Introduction
As the most common form of extrapulmonary
tuberculosis (TB), spinal TB has remained prevalent worldwide,
particularly in the less developed and developing countries
(1,2), occurring in 1.7% of the world
population (3) and accounting for
almost 50% of cases of skeletal TB (4). Additionally, it can be the most
dangerous form of skeletal TB due to its capacity for causing bone
destruction, deformity and paraplegia (5). Anti-tuberculous chemotherapy has proven
effective in the majority of cases and has become the mainstay of
treatment (6), yet it cannot prevent
kyphotic degeneration (7,8). Surgery is therefore frequently
imperative for spinal decompression (9).
Various surgical methods have been described for
treating spinal TB. While there are advantages to exposing the
pathological site directly and resecting damaged vertebrae,
sequestra of disc and bone, and tuberculous granuloma, which cause
predominantly anterior compression of the spinal cord, have led
certain authors (10,11) to consider the anterior approach too
invasive and often unnecessary in the context of spinal TB. The
anterior approach may also involve division of the diaphragm and
segmental spinal vessels. An increasing number of surgeons have
adopted the method of posterior debridement, bone fusion and
posterior fixation to treat monosegmental spinal TB. However,
complications resulting from damage to the posterior spinal column
due to the posterior approach reduce the surgical effect and affect
the patient's quality of life (12).
A procedure that caused less damage to the posterior spinal column
would be of great clinical significance. In the current study, the
clinical outcomes of one-stage posterior debridement, limited
decompression, bone grafting and internal fixation combined with
lamina reconstruction were compared with that of single posterior
debridement, decompression, interbody fusion and posterior
instrumentation for treating spinal TB.
Subjects and methods
Patient information
Written informed consent was obtained from the
patients and the Xiangya Hospital Ethics Committee approved the
study protocol. A total of 73 patients with spinal TB (without
active pulmonary TB) who had been treated at the Xiangya Hospital
(Changsha, Hunan, China) from January 2006 to April 2011 were
enrolled. There were 41 males and 32 females; the mean age at
surgery was 38.6 years (range, 22–62 years) (Table I). The patients presented with
constitutional symptoms such as back pain, limited spinal mobility,
and a hump-shaped deformity. There was a neurological deficit in 49
patients, varying in severity from unilateral or bilateral numbness
and lower extremity weakness to walking disorders (Table II). The pre-operative erythrocyte
sedimentation rate (ESR) and Oswestry Disability Index (ODI) were
abnormal (Table III).
 | Table I.Patient characteristics. |
Table I.
Patient characteristics.
| Characteristics | Group A | Group B | P-value |
|---|
| Gender |
|
| 0.964 |
| Male | 19 | 22 |
|
|
Female | 15 | 17 |
|
| Mean age (years) | 38.7±8.0 | 38.4±8.3 | 0.888 |
| Pathological
region |
|
|
|
|
Thoracic | 15 | 17 | 0.964 |
|
Thoracolumbar | 10 | 12 | 0.900 |
|
Lumbar | 9 | 10 | 0.319 |
| Concurrent
disease |
|
|
|
|
Hypertension | 4 | 5 | 0.891 |
|
Diabetes | 5 | 7 | 0.709 |
| Coronary
heart disease | 6 | 9 | 0.567 |
|
Electrocardiographic
abnormality | 8 | 11 | 0.650 |
 | Table II.Neurological recovery according to the
American Spinal Injury Association grade (groups A and B). |
Table II.
Neurological recovery according to the
American Spinal Injury Association grade (groups A and B).
| Group A/B | Group A final
follow-up | Group B final
follow-up |
|---|
|
|
|---|
| Pre-operation | n/n | A | B | C | D | E | A | B | C | D | E |
|---|
| A | 0/0 |
|
|
|
|
|
|
|
|
|
|
| B | 2/2 |
|
| 1 | 1 |
|
|
| 2 |
|
|
| C | 9/11 |
|
| 1 | 3 | 5 |
|
| 1 | 5 | 5 |
| D | 12/13 |
|
|
|
| 12 |
|
|
|
| 13 |
| E | 11/13 |
|
|
|
| 11 |
|
|
|
| 13 |
 | Table III.Patient clinical data. |
Table III.
