Introduction
Pheochromocytomas are derived from chromaffin cells
and secrete catecholamines; 15–20% of pheochromocytomas are
extra-adrenal and termed as paragangliomas (1). A high incidence of malignancy
(13–26%) has been reported in paragangalioma (2). Complete surgical resection has been
recommended as the mainstay of management (3). Yet, due to severe hypertension and
its consequences, the anesthetic management has been quite
challenging and the mortality rate remains high, particularly in
those close to the aorta or in patients having aortic complications
(4). Preoperatively, it is
difficult to control blood pressure due to its pulse release of
catecholamines and waves of blood pressure changes.
Intraoperatively, there are fluctuations in blood pressure due to
the clamping, maneuver, ligation of the arteries, lack of
communication between the surgeons and anesthesiologist, and the
dosing of the medications. Postoperatively, the hemodynamic state
of the patient requires intensive monitoring. The present case
report describes the successful anesthetic management used in a
unique case of para-aortic ganglioma resection with unexpected
aortic segment resection. The key factors cosnidered are α and β
blockades as necessary to control BP preoperatively, frequent
communication between the anesthesiologist and surgeon,
intraoperative intervention in excess catecholamine release with
phentolamine, nitroprusside and labetalol prior to tumor removal,
and vasopressin for catecholamine deficiency when clamping or
subsequent to tumor removal.
Multiple attempts have been made to contact the
patient or their legal designee for consent; however, these have
not been successful. Approval was thus sought from the VA Western
New York Healthcare System Institutional Review Board (Buffalo, NY,
USA) who determined that approval was not required.
Case report
Patient
A 64-year-old male was admitted to the VA Western
New York Healthcare System for the resection of
pheochromocytoma/paraganglioma. The patient had been diagnosed with
