Introduction
Marchiafava-Bignami disease (MBD) is a rare
neurological disease often associated with chronic, heavy alcohol
consumption and malnutrition, and is characterized by callosal
lesions consisting of necrosis and demyelination (1–4).
Over the past few years, magnetic resonance imaging (MRI) findings
of the callosal and cortical lesions, which are critical for the
diagnosis of MBD, have been investigated (5). To date, the etiology of MBD is
incompletely understood. In excess of 90% of patients with MBD
exhibit a poor prognosis (6);
however, with adequate therapy, these patients can recover
completely, with the disappearance of the callosal lesions on
serial MRI (7–8).
It is well known that MBD is widely observed and can
be caused by any alcoholic beverage. It appears that, with
alcoholism, the prognosis is worse; however, MBD can occur in
patients who have no history of alcohol abuse (9–11).
The main hypothesis for the pathogenesis of MBD is that the
condition is associated with malnutrition or vitamin B deficiency
(9), although there are reports
describing cases of MBD caused by existing cyanide, CO poisoning
and sepsis, as well as sickle cell disease and Plasmodium
infection (3). The treatment of
MBD in those patients remains controversial; however, the
administration of nutritional factors, such as high-dose group B
vitamins and folic acid, is believed to be beneficial, and numerous
patients have shown improvements following the administration of
vitamin B therapy (9,12).
The present study describes a case of MBD in a
non-drinker, who had previously undergone cardiac carcinoma
surgery. The study was conducted in accordance with the Declaration
of Helsinki and with approval from the Ethics Committee of the
Harrison International Peace Hospital (Hengshui, China). Written
informed consent was obtained from participant.
Case report
Patient history
The patient, a 62-year-old male, came from Hengshui
Wuyi county and was referred to our department due to dizziness and
gait instability that had persisted for >10 days. The patient
staggered from side to side, fell several times due to the gait
instability, did not dare to stand and exhibited continuously
worsening symptoms. The patient also had a dull expression and
hypomnesia. Three years previously, the patient had undergone
cardiac carcinoma surgery and was prescribed long-term oral
ranitidine and furazolidone. The family members of the patient
complained that his food intake had decreased significantly and
that he had recently suffered from delusions, following which his
appetite had reduced further. The patient had no history of poison
contact or drinking or drug abuse.
Physical, biochemical and imaging
examinations
Physical examination of the patient revealed that he
was lucid when conscious, but exhibited slurred speech, apathy,
cognitive impairment and poor calculation and memory. The bilateral
pupils of the patient were round and equal, his light reflex and
eyeball motion were normal, and the patient did not exhibit
nystagmus. His bilateral frontalis and nasolabial groove were
approximately symmetrical, and his tongue was in the center. The
muscle strength of the patient’s extremities was grade 5, with
normal muscle tone. The patient had no sensory disturbance, and his
physiological reflexes were present without pathological reflex.
The finger-to-nose and fast alternating movement tests showed the