Patient clinical data.
| Group | Surgery duration
(min) | Amount of bleeding
(ml) | Hospital stay
(days) | ESR | ODI | Fusion time
(months)e |
|---|
|
|
|---|
|
|
|
|
| Pre | Postc | Pre | LVd |
|
|---|
| A | 171.4±12.2 | 717.6±110.8 | 13.5±2.1 | 53.9±15.9 | 10.4±2.6 | 40.2±3.9 | 10.1±3.0 | 7.2±1.5 |
| B |
160.4±15.6a |
803.1±124.6a |
14.0±2.9b | 55.0±15.6 | 9.1±2.4 | 39.7±4.0 | 20.6±3.0 | 8.1±1.5 |
Diagnosis was based on non-specific laboratory and
imaging findings, including spinal radiographic films, computed
tomography (CT) and magnetic resonance imaging. The mean disease
course was 10 months (range, 3–16 months). The findings showed the
following indications for surgery: i) Progressive neurological
deficit; ii) persistent pain due to instability; iii) severe
kyphosis or kyphosis likely to progress (9); iv) poor outcome following conservative
treatment. Patients who met the surgical criteria were assigned to
group A or B. Patients in the former group underwent one-stage
posterior debridement, limited decompression, bone grafting and
internal fixation combined with lamina reconstruction. Patients in
the latter group underwent single posterior debridement,
decompression, bone grafting and instrumentation. In practice, it
is challenging to randomly select a surgical treatment method
clinically; therefore, in the present study, cases in group B were
collected earlier while cases in group A were collected in more
recent years. The same team reviewed the surgical indications and
performed the procedures. Table I
lists the characteristics of each group.
Pre-operative procedure
The patients received standard anti-tuberculous
chemotherapy (300 mg/day isoniazid, 450 mg/day rifampicin, 750
mg/day ethambutol and 750 mg/day pyrazinamide) for an average 2–3
weeks prior to surgery. The surgery was postponed until anemia and
hypoproteinemia recovered and there was a general significant
decrease in ESR.
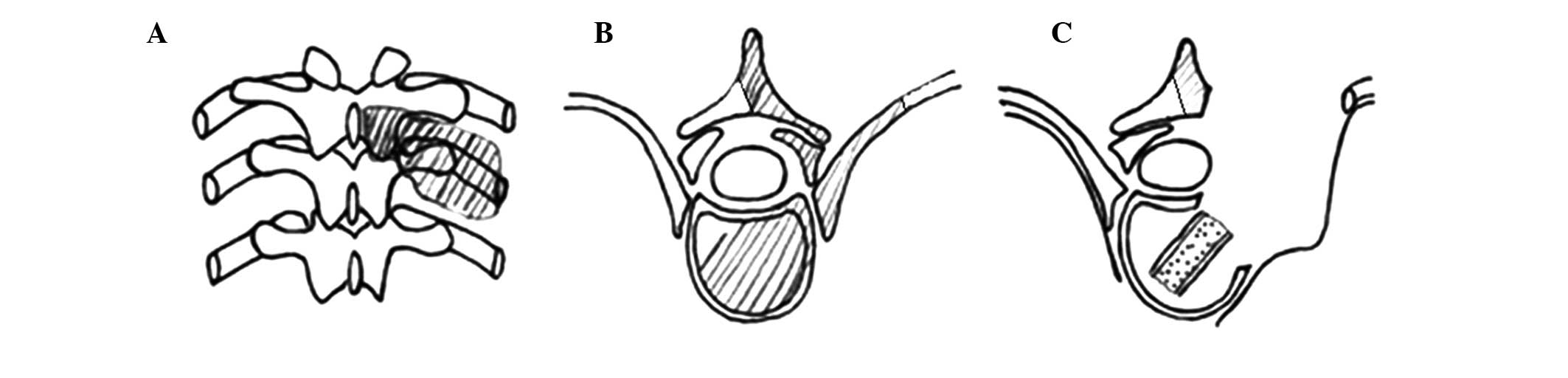
Surgical method
Group A patients were placed in the prone position
and surgery was performed under general endotracheal anesthesia.
Pedicle screws were placed according to the level of decompression
required based on pre-operative imaging. A temporary, pre-bent rod
was then stabilized on the mildly affected side of the focus to
avoid spinal cord injury during decompression and focal
debridement. The side on which the infection was predominant was
selected. Unilateral facetectomy and laminectomy up to the medial
pedicle edge were performed. If required 1.0–1.5 cm were removed
from the rib adjacent to the thoracic spine (Fig. 1). To decompress the spinal cord,
lesions were removed through to healthy bleeding bone using
curettes of various sizes and angles. Somatosensory-evoked
potential monitoring was performed to avoid spinal cord injury.
