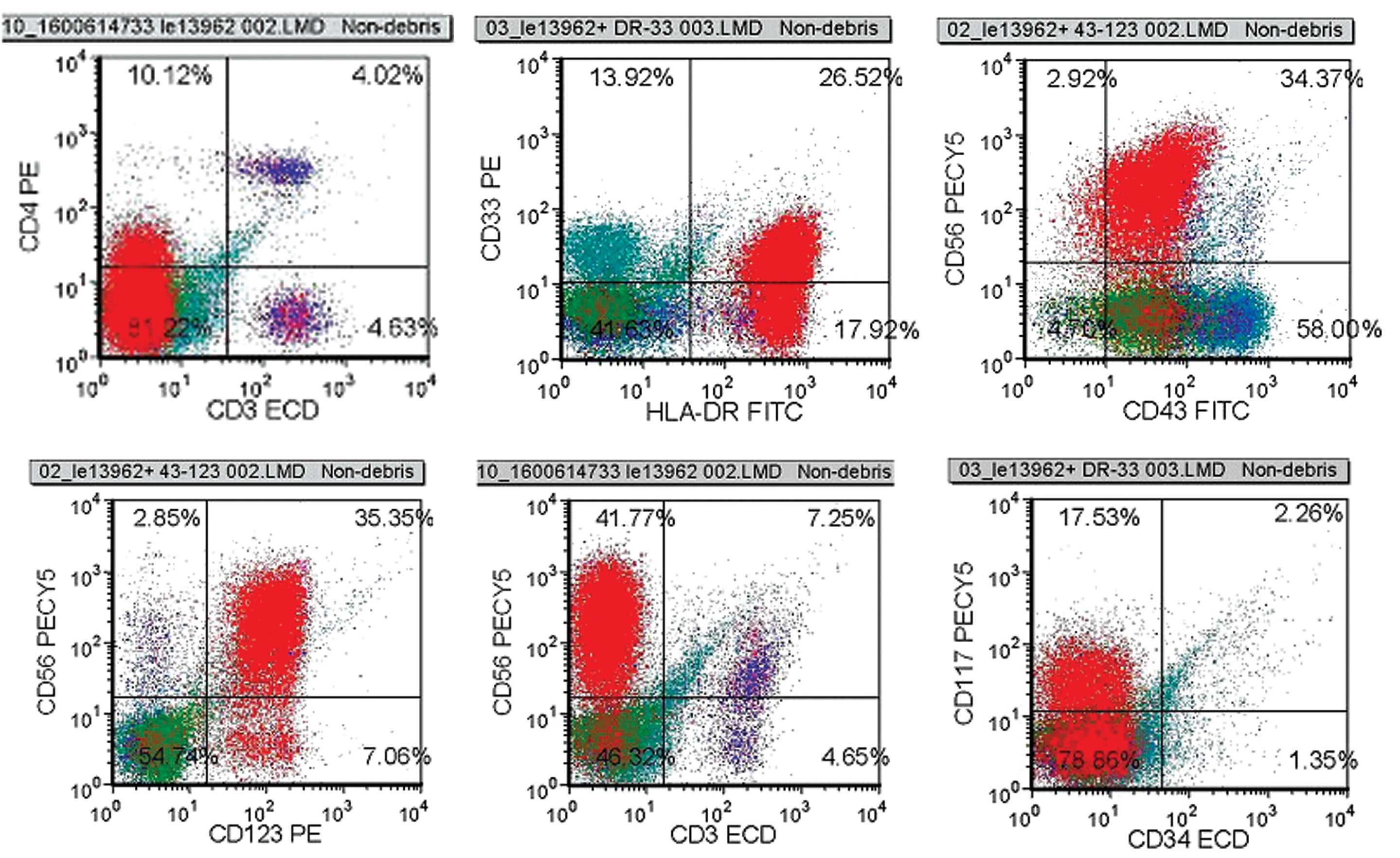
tissue. Flow cytometric analysis of the bone marrow revealed the
following cellular characteristics: CD4+,
CD56+, CD117+, CD33+,
HLA-DR+, CD43+, CD123+ (Fig. 4), CD34−,
MPO−, CD36−, CD64−,
CD303−, CD304−, CD19−,
CD10−, CD20−, CD38−,
CD138−, CD13− and TdT−.