pheochromocytoma during a previous surgery. This was further
confirmed by the patient’s significant symptoms, magnetic resonance
imaging (MRI; 5 mm lesion, 1.8 cm proximal to aortic bifurcation)
and 24 h urine normetanephrine (4-fold greater than the normal
upper limit) and vanillylmandelic acid (VMA; 1.5-fold greater than
the normal upper limit). Systemic review revealed hypertension,
hyperlipidemia, osteoporosis, rectal carcinoma and
pheochromocytoma. The patient weighed 84 kg and was 168 cm in
height.
Pre-operative assessment and
preparation
The patient had been taking an α-blocker
(phenoxybenzamine, 10 mg twice per day, orally) for over a month
and then a β-blocker (metoprolol). The blood pressure (BP) was
maintained at ~120/80 mmHg, and the heart rate (HR) was 55 bpm. The
Mallampati class was 2, the American Society of Anesthesiologists
(ASA) class was 3, the hemoglobin level was 12.9 g/dl and the
hematocrit was 38.3%. An electrocardiogram revealed no
abnormalities and chest X-ray indicated no active disease. During
the arterial line placement, the patient complained of nausea, the
BP dropped to 80/50 mmHg and the HR rose to 70 bpm. This was
resolved after the patient lay flat and a 500-ml bolus of normal
saline was given.
Intra-operative management
The patient was placed under general anesthesia,
with two large peripheral intravenous lines (PIVs), one arterial
line, one right internal jugular central line and a pulmonary
artery catheter. A total of 1–3 mg/kg/h propofol and 2–20
mcg/kg/dose fentanyl were used for induction, and nitroglycerine
was readily available. During the procedure, aortic segment
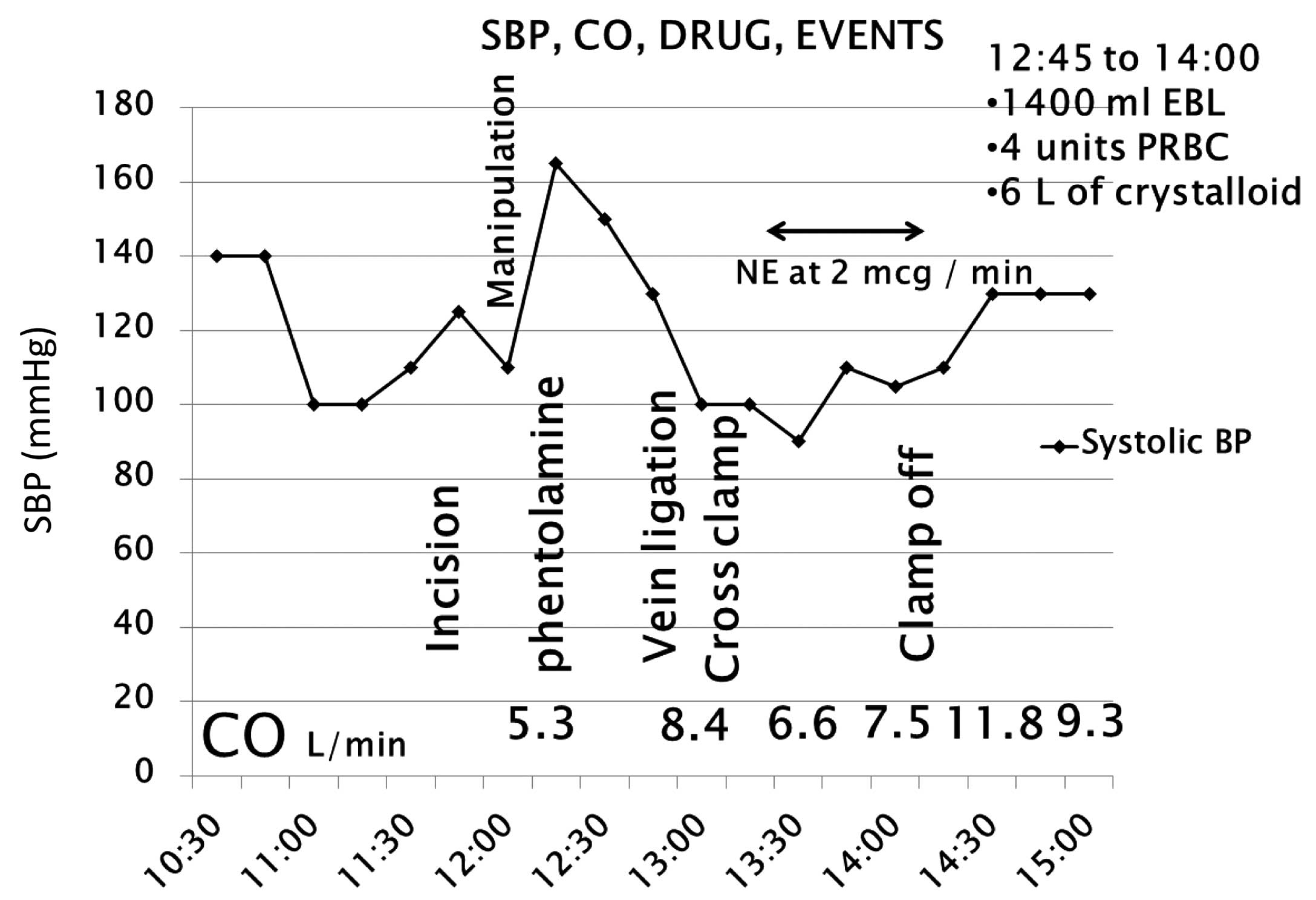
resection was required to complete the tumor resection. As shown in
Fig. 1, due to tumor manipulation
and catecholamine release, the BP of the patient increased. This
was managed with phentolamine, nitroprusside, esmolol and
labetolol. Tumor vein ligation and clamping triggered a reduction
of the BP, which was managed with norepinephrine (NE) and
vasopressin. Continuous NE infusion was set at a rate of 2 μg/min.