Thoracic nerve roots on the focal side were sacrificed for better
exposure. The operating table was then tilted 30° to the opposite
side for a better view to enable complete removal of the lesions.
Pus and necrotic tissue were eliminated by pressurized washing
using a soft catheter inserted into the deep part of the lesion
during surgery and negative pressure suction. The appropriate
shaping allograft or autograft was embedded in the bone interbody.
Subsequently, an allograft or autograft plate was embedded in the
lamina defect area excised for focal debridement. To complete the
lamina reconstruction, the rod on the decompressed side and
cross-linkage were connected to immobilize the bone plate.
Streptomycin (1.0 g) and isoniazid (0.2 g) were administered
locally, and drainage and incision suturing were performed
postoperatively. The debrided material was sent for culture and
histopathological examination.
Group B patients underwent expanded hemilaminectomy
(resection of the spinous process, unilateral facet joint, pedicles
and transverse process). The exposed dural sac and posterior body
bone defects were not covered with a bone plate. Other procedures
were the same as that for group A.
Postoperative procedure
Typically, the drain was removed when drainage flow
was <50 ml/24 h. With assistance from a plastic orthosis, the
patients were allowed to start walking gradually after remaining
supine for an average of four weeks postoperatively, depending on
their recovery of lower limb muscle power. The brace was discarded
≤12 months postoperatively. The patients were treated with the
above-mentioned anti-TB chemotherapy regimen for 12–18 months
postoperatively and the ESR and hepatic function were examined
regularly.
Evaluation standard and statistical
analysis
Immediately following surgery, routine lateral and
anteroposterior radiographs and a CT (Brilliance 16-slice; Philips,
Andover, MA, USA) were obtained to assess the placement of graft
and instrumentation and formation of sequestra. The overall mean
follow-up period was 31.3 months (range, 21–42 months). The
following indices were recorded pre- and postoperatively and during
follow-up: i) Cobb angle; ii) angle loss rate, which was calculated
as follows: [(Cobb angle at the last visit)-(postoperative Cobb
angle)/(preoperative Cobb angle)] ×100%; iii) neurological status
according to the Frankel classification; iv) ESR; v) ODI; and vi)
fusion status evaluated according to Lee et al (13).
Statistical analyses were performed using SPSS
software (version 17.0; SPSS Inc., Chicago, IL, USA). Changes in
laboratory and physical parameters in the two groups were compared
using the Student-Newman-Keuls test. Any discrepancy in normal
distribution was analyzed using the rank sum test. P<0.05
indicated statistical significance.
Results
The overall mean follow-up was 31.3 months (range,
21–42 months). Table I shows the
patient data and the neurological status is listed in Table II. No severe neurological
complications were observed in either group. The surgery time,
amount of bleeding and length of hospital stay was recorded for
each patient following surgery (Table
III). The ESR returned to normal within three months
postoperatively (Table III). By
the last visit, the group A ODI values were significantly lower
than those of group B (P<0.05) (Table III). Compared with the
pre-operative values, the ODI values for the two groups were
greatly improved (P<0.05).