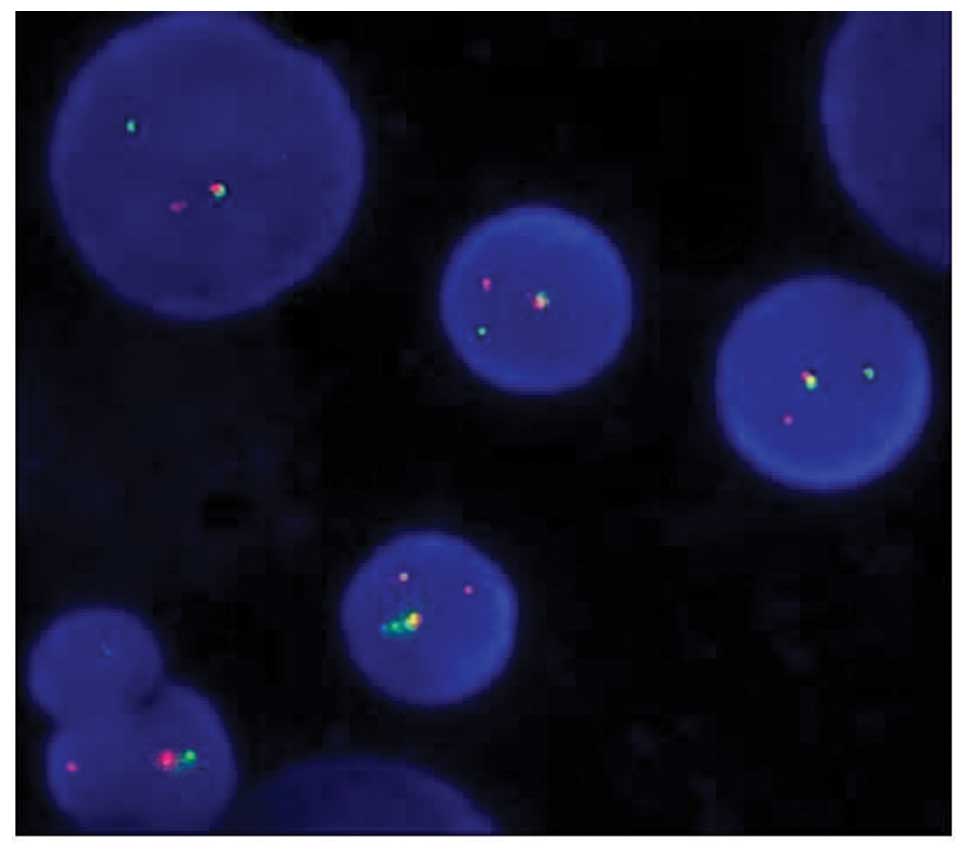
Traditional R-banding cytogenetic analysis did not detect any
further chromosome abnormalities. The marrow sample was further
probed using split-signal fluorescence in situ hybridization
(FISH), which identified the rearrangement of ETV6 (Fig. 5). T-cell receptor gene
rearrangement was not detected. Diagnosis of BPDCN was conclusive,
based on the aforementioned findings. Notably, the blast cells were
found to be positive for CD33 and CD117, which are myeloid
leukemia-associated antigens.
Initially, the patient was treated with the VDCP
regimen (vincristine: 2 mg, i.v. drip, days 1, 8, 15 and 22;
daunorubicin: 40 mg, i.v. drip, days 1–3 and 15–17;
cyclophosphamide: 1 g, i.v. drip, days 1 and 15; and prednisone: 60
mg, p.o., days 1–14, decrement from day 15) (6). Following the intensive chemotherapy
treatment, the proportion of tumor cells decreased from 52 to 3.5%.
The patient suffered from severe headache in the complete remission
stage; however, brain CT scans showed no significant abnormalities.
Subsequently, several lumbar punctures and intrathecal chemotherapy
(cytarabine, methotrexate and dexamethasone) were performed, and
the patient recovered gradually. However, three weeks after the
treatment period, the tumor cells rapidly increased. Thus, the
patient was treated with the MEVP regimen (mitoxantrone: 10 mg,
i.v. drip, days 1–3, etoposide: 100 mg, i.v. drip, days 1–5;
vincristine: 2 mg, i.v. drip, days 1 and 8; and prednisone 60 mg,
p.o., days 1–14) (6), followed by
the HAD regimen (homoharringtonine: 3 mg, i.v. drip, days 1–5;
cytarabine: 150 mg, i.v. drip, days 1–5; and daunorubicin: 40 mg,
i.v. drip, days 1–3) (7),
according to the immune phenotype (CD33+, CD117+ and HLA-DR+). The
treatment had no effect on the tumor growth and the patient
succumbed to severe pulmonary infection seven months after the
diagnosis. The present study was approved by the Ethics Committee
of the Binzhou Medical University Hospital. Informed consent was
obtained from the patient’s family prior to participation in the
current study.
