Introduction
Acute subdural hematoma is a major life-threatening
condition with a mortality rate of 60–80% (1). Subdural hematomas require immediate and
aggressive treatment. The main surgical approach is to perform a
craniotomy, which involves removing part of the skull, followed by
drainage of the hematoma and reattachment of the skull fragment
(2). Decompressive craniectomy also
involves removing part of the skull to relieve intracranial
pressure; however, the part of the skull that is removed is not
generally replaced (2). Although
craniotomies and craniectomies are frequently used for the
treatment of acute subdural hematomas, a major limitation of their
use is that these surgical techniques are associated with high
mortality rates (3,4). Preoperative trepanation and drainage,
in which a burr hole is created in the skull to reduce pressure,
may improve surgical outcomes or, in some cases, reduce the need
for follow-up surgical care (5).
This approach may be particularly valuable for patients who present
with comorbidities or cannot endure highly invasive surgical
procedures. In the present study, two cases of elderly patients
with acute subdural hematomas treated by preoperative trepanation
and drainage are reported.
Case reports
Case 1
An 86-year-old male patient developed a sudden
headache followed by nausea and vomiting with gradual loss of
consciousness. In transit to the Shenyang General Hospital
(Shenyang, China), the patient developed cerebral herniation with
right and left mydriases of 6.0 mm and 2.0 mm, respectively. The
patient was initially admitted to the Emergency Department for
acute subdural hematoma and later transferred to the intensive care
unit of the Neurological Department. The patient was deeply
comatose at the time of admission with a Glasgow Coma Scale (GCS)
score of 5, with no eye movement or light reflex. The left pupil
diameter was 2.0 mm and the right pupil diameter was 5.5 mm.
Limb-muscle strength was grade II with normal muscle tension (MRC
grading system) (6), and a
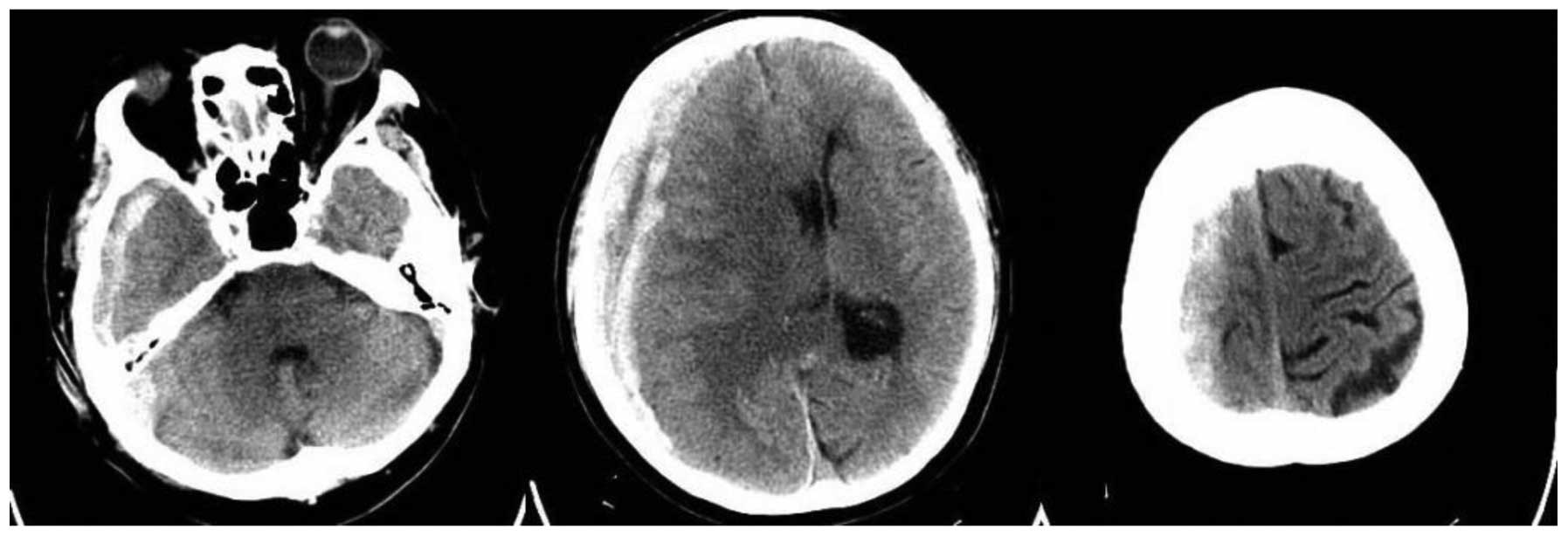
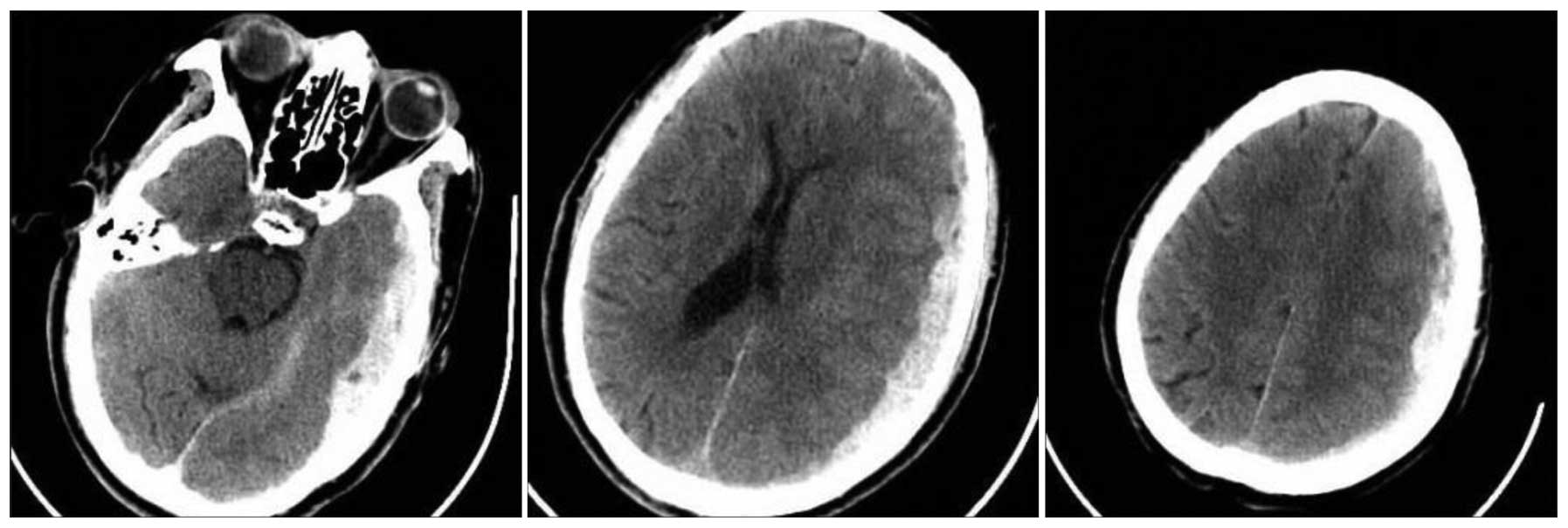
pathological reflex was not elicited. Computed tomography (CT)
images of the head are shown in Fig.
1.
Due to the instability of the vital signs, an
emergency surgery was required to remove the hematoma. Family
members of the patient did not support a decompressive craniectomy
with general anesthesia being performed but agreed to burr-hole
drainage for subdural hematoma on the right frontal, temporal and
parietal regions using local anesthesia.