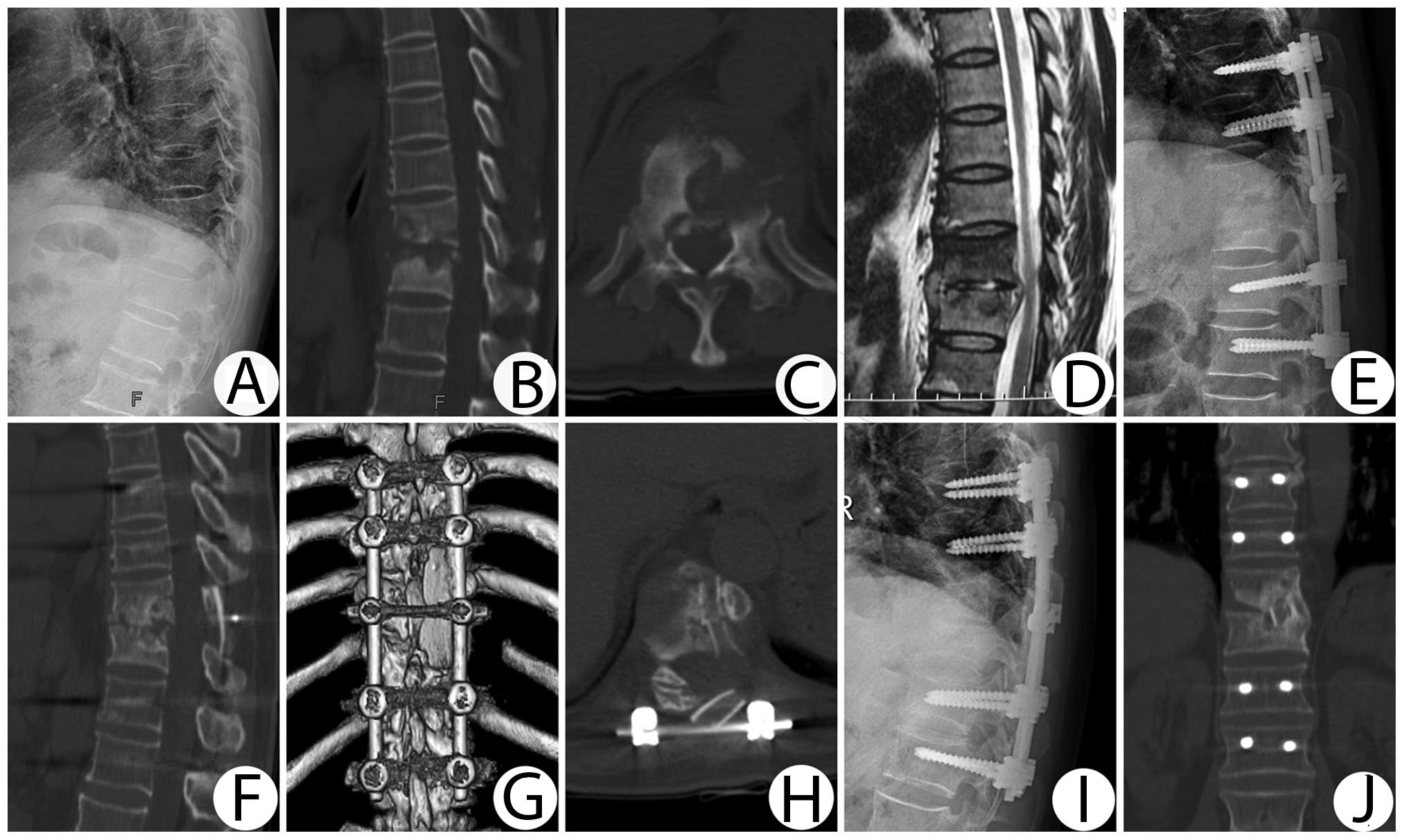
In group A, all the grafted bones ultimately fused
with the fusion time ranging 4–10 months (mean, 7.2 months)
(Fig. 2). The grafts in all but two
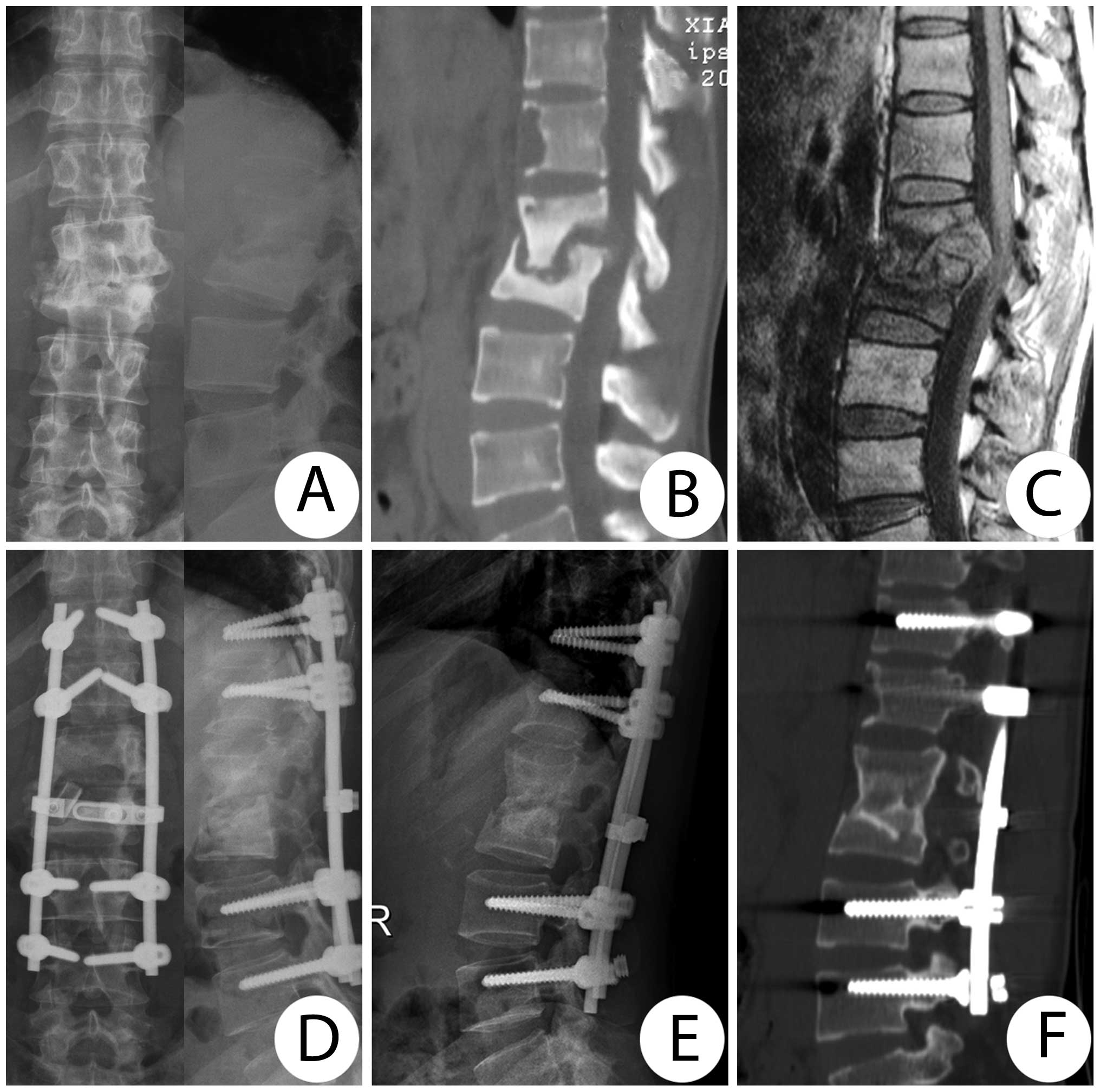
subjects in group B ultimately fused, with the fusion time ranging
6–12 months (mean, 8.1 months) (Fig.
3). Fusion in two patients was delayed due to extraction of
internal fixation. CT scans detected no sequestra in any of the
cases during follow-up.
Table IV lists the
Cobb angles recorded during follow-up. There were significant
differences between the pre- and postoperative values
(PA<0.05, PB<0.05) for the two groups.
No significant difference was observed immediately postoperatively
between the two groups (P=0.396). However, at the last follow-up,
there was a significant difference between loss of correction,
angle loss rate and Cobb angle between the two groups
(P<0.05).
 | Table IV.Patient clinical data. |
Table IV.
Patient clinical data.
| Cobb angle (°) | |
|---|
|
|---|
| Pathological
region | Prea | Postb* | LVc | LCd | Angle loss
ratee |
|---|
| Group A |
|
|
|
|
|
|
Thoracic |
28.8±6.1 |
6.4±1.6 |