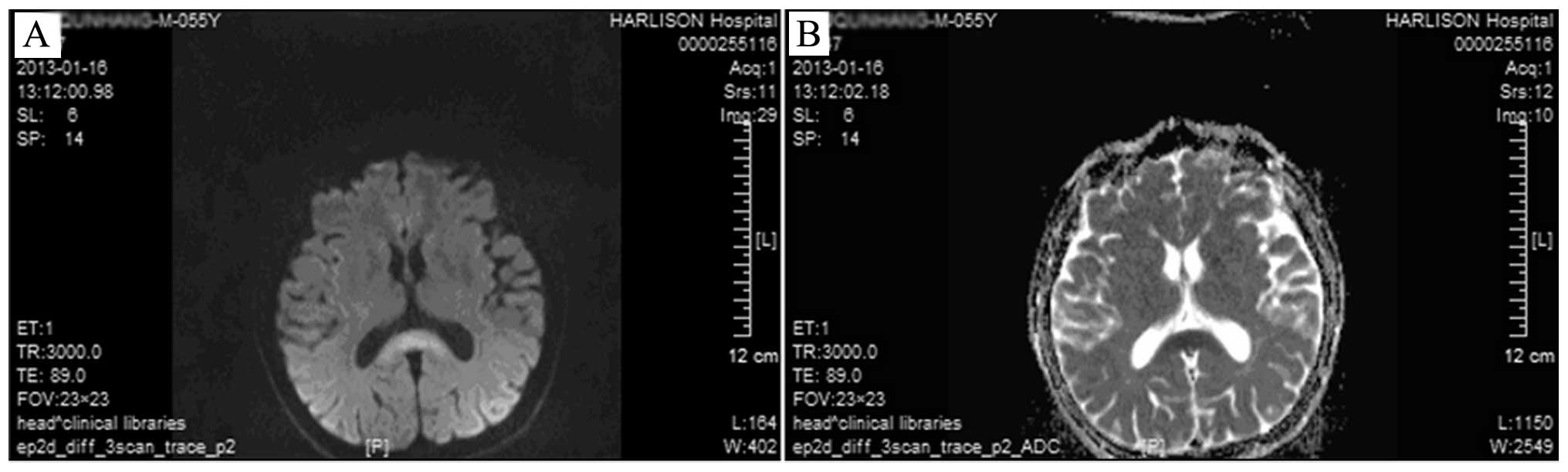
patient to be slightly clumsy, and MRI showed symmetric abnormal
signals in the splenium of the corpus callosum (Fig. 1). Blood lipid tests revealed a
total cholesterol level of 6.29 mmol/l and a low-density
lipoprotein level of 3.96 mmol/l. Routine blood, urine, liver and
kidney function and blood coagulation tests showed no obvious
abnormalities, and no abnormalities were found with thoracic and
abdominal computed tomography. The diagnosis was MBD. The patient
was told to consume a diet rich in vitamins to improve the brain
blood and oxygen supply, and was prescribed vitamins B1 and B6,
methylcobalamin, and folic acid treatments. Two weeks after
admission, the slow responses and delusions of the patient had
improved markedly. Following discharge, the patient was followed-up
for two months. He could walk freely and live on his own.
Discussion
To date, the etiology of MBD is incompletely
understood, as it is one of the rare complications of chronic
alcoholism (1–2). It is believed that MBD may be closely
associated with chronic alcoholism and/or malnutrition caused by
long-term alcohol abuse; however, MBD can also occur in patients
who have no history of alcohol abuse (9–11).
The main hypothesis for MBD pathogenesis is that the condition may
be associated with malnutrition or vitamin B deficiency (9), although it is believed that MBD may
have other etiologies. There are reports on MBD caused by existing
cyanide, CO poisoning and sepsis, as well as sickle cell disease
and Plasmodium infection (3).
The present study describes a patient who had
undergone cardiac carcinoma surgery three years previously, and who
had received chemotherapy three times; the last chemotherapy
session was one-and-a-half years prior to admission. The etiology
of the patient’s condition may have been similar to that described
in a previous study, in which a metabolic disorder of the myelin in
the brain of a patient with no long-term alcohol abuse, which was
caused by long-term malnutrition involving protein, folic acid and
particularly thiamine deficiency, led to demyelinating changes and
MBD (9). The corpus callosum,
which is the largest commissural fiber system within the
hemisphere, has a relatively high myelin content, and may often
cause the degeneration and necrosis of nerve cells in such
patients. The treatment of MBD in these patients remains
controversial, although it is believed that nutritional factors,
such as high-dose group B vitamins and folic acid, may be
beneficial.
Over the past few years, MRI findings of the
callosal and cortical lesions, which are critical for the diagnosis
of MBD, have been investigated (5). An improvement in the neurological
disorder occurring concurrently with a change in the MRI findings
following therapy should therefore enhance the understanding of the
disease, which may be beneficial for the definitive diagnosis and
monitoring of MBD in patients with no long-term alcohol abuse.
Specific MRI changes have been approved as the main basis for the
diagnosis of the condition, including a slightly low or hypointense
signal on the T1WI, and a hyperintense signal on the T2WI,
fluid-attenuated inversion recovery and diffusion-weighted imaging
sequences. The MR images of the patient in the present case were
consistent with those expected for MBD (Fig. 1A and B).