Discussion
BPDCN is a rare and highly aggressive hematologic
malignancy that involves plasmacytoid dendritic cell precursors.
The nomenclature of this disease has evolved over time. In 1994,
the disease was first identified as blastic NK cell
lymphoma/leukemia by Adachi et al (5). In 2005, the WHO-European Organization
for Research and Treatment of Cancer identified the disease as a
CD4+/CD56+ hematodermic neoplasm due to its
derivation from a plasmacytoid dendritic cell precursor (4). The term BPDCN was enlisted in the
2008 WHO classification of hematopoietic and lymphoid tissue tumors
(1). BPDCN frequently involves the
skin, lymph nodes, peripheral blood and bone marrow.
Histopathologically, BPDCN is characterized by a diffuse,
monomorphous infiltrate of medium-sized blastic cells with
irregular nuclei, fine chromatin and one-to-several small nucleoli
(5). The first manifestation of
the disease is often cutaneous involvement. The majority of
patients present skin involvement, while a number of cases with
only skin involvement have been reported (8). The present study presents a rare case
of leukemic manifestation with lack of skin involvement. To date,
few such cases have been studied worldwide (9). To the best of our knowledge, the
present study is the first reported case of BPDCN with leukemic
involvement and lack of skin involvement in China. Notably, the
possibility of central nervous system involvement during the
development of BPDCN was observed. Therefore, prevention of central
nervous system leukemia in patients suffering from the reported
BPDCN type is necessary in the complete remission stage.
BPDCN is characterized by a medium-sized, dense
monomorphous infiltration with a blastoid morphology (5), typically expressing CD4, CD56, CD43,
CD45RA, CD123, BDCA-2/CD303 and TCL1 antigens. The expression of
CD56 has been rarely found to be negative. In addition, BPDCNs
usually lack most myeloid antigens; thus, CD117 and CD33-positve
BPDCNs are extremely rare. The expression of CD68 is normally
negative in BPDCNs, whereas a positive CD68 expression indicates
that the BPDCN may be transformed into acute or chromic leukemia
and particularly monocytic leukemia. In the present case, lymph
node immunohistochemical staining revealed a small scattering of
cells positive for CD68, which may be one of the reasons for the
leukemic transformation.
ETS variant gene 6 (ETV6), mapped to 12p13, is an
ETS family transcription factor that is essential in hematopoietic
processes (3). ETV6 gene-involved
chromosomal translocations have been detected in numerous
hematological malignancies characterized by fusion with a number of
partner genes. ETV6 mainly codes for tyrosine kinases or
transcription factors, which are important in the initiation,
progress and prognosis of a disease. In the present study,
split-signal FISH was used and ETV6 rearrangement was observed. To
the best of our knowledge, this is the first case of ETV6
involvement in translocation in BPDCN. Repression of ETV6 appears
to be important in the regulation of cell growth and
differentiation (10,11). In addition, ETV6 has been shown to
stimulate erythroid differentiation of a murine erythroid leukemia
cell line (11). However, further
research is required to establish whether ETV6 rearrangement
participates in the pathogenesis and leukemic transformation of
BPDCN. Furthermore, BPDCN usually has an abnormal and complex
karyotype, lacking specific chromosomal aberrations (12). ETV6 rearrangement may not be the
primary transforming event in BPDCN, while the abnormal karyotype
observed in the patient of the present study may be exceptional in
BPDCN. However, the molecular pathogenesis of the disease remains
unclear.
BPDCN is not sensitive to conventional chemotherapy
and the prognosis is poor. Currently, no standard treatment for
BPDCN exists. However, AML chemotherapy regimes may not be the
optimal treatment methods for BPDCN. By contrast, acute
lymphoblastic leukemia (ALL) protocols have been shown to be more
advantageous (13). In the present
study, the patient received ALL-like schemes (VDCP, MEVP) and
AML-like schemes (HAD) in succession. A complete remission was
achieved in the early stage; however, the two schemes were invalid
in the relapse phase. Allogeneic hematopoietic stem cell
transplantation should be considered to be the most effective
treatment measure.