8.7±1.8 |
2.2±1.0 |
8.3±4.4 |
|
Thoracolumbar |
32.9±6.5 |
8.5±2.7 |
10.8±2.8 |
2.3±1.0 |
7.5±4.9 |
|
Lumbar |
27.5±7.2 |
5.4±2.9 |
6.9±2.9 |
1.5±0.8 |
6.0±4.4 |
| Group B |
|
|
|
|
|
|
Thoracic |
29.2±5.5 |
7.2±1.9 |
12.1±1.9 |
4.9±1.0 |
17.3±6.0 |
|
Thoracolumbar |
30.5±5.6 |
7.7±2.6 |
12.5±2.5 |
4.8±0.9 |
16.5±5.3 |
|
Lumbar |
26.1±4.7 |
6.8±2.4 |
11.8±2.5 |
5.0±1.3 |
19.9±6.8 |
There was superficial infection in one incision in
group A, which was treated successfully with antibiotics. Five
group B patients experienced surgical complications. There was
superficial infection in one incision, which was managed
successfully with antibiotics. One patient, who suffered from sinus
drainage tube formation one week postoperatively, was successfully
treated by weekly local isoniazid therapy. Extraction of internal
fixation was detected in two patients at the eight- and 10-month
follow-up, respectively, which were successfully treated with
anterior debridement and interbody fusion combined with
long-segment posterior instrumentation. One patient had refractory
intercostal neuralgia, which was relieved by non-steroidal
anti-inflammatory drugs.