For the patient in the present report, a number of
diseases and conditions had to be excluded prior to a diagnosis of
MBD being reached. The first condition was paraneoplastic syndrome
(PNS), which is characterized by symptoms including cerebellar
degeneration and limbic encephalitis. Patients with PNS also
exhibit cerebrospinal fluid (CSF) pleocytosis and elevated protein
and immunoglobulin G levels. The routine CSF and biochemical tests
of the present patient were normal, and the brain MRI results were
not consistent with PNS. Furthermore, the condition of the patient
improved following vitamin treatment; none of these observations
supported a diagnosis of PNS. Secondly, multiple sclerosis (MS) had
to be excluded. MS lesions are relatively small, and the condition
predominantly manifests as multiple lesions of the periventricular
white matter. The lesions rarely develop initially or appear only
in the corpus callosum. In the majority of cases of MS, the
condition exhibits remission and relapse. In the present case, the
condition of the patient, the CSF tests and the MRI findings were
not in accordance with MS. A third possible condition was
Wernicke’s encephalopathy (WE). In patients with WE, the bilateral
thalamus and brainstem often show symmetrical lesions, and the
typical MRI findings are abnormal signals in the mammillary body,
aqueduct and around the third ventricle, which can be combined with
MBD. The MRI of this patient revealed a solitary lesion in the
corpus callosum, which was not consistent with WE. A fourth
condition to be excluded was corpus callosum infarction, which is
rarely seen in the clinic. The anterior and posterior cerebral
arteries supply blood to the anterior and posterior corpus
callosum, respectively, and most lesions are unilateral. A fifth
possible condition was progressive multifocal leukoencephalopathy
(PML), which is a type of progressive demyelinating disease caused
by papovavirus infection. In addition to the corpus callosum, this
disease involves the subcortical white matter, and the lesions show
a non-symmetrical distribution. Furthermore, as time progresses,
the lesions may exhibit an integration trend. PML is dangerous,
progressive and has a poor prognosis, but the observations in the
present case did not support a PML diagnosis. Finally, a
poison-induced disease had to be excluded. Since the mechanisms
underlying brain damage in poisoning diseases, such as CO,
organophosphorus, lead or mercury poisoning, are different, the
lesions in the cerebral white matter are different, and the MRI
features, which involve the basal ganglia, brainstem, cerebellum
and cortex, are not specific. Furthermore, the patient may have a
clear history of poisoning.
MBD may be a reversible brain disease. Clinicians
should enhance the awareness of the disease and emphasize that the
disease cannot be ignored in patients without a drinking history,
particularly in malnourished patients. An improvement in the
neurological disorder occurring concurrently with a change in the
corpus callosum degeneration following therapy should enhance the
understanding of the disease, which may be beneficial for the
definitive diagnosis and early treatment of MBD.
References
|
1
|
Suzuki Y, Oishi M, Ogawa K and Kamei S: A
patient with Marchiafava-Bigami disease as a complication of
diabetes mellitus treated effectively with corticosteroid. J Clin
Neurosci. 19:761–762. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Tung CS, Wu SL, Tsou JC, Hsu SP, Kuo HC
and Tsui HW: Marchiafava-Bignami disease with widespread lesions
and complete recovery. AJNR Am J Neuroradiol. 31:1506–1507. 2010.
View Article : Google Scholar
|
|
3
|
Boutboul D, Lidove O, Aguilar C, Klein I
and Papo T: Marchiafava-Bignami disease complicating SC hemoglobin
disease and Plasmodium falciparum infection. Presse Med.
39:990–993. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Tuntiyatorn L and Laothamatas J: Acute
Marchiafava-Bignami disease with callosal, cortical and white
matter involvement. Emerg Radiol. 15:137–140. 2008. View Article : Google Scholar
|
|
5
|
Wenz H, Eisele P, Artemis D, Förster A and
Brockmann MA: Acute Marchiafava-Bignami disease with extensive
diffusion restriction and early recovery: case report and review of
the literature. J Neuroimaging. 24:421–424. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Namekawa M, Nakamura Y and Nakano I:
Cortical involvement in Marchiafava-Bignami disease can be a
predictor of a poor prognosis: a case report and review of the
literature. Intern Med. 52:811–813. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kinno R, Yamamoto M, Yamazaki T, Owan Y,
Fukui T and Kinugasa E: Cerebral microhemorrhage in
Marchiafava-Bignami disease detected by susceptibility-weighted
imaging. Neurol Sci. 34:545–548. 2013. View Article : Google Scholar
|
|
8
|
Yoshizaki T, Hashimoto T, Fujimoto K and
Oguchi K: Evolution of callosal and cortical lesions on MRI in
Marchiafava-Bignami disease. Case Rep Neurol. 2:19–23. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Carrilho PE, Santos MB, Piasecki L and
Jorge AC: Marchiafava-Bignami disease: a rare entity with a poor
outcome. Rev Bras Ter Intensiva. 25:68–72. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Celik Y, Temizoz O, Genchellac H, Cakir B
and Asil T: A non-alcoholic patient with acute Marchiafava-Bignami
disease associated with gynecologic malignancy: paraneoplastic
Marchiafava-Bignami disease? Clin Neurol Neurosurg. 109:505–508.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Rusche-Skolarus LE, Lucey BP, Vo KD and
Snider BJ: Transient encephalopathy in a postoperative
non-alcoholic female with Marchiafava-Bignami disease. Clin Neurol
Neurosurg. 109:713–715. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hoshino Y, Ueno Y, Shimura H, Miyamoto N,
Watanabe M, Hattori N and Urabe T: Marchiafava-Bignami disease
mimics motor neuron disease: case report. BMC Neurol. 13:2082013.
View Article : Google Scholar : PubMed/NCBI
|