After informed consent was obtained from the
patients' families, local anesthesia was administered and 1.0-cm
surgical incisions were created at the centers of the thickest
hematoma regions in the right parietal and temporal lobes. Two 1-cm
burr holes were drilled until an outflow of dark red, bloody fluid
was achieved. A drainage tube (10#; diameter, 3 mm) was placed into
the hematomal cavity and the incision was subsequently sutured and
closed. The drainage tube was connected to a sterile drainage bag,
and the incision was covered with sterile dressing. The
postoperative drainage tubes were patent and the patient exhibited
stable vital signs following surgery. The GCS score was 4 and the
pupil diameters remained unequal at 6.0 and 2.0 mm in the right and
left eye, respectively. The light reflex remained absent. A
postoperative subdural injection of urokinase (5×104 IU)
accelerated the dissolution of the intracranial hematoma. The
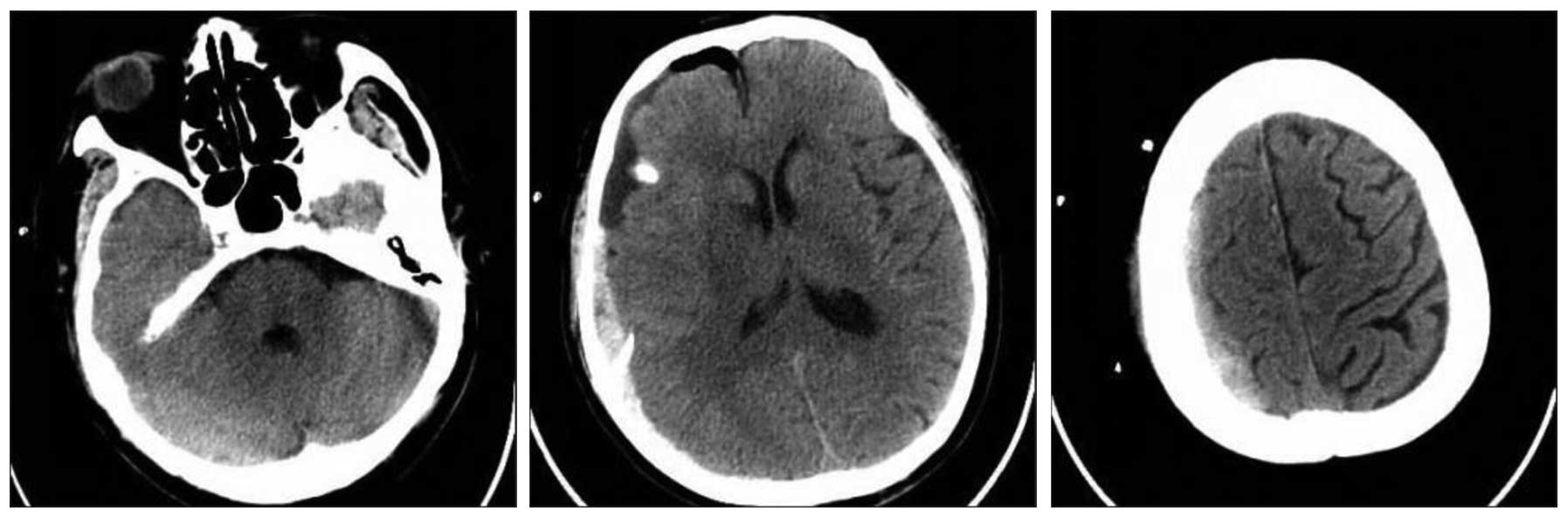
postoperative CT images are presented in Fig. 2.
On postoperative day 1, the patient was comatose
with a GCS score of 5. The patient showed no eye movement and had
retarded light reflex in the left pupil at 2.0 mm, and areflexia in