Discussion
Despite ongoing efforts by the World Health
Organization and local health authorities, TB remains prevalent in
certain developing countries, affecting all susceptible individuals
(14). Over the last 50 years,
various methods for surgical debridement and fusion have been
described for spinal TB (1,10,15). The
purpose of any procedure is obtaining adequate decompression and
visualization for intervention, and achieving spinal stability.
With the improvement of internal fixation devices, many surgeons
(16–18) have reported that a posterior approach
to fixation achieves good results in the treatment of spinal TB.
Firstly, posterior spinal fusion avoids the possible hazards of
breaching the thoracic or abdominal cavities. Additionally, the
pedicle screw, the strongest part of the vertebral body, provides
three-dimensional correction and stabilization, which is much
stronger than anterior instrumentation. This approach, however,
destroys the posterior spinal column, resulting in spinal
instability (19).
In 1983, Denis (20)
first described the three-column model concept of the spine to
elucidate the instability of spinal trauma. Biomechanical and
pathomechanical studies have demonstrated that intact middle and
posterior column structures play a key role in spinal stability
(21). Xie et al (22) noted that the posterior spinal column
was critical for maintaining spinal stability and resistance to
shear force and rotational force. Similarly, Degreif et al
(23) reported that laminectomy
caused 27% rotational stability loss. Therefore, a surgical
approach that causes minimal structural damage to the posterior
spinal column is of great clinical significance for preventing
postoperative complications in the treatment of spinal TB.
Raimondi et al (24)
first described lamina replacement following an intraspinal
approach in 1976. More recently, several studies reported the
usefulness of lamina reconstruction for treating spinal or spinal
cord injury, achieving good clinical and biomechanical outcomes
(25,26). In the present study, the method of
lamina reconstruction based on one-stage posterior debridement,
limited decompression, bone grafting and internal fixation was used
to treat monosegmental spinal TB in group A and good clinical
efficacy was achieved. There were significant differences between
the loss of correction and angle loss rate of groups A and B. Angle
correction in group A was retained more satisfactorily than that in
group B, with only 2.0° Cobb angle loss, which is better than the
result of Louw et al (3.3°) (27).
Additionally, the fusion time of bone grafts in group A was shorter
than that in group B, reducing the risk of failure of internal
fixation. There was extraction of internal fixation in two group B
patients but not in group A patients.
Chandler et al (28) indicated that considerable scar tissue
filled the gap following laminectomy, forming a scar tissue
membrane layer, and abnormal proliferation of fibrous connective
tissue often adhered to the dural sac and nerve root, causing a
sequence of nerve compression symptoms. The formation of scar
tissue would eventually lead to failed back surgery syndrome,
affecting the patient's life adversely (29,30). An
effective and safe mechanical barrier, lamina reconstruction forms
a relatively enclosed environment, preventing invasion and
suppression by posterior organization. It effectively overcame the
drawback of dural sac compression resulting from hematoma and
organization formation following the implantation of other
materials. Compared with the results in group B, a better quality
of life of the patients in group A, reflected by the ODI, was
achieved following surgery. The ODI decrease in group A was more
significant than that in group B.
The difficulty underlying the use of this approach
to treat spinal TB stems from whether such an approach can achieve
complete focal debridement, and how the reconstructed lamina can be
prevented from subsiding into the spinal canal. The approach offers
no advantage in terms of debridement; however, with the development
of effective anti-TB drugs, tuberculous lesions may be successfully
treated through spontaneous fusion, and complete debridement is not
unduly emphasized (31,32). To prevent subsidence of the
reconstructed lamina, it was attached to the vertebral plate
adjacent to the lesion during the surgery.