During the whole procedure, the cardiac output was maintained
within the normal range, 6 liters of crystalloid and 4 units of
packed red blood cells were administered, and there was an
estimated blood loss of 1,400 ml. The blood glucose level was 174
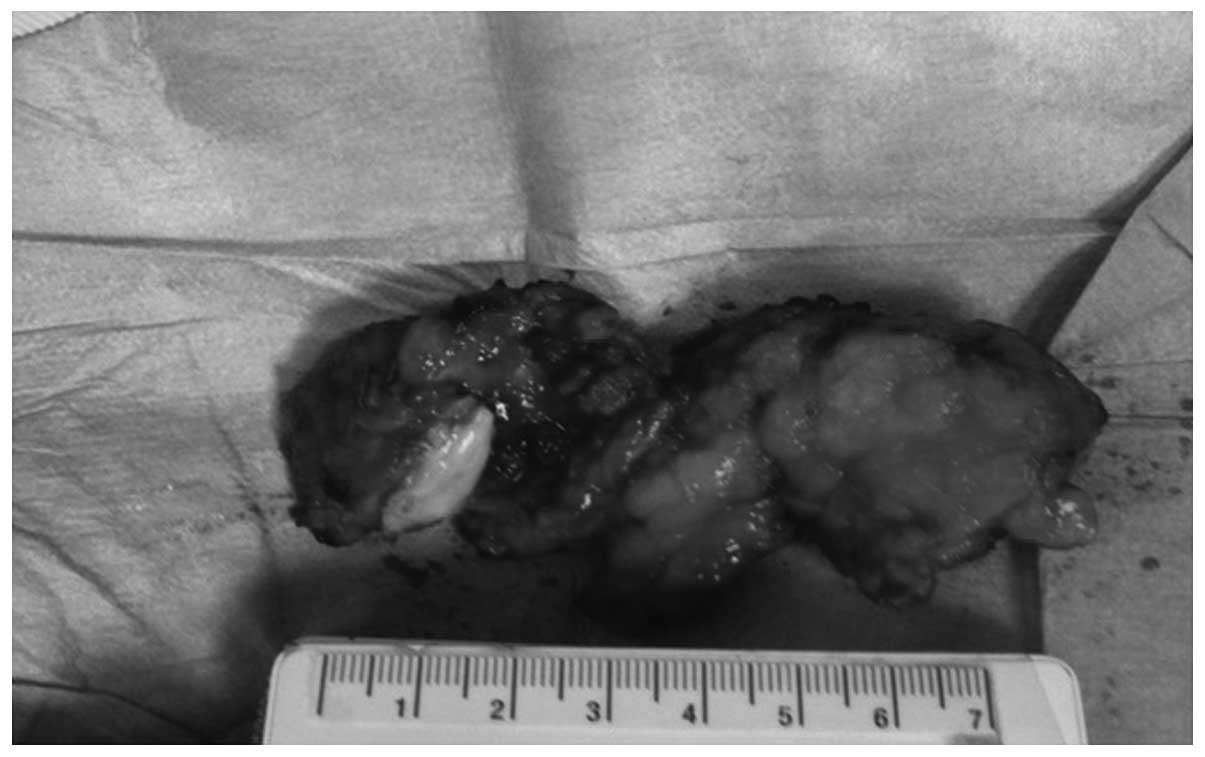
mg/dl. Fig. 2 shows the gross
resected mass. Diagnosis was further confirmed by pathological
examination, which identified an extra-adrenal paraganglioma, 4.3
cm in diameter, within a para-aortic ganglion and invading the
aortic adventitia, without evidence of adrenal parenchyma or
angiolymphatic invasion. Positivity for chromogranin and S100, a
low proliferative index and negative nodes were observed.
Post-operative management
Following the procedure, the patient was transferred
to the intensive care unit (ICU) without pressor medication,
intubated and hemodynamically stable. The patient was extubated the
next morning, transferred to the ward after 24 h, and discharged 5
days later, in a hemodynamically stable condition.
Discussion
To the best of our knowledge, this is the first case
report of successful anesthetic management in the resection of
paraganglioma along with unexpected aortic resection. The success
achieved suggests that delicate management can reduce mortality,
even with unexpected challenges. The key is maintaining the BP
within a reasonable range and keeping the patient hemodynamically
stable. The hallmarks include preoperative α blockade, and
intraoperative intervention in excess catecholamine release prior
to tumor removal and catecholamine deficiency following tumor
removal.
As shown in Table
I, we recommend that pre-operative management should focus on
complete α blockade and β blockade as necessary to avoid
hypertensive crisis during induction. A course of 10–14 days α
blockade is recommended prior to the addition of β blockade.
Notably, β blockade should never be initiated without successful α
blockade, as this may trigger hypertensive crisis due to unopposed
α-adrenergic receptor stimulation (5). A norepinephrine synthesis inhibitor
may be used as an alternative. However, it generally takes 3 weeks
to take effect. The common agents used are phenoxybenzamine,
propanolol and metyrosine, respectively (3,6).
Calcium channel blockers have also been used to achieve a better
control of BP in addition to α blockade, for patients intolerant to
α blockade, and those with intermittent hypertension (3,7). In
the present case, the BP of the patient was well controlled with α
blockade and β blockade as necessary pre-operatively. However, the
patient complained of feeling unwell and BP changes occurred during
induction, which were resolved by the patient lying down and
receiving fluid resuscitation. This is a reminder that caution
should be paid even with good BP control pre-operatively, as any
stimulation of the vessels/tumor could dramatically change the
vessel tone and thus BP.
 | Table IManagement of para-ganglioma
resection. |
Table I
Management of para-ganglioma
resection.