the right pupil at 5.0 mm. The dehydration drug Mannitol (Shanghai
Baxter Healthcare Co., Ltd., Shanghai, China) was administered in
three 250-ml doses and urokinase was injected into the secondary
hematoma cavity to drain the hematoma. The patient was drowsy on
postoperative day 3 and pupil diameters remained unequal at 2.0 mm
in the left eye and 6.0 mm in the right eye. Furthermore, the light
reflex remained retarded in the left pupil with areflexia in the
right pupil. On postoperative day 4, the patient exhibited a degree
of unconsciousness with a GCS score between 5–8. Urokinase was
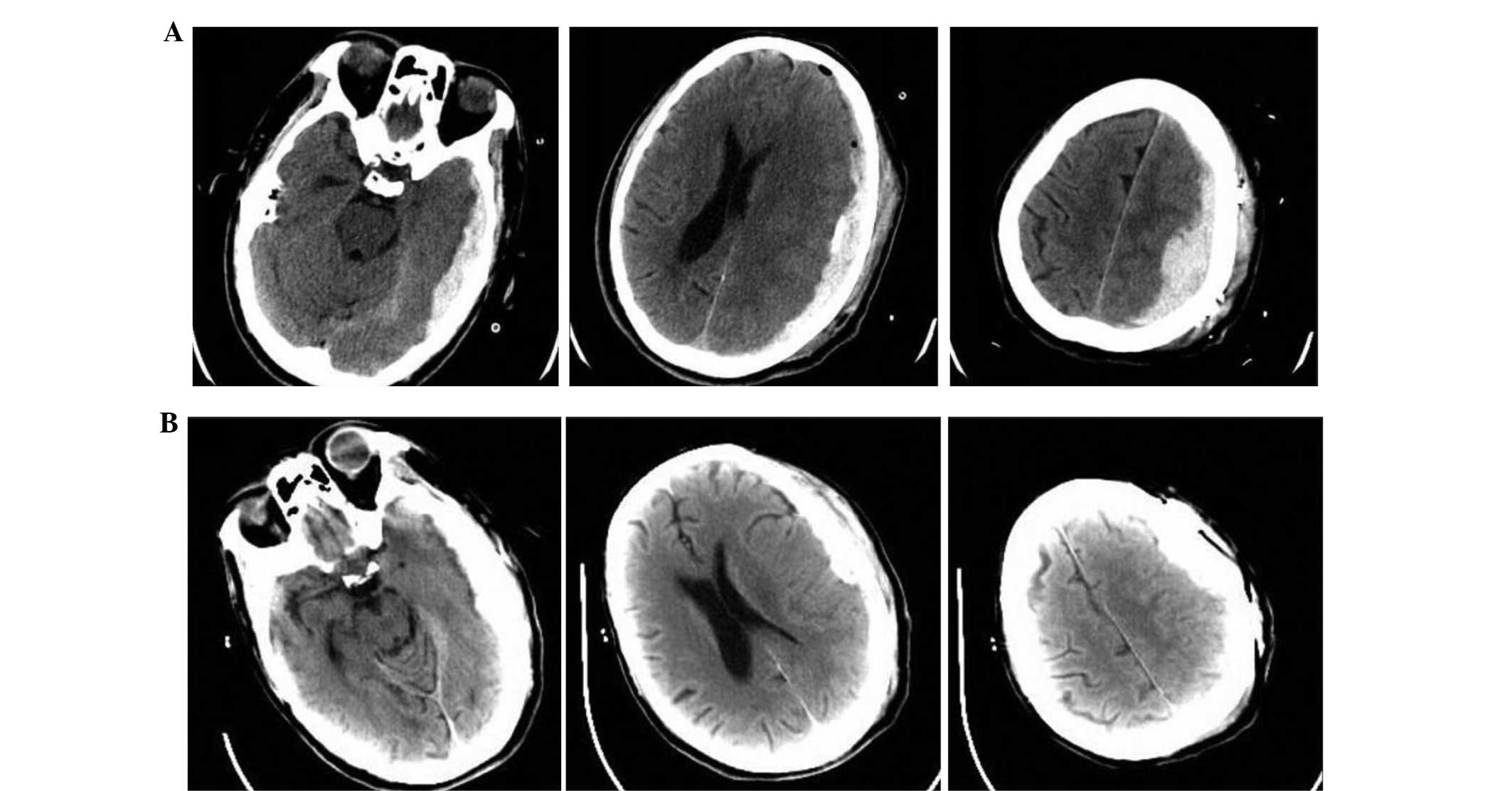
injected into the hematomal cavity. CT images of the head on
postoperative day 4 are shown in Fig.
3A. Hypoalbuminemia and a significantly increased inflammatory
cell count were noted on postoperative day 5. Elevated sodium and
reduced potassium levels were also observed but were corrected.
Sodium levels were corrected by administering the patient drinking
water, while potassium levels were normalized via the intravenous
administering of potassium. CT images showed no abnormalities on
postoperative day 6 (Fig. 3B). On
postoperative day 9, the patient exhibited a degree of
unconsciousness (GSC score 5–8) and had excessive levels of sputum.