The six factors constituting the main advantages
this approach has over other methods include that: i) It minimizes
damage to spinal stability, overcoming the shortcomings of a large
fixation range and retaining more motor units of the spine. ii)
Satisfactory Cobb angle correction can be achieved, with less angle
loss and assurance of spinal stability. iii) It effectively
prevents postoperative instability, subluxation and kyphotic
deformities. iv) The technique allows conservation of the bone
protecting the spinal cord and prevents epidural adhesion following
laminectomy. v) Lamina replantation enables muscle and soft tissue
attachment, increasing postoperative paraspinal muscle function.
vi) The procedure can also relieve spinal nerve compression, reduce
trauma for patients, and improve their quality of life more
effectively.
There are limits to this procedure, however. Based
on experience, the indications for the method are as follows: i)
Cases with monosegmental TB or single vertebral TB; ii) paraspinal
abscess confined to one segment; and iii) Cobb angle of the lesion
<45°. Conversely, the procedure cannot be performed in the
following situations: i) multi-segmental vertebral TB; ii)
multi-level non-contiguous spinal TB; iii) paraspinal abscess
diffused across two segments or accompanied by psoas abscess or
iliac fossa abscess; and iv) case combined with complete
paraplegia.
Due to controversy regarding the treatment of spinal
TB, each case should be considered individually. When formulating a
successful surgical plan, practitioners should consider the
severity of the disease, individual patient differences and
available surgical expertise and facilities.
In conclusion, surgical treatment involving
one-stage posterior limited decompression, bone grafting and
internal fixation combined with lamina reconstruction can be an
effective treatment method for monosegmental thoracic and lumbar
TB. This method can lead to the effective recovery of posterior
spinal column integrity, improve neurological function and reduce
postoperative complications. Thus far, the clinical and
radiographic results of the patients are good. However, these are
preliminary results from a small study population and certain
patients had a relatively short follow-up. Future investigations
with a larger number of patients and a longer follow-up is
required.
Acknowledgements
This study was partially funded by the National
Natural Science Foundation of China (no. 81171736).
References
|
1
|
Chen WJ, Chen CH and Shih CH: Surgical
treatment of tuberculous spondylitis. 50 patients followed for 2–8
years. Acta Orthop Scand. 66:137–142. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Garst RJ: Tuberculosis of the spine: a
review of 236 operated cases in an underdeveloped region from 1954
to 1964. J Spinal Disord. 5:286–300. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Gautam MP, Karki P, Rijal S and Singh R:
Pott's spine and paraplegia. JNMA J Nepal Med Assoc. 44:106–115.
2005.PubMed/NCBI
|
|
4
|
Fuentes Ferrer M, Gutiérrez Torres L,
Ayala Ramírez O, Rumayor Zarzuelo M and del Prado González N:
Tuberculosis of the spine. A systematic review of case series. Int
Orthop. 36:221–231. 2012.
|
|
5
|
Cavuşoğlu H, Kaya RA, Türkmenoğlu ON,
Tuncer C, Colak I and Aydin Y: A long-term follow-up study of
anterior tibial allografting and instrumentation in the management
of thoracolumbar tuberculous spondylitis. J Neurosurg Spine.
8:30–38. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Moon MS, Moon YW, Moon JL, Kim SS and Sun
DH: Conservative treatment of tuberculosis of the lumbar and
lumbosacral spine. Clin Orthop Relat Res. 398:40–49. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Rajasekaran S and Shanmugasundaram TK:
Prediction of the angle of gibbus deformity in tuberculosis of the
spine. J Bone Joint Surg Am. 69:503–509. 1987.PubMed/NCBI
|
|
8
|
Rajasekaran S: The natural history of
post-tubercular kyphosis in children. Radiological signs which
predict late increase in deformity. J Bone Joint Surg Br.
83:954–962. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Jain AK: Tuberculosis of the spine: a
fresh look at an old disease. J Bone Joint Surg Br. 92:905–913.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
McDonnell MF, Glassman SD, Dimar JR II,
Puno RM and Johnson JR: Perioperative complications of anterior
procedures on the spine. J Bone Joint Surg Am. 78:839–847.
1996.PubMed/NCBI
|
|
11
|
Ikard RW: Methods and complications of
anterior exposure of the thoracic and lumbar spine. Arch Surg.
141:1025–1034. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Garg B, Kandwal P, Nagaraja UB, Goswami A
and Jayaswal A: Anterior versus posterior procedure for surgical
treatment of thoracolumbar tuberculosis: A retrospective analysis.