| Management | Recommendation |
|---|
| Operative |
| Pre-operative | α-blocker (≥2 weeks),
β-blocker (after α-blocker), cathecholamine synthesis inhibitor,
calcium channel blocker |
| Intra-operative | Communication between
surgeons, nitrupresside/labetolol for BP, NE for tumor vein
ligation/clamping, magnesium, clevidipine |
| Post-operative | Vasopressin, blood
glucose, urine VMA |
| Avoid/caution |
| Food | Aged cheese, yogurt,
sour cream, wine, beer, chocolate, smoked meats, fermented bean or
fish products, nuts, certain fruits and vegetables |
| Drugs | β blockade before α
blockade, D2 receptor antagonists, serotonin/NE receptor
inhibitors, sympathomimetics, chemotherapeutics, α-blocker for
tumor manipulation, opiates, neuromuscular blockers, peptides and
steroids |
For intra-operative management, frequent
communication between surgeons and the anesthesiologist is
extremely important, as manipulation of the tumor, clamping and
unclamping of the aorta, and other stimulation can change the BP
significantly. Increased BP could increase bleeding from small
vessels. Due to catecholamine release, hyperglycemia presented
during the operation. However, the over-treatment of hyperglycemia
may cause significant post-operative hypoglycemia. It is
recommended that an arterial line should be put in place prior to
induction to monitor the BP. A central venous catheter and
large-bore peripheral catheter should be used to manage
resuscitation. The successful management in the present case
suggests that changes in BP can be well controlled during surgery,
based on pathophysiology. In the present case, α blockade was used
to intervene in the excess catecholamine release due to tumor
manipulation; nitroprusside and labetolol were also used to better
control the BP, and NE was administered to maintain the BP which
fell due to catecholamine deficiency when clamping or following
tumor removal. This is consistent with the majority of studies
(3,7), indicating that dedicated monitoring
and intervention can benefit the patient and reduce mortality
significantly. Magnesium and clevidipine have also been used to
control or maintain BP (1).
It is recommended that post-operative management
should be focused on blood glucose monitoring, BP normalization,
urine 24 h catecholamine measurements 1–2 weeks after surgery and
associated check-ups (6).
Certain food and drugs should be avoided or used
with caution prior to surgery (5,6).
Foods rich in tyrosine such as aged cheese, yogurt, sour cream,
wine, beer, chocolate, smoked meats, fermented soy bean or fish
products, nuts and certain fruits and vegetables should be avoided
or limited in intake (5). Some
drugs, such as β-blockers prior to α-blockers, dopamine D2 receptor
antagonists, serotonin receptor inhibitors, NE receptor inhibitors,
monoamine oxidase inhibitors, tricyclic antidepressants,
sympathomimetics, chemotherapeutic agents, opiates, neuromuscular
blockers, peptides and steroids should also be avoided (3).
In conclusion, the anesthetic management in this
challenging case of para-aortic ganglioma resection with unexpected
aortic segment resection was successful. It suggests that resection
of a paraganglioma and aortic segment requires delicate anesthetic
management. The key features are α blockade and β blockade as
necessary to control the BP pre-operatively, frequent communication
between the anesthesiologist and surgeons, intra-operative
intervention in excessive catecholamine release with phentolamine,
nitroprusside and labetalol prior to tumor removal, and vasopressin
for catecholamine deficiency when clamping or subsequent to tumor
removal. It is a delicate procedure, requiring teamwork and
orchestration.
References
|
1
|
Lord MS and Augoustides JG: Perioperative
management of pheochromocytoma: focus on magnesium, clevidipine,
and vasopressin. J Cardiothorac Vasc Anesth. 26:526–531. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Subramaniam R: Pheochromocytoma - current
concepts in diagnosis and management. Trends in Anaesthesia &
Critical Care. 1:104–110. 2011. View Article : Google Scholar
|
|
3
|
Martucci VL and Pacak K: Pheochromocytoma
and paraganglioma: diagnosis, genetics, management, and treatment.
Curr Probl Cancer. 38:7–41. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Bowen FW, Civan J, Orlin A and Gleason T:
Management of type A aortic dissection and a large
pheochromocytoma: a surgical dilemma. Ann Thorac Surg.
81:2296–2298. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hodin R, Lubitz C, Phitayakorn R and
Stephen A: Diagnosis and management of pheochromocytoma. Curr Probl
Surg. 51:151–187. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Tsirlin A, Oo Y, Sharma R, Kansara A,
Gliwa A and Banerji MA: Pheochromocytoma: a review. Maturitas.
77:229–238. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Jugovac I, Antapli M and Markan S:
Anesthesia and pheochromocytoma. Int Anesthesiol Clin. 49:57–61.
2011. View Article : Google Scholar : PubMed/NCBI
|