A percutaneous tracheal atherectomy was performed and head CT scans
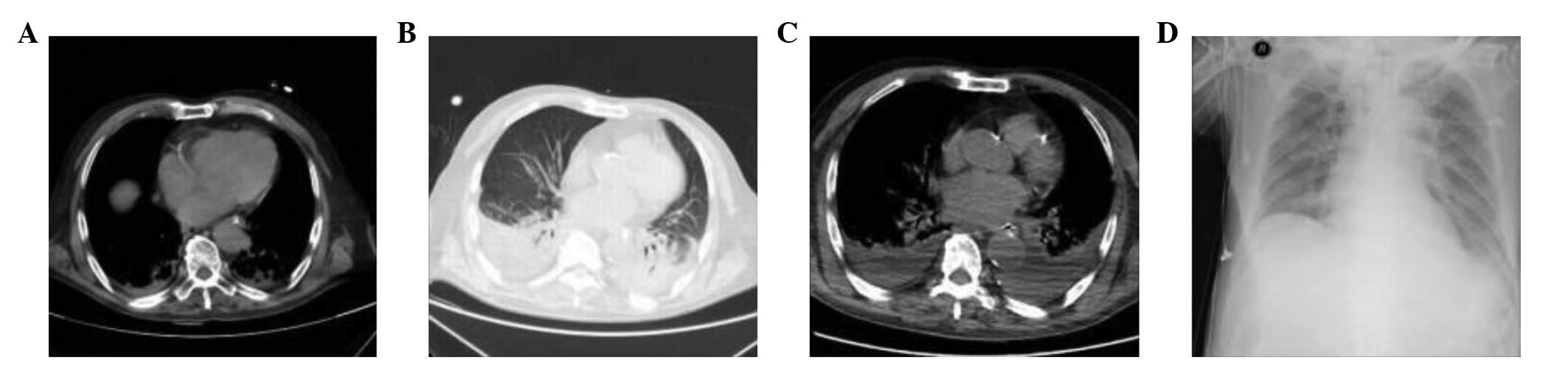
were obtained (Fig. 3C). On day 26
following admission, the patient showed faint signs of
consciousness with stable vital signs and head images. However,
serious lung inflammation (Fig. 4)
required continuous intervention with three 4.5-g doses of
piperacillin/tazobactam (Qingzhou Yaowang Medicine Co., Ltd.,
Weifang, Shandong, China) by the Department of Respiratory
Medicine. The patient regained consciousness, showed signs of
recovery and was discharged on day 48 after admission.
Case 2
A 74-year-old male patient developed transient chest
pain and was admitted to the Shenyang General Hospital for further
treatment following an unspecified drug treatment at a different
hospital. The patient had been diagnosed with coronary artery
disease and myocardial infarction with an acute non-ST segment
elevation 3 years previously. There was no history of hypertension,
diabetes mellitus or cerebrovascular disease. The patient was
diagnosed with coronary atherosclerotic heart disease with unstable
angina, old anterior myocardial infarction and cardiac function
level II (New York Heart Association class) (7) at the time of admission. A single 100-mg
dose of aspirin (Bayer AG, Leverkusen, Germany) was administered as
an anti-platelet therapy, resulting in protection of the gastric
mucosa, adjustment of the levels of blood fat, improved blood
circulation, controlled heart rate, decreased myocardial oxygen
consumption, dilated coronary arteries and reduced cardiac
stress.
Coronary angiography showed 99% occlusion of the
proximal and middle right coronary artery with the appearance of
bridge collaterals on day 3 following admission. Furthermore,
complete (100%) occlusion of the distal left circumflex artery and
90–95% stenosis of the proximal and middle left anterior descending
artery was observed. The Thrombolysis in Myocardial Infarction
(TIMI) score was 2–3 (8). Septal
branches extended to the left circumflex artery and obtuse marginal
branches to form a coarse two-level collateral circulation. The
family of the patient requested coronary-artery bypass
grafting.
The patient was scheduled for surgery and
preoperative preparations by the Department of Cardiac Surgery on