Indian J Orthop. 46:165–170. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Lee CK, Vessa P and Lee JK: Chronic
disabling low back pain syndrome caused by internal disc
derangements. The results of disc excision and posterior lumbar
interbody fusion. Spine. 20:356–361. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zhang HQ, Li JS, Zhao SS, Shao YX, Liu SH,
Gao Q, Lin MZ, Liu JY, Wu JH and Chen J: Surgical management for
thoracic spinal tuberculosis in the elderly: posterior only versus
combined posterior and anterior approaches. Arch Orthop Trauma
Surg. 132:1717–1723. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Moon MS: Tuberculosis of the spine.
Controversies and a new challenge. Spine. 22:1791–1797. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Moon MS, Woo YK, Lee KS, Ha KY, Kim SS and
Sun DH: Posterior instrumentation and anterior interbody fusion for
tuberculous kyphosis of dorsal and lumbar spines. Spine.
20:1910–1916. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lee SH, Sung JK and Park YM: Single-stage
transpedicular decompression and posterior instrumentation in
treatment of thoracic and thoracolumbar spinal tuberculosis: a
retrospective case series. J Spinal Disord Tech. 19:595–602. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Talu U, Gogus A, Ozturk C, Hamzaoglu A and
Domanic U: The role of posterior instrumentation and fusion after
anterior radical debridement and fusion in the surgical treatment
of spinal tuberculosis: experience of 127 cases. J Spinal Disord
Tech. 19:554–559. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Jarrett CD, Heller JG and Tsai L: Anterior
exposure of the lumbar spine with and without an ‘access surgeon’:
morbidity analysis of 265 consecutive cases. J Spinal Disord Tech.
22:559–564. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Denis F: The three column spine and its
significance in the classification of acute thoracolumbar spinal
injuries. Spine. 8:817–831. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Ogden AT, Bresnahan L, Smith JS, Natarajan
R and Fessler RG: Biomechanical comparison of traditional and
minimally invasive intradural tumor exposures using finite element
analysis. Clin Biomech (Bristol, Avon). 24:143–147. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Xie J, Li T, Wang Y, Zhao Z, Zhang Y and
Bi N: Change in Cobb angle of each segment of the major curve after
posterior vertebral column resection (PVCR): a preliminary
discussion of correction mechanisms of PVCR. Eur Spine J.
21:705–710. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Degreif J, Wenda K, Runkel M and Ritter G:
Rotational stability of the thoracolumbar spine after interlaminar
ultrasound window, hemilaminectomy and laminectomy. A comparative
experimental study. Unfallchirurg. 97:250–255. 1994.[(In German)].
PubMed/NCBI
|
|
24
|
Raimondi AJ, Gutierrez FA and Di Rocco C:
Laminotomy and total reconstruction of the posterior spinal arch
for spinal canal surgery in childhood. J Neurosurg. 45:555–560.
1976. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Matsui H, Kanamori M and Miaki K:
Expansive laminoplasty for lumbar intradural lipoma. Int Orthop.
21:185–187. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Shikata J, Yamamuro T, Shimizu K and Saito
T: Combined laminoplasty and posterolateral fusion for spinal canal
surgery in children and adolescents. Clin Orthop Relat Res.
259:92–99. 1990.PubMed/NCBI
|
|
27
|
Louw JA: Spinal tuberculosis with
neurological deficit. Treatment with anterior vascularised rib
grafts, posterior osteotomies and fusion. J Bone Joint Surg Br.
72:686–693. 1990.PubMed/NCBI
|
|
28
|
Chandler K and Cappello R: Laminectomy
membrane formation in dogs: is the answer still elusive? Vet J.
172:1–2. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Ross JS, Robertson JT, Frederickson RC,
Petrie JL, Obuchowski N, Modic MT and deTribolet N: Association
between peridural scar and recurrent radicular pain after lumbar
discectomy: magnetic resonance evaluation. ADCON-L European Study
Group. Neurosurgery. 38:855–861; discussion 861–863. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Fritsch EW, Heisel J and Rupp S: The
failed back surgery syndrome: reasons, intraoperative findings, and
long-term results: a report of 182 operative treatments. Spine.
21:626–633. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Pande KC and Babhulkar SS: Atypical spinal
tuberculosis. Clin Orthop Relat Res. 398:67–74. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Rajasekaran S: The problem of deformity in
spinal tuberculosis. Clin Orthop Relat Res. 398:85–92. 2002.
View Article : Google Scholar : PubMed/NCBI
|