In conclusion, BPDCN is a rare disease with a poor
prognosis. It is similar to acute leukemia but with high-risk
features. The current study is the first, to the best of our
knowledge, to describe the ETV6 rearrangement in BPDCN. The
significance of the ETV6 rearrangement in BPDCN requires further
study. Additional studies with larger sample sizes are required in
order to increase understanding of the disease and its molecular
and biological features.
References
|
1
|
Facchetti F, Jones DM and Petrella T:
Blastic plasmacytoid dendritic cell neoplasm. Swerdlow SH, Campo E,
Harris NL, et al: WHO Classification of Tumors of Hematopoietic and
Lymphoid Tissues. 4th edition. IARC Press; Lyon: pp. 145–147.
2008
|
|
2
|
Petrella T, Comeau MR, Maynadié M,
Couillault G, et al: ‘Agranular CD4+ CD56+ hematodermic neoplasm’
(blastic NK-cell lymphoma) originates from a population of CD56+
precursor cells related to plasmacytoid monocytes. Am J Surg
Pathol. 26:852–862. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Maki K, Arai H, Waga K, Sasaki K, Nakamura
F, Imai Y, et al: Leukemia-related transcription factor TEL is
negatively regulated through extracellular signal-regulated
kinase-induced phosphorylation. Mol Cell Biol. 24:3227–3237. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Willemze R, Jaffe ES, Burg G, Cerroni L,
Berti E, Swerdlow SH, Ralfkiaer E, Chimenti S, Diaz-Perez JL,
Duncan LM, et al: WHO-EORTC classification for cutanous lymphomas.
Blood. 105:3768–3785. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Adachi M, Maeda K, Takekawa M, Hinoda Y,
Imai K, Sugiyama S and Yachi A: High expression of CD56 (N-CAM) in
a patient with cutaneous CD4-positive lymphoma. Am J Hematol.
47:278–282. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Chinese Society of Hematology, Chinese
Medical Association and Society of Hematological Malignancies
Chinese Anti-Cancer Association. A Chinese expert panel consensus
on diagnosis and treatment of adult acute lymphoblastic leukemia.
Zhonghua Xue Ye Xue Za Zhi. 33:789–792. 2012.(In Chinese).
|
|
7
|
Jin J; Chinese Society of Hematology and
Chinese Medical Association. Chinese guidelines for the diagnosis
and treatment of relapsed and refractory acute myelogeneous
leukemia. Zhonghua Xue Ye Xue Za Zhi. 32:887–888. 2011.(In
Chinese).
|
|
8
|
Xue R, Wu T, Pan H, Gu Y, Yang B, Chen Y
and Qiu J: A case of cutaneous blastic plasmacytoid dendritic cell
neoplasm. Acta Derm Venereol. 90:645–646. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Facchetti F, Ungari M, Marocolo D, Lonardi
S and Vermi W: Blastic plasmacytoid dendritic cell neoplasm.
Haematol Meet Rep. 3:1–3. 2009.
|
|
10
|
Lopez RG, Carron C, Oury C, Gardellin P,
Bernard O and Ghysdael J: TEL is a sequence-specific
transcriptional repressor. J Biol Chem. 274:30132–30138. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Takahashi W, Sasaki K, Kvomatsu N and
Mitani K: TEL/ETV6 accelerates erythroid differentiation and
inhibits megakaryocytic maturation in a human leukemia cell line
UT-7/GM. Cancer Sci. 96:340–348. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Leroux D, Mugneret F, Callanan M,
Radford-Weiss I, Dastugue N, Feuillard J, Le Mée F, Plessis G,
Talmant P, Gachard N, et al: CD4(+), CD56(+) DC2 acute leukemia is
characterized by recurrent clonal chromosomal changes affecting 6
major targets: a study of 21 cases by the Groupe Français de
Cytogénétique Hématologique. Blood. 99:4154–4159. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Piccaluga PP, Paolini S, Sapienza MR and
Pileri SA: Blastic plasmacytoid dendritic cell neoplasm: is it time
to redefine the standard of care? Expert Rev Hematol. 5:353–355.
2012. View Article : Google Scholar : PubMed/NCBI
|