day 5 after admission. However, the patient developed a fever of
37.6°C and 0.5 g paracetamol (Southwest Pharmaceutical Co., Ltd.,
Chongqing, China) was administered orally as an antipyretic. The
patient developed sudden slurring of speech, lethargy, and
right-limb movement disorder by the next day (day 6 after
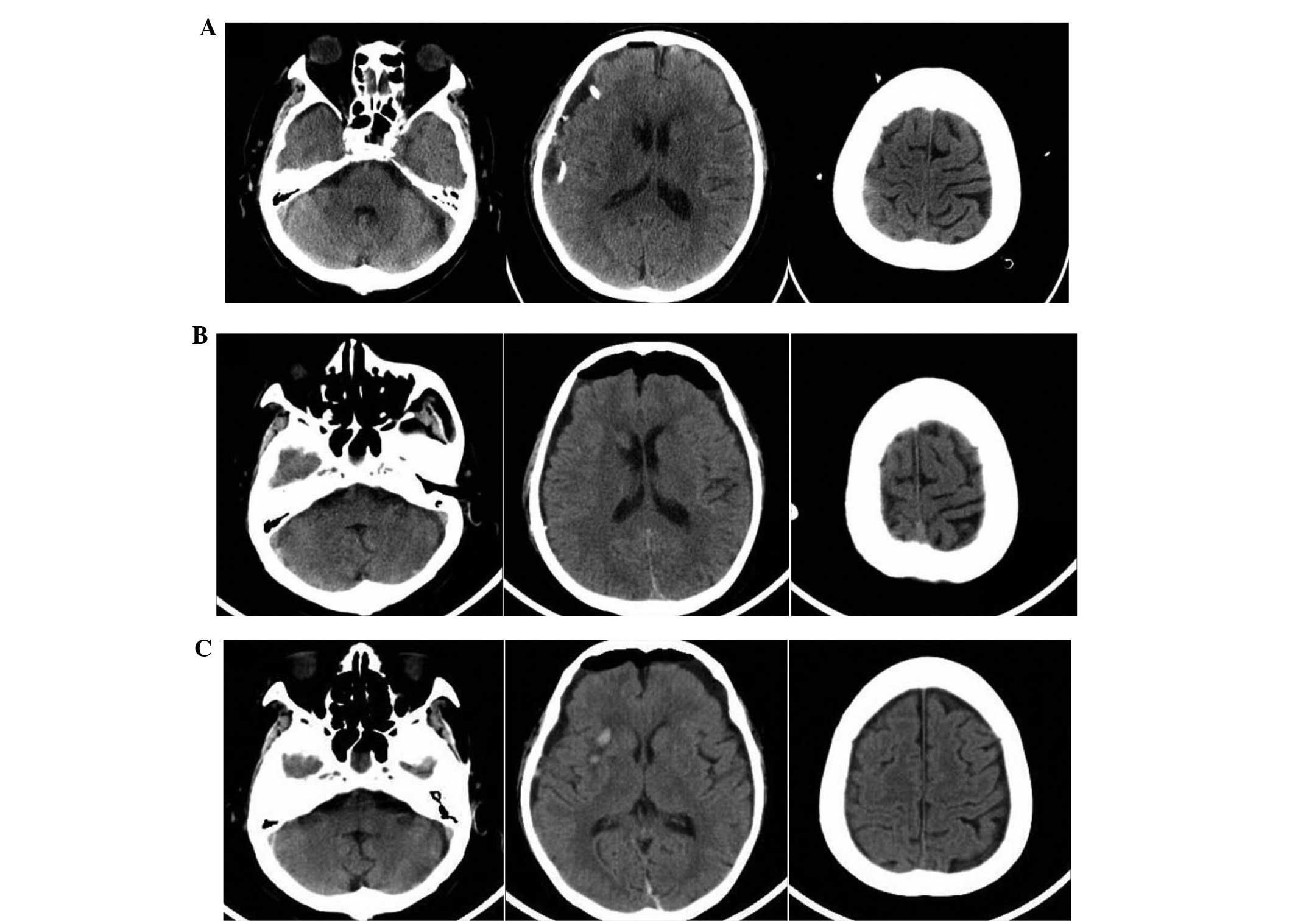
admission). Cranial CT scans showed the presence of a left-sided
subdural hematoma (Fig. 5). The
patient was transferred to the intensive care unit of the
Neurosurgery Department. The family of the patient did not allow
the medical team to perform a decompressive craniectomy with
general anesthesia. However, following additional discussions, the
family consented to burr-hole drainage with local anesthesia as a
treatment for the left subdural hematoma.
The patient showed faint consciousness on day 6
after admission. Burr-hole drainage was performed and surgical
incisions were created at the centers of the thickest regions of
the hematoma in the left parietal lobe to expose the dura, which
was dark blue and showed a high degree of tension. Following
fulguration, a cross-shaped incision was created to open the dura
until an outflow of ~20 ml of dark red, bloody fluid was achieved.
A 10# pipe was placed into the hematomal cavity followed by washout
with normal saline. The incision was sutured and closed layer by
layer. The drainage tube was rinsed with an ample amount of normal
saline until the saline was clear; the tube was subsequently
connected to a sterile drainage bag. A further incision was created
in the left temporal lobe as described above. The patient was in a
coma on the day of surgery with a GCS score of 7 and equal pupil
diameters of 1.5 mm each. Furthermore, the patient exhibited a
retarded light reflex, tingling of the limbs and bilateral negative
pathological signs. Postoperative seizures occurred several times
and valproate and sedative drugs (propofol, 20 mg/h; Fresenius
Kabi, Bad Bomburg, Germany) were administered in combination due to
concerns of vasospasms and transient convulsions secondary to
reduced intracranial pressure. Postoperative CT imaging was
performed (Fig. 6A).
The GCS score was 7 on days 1–4 following surgery, 9
on days 5–12 and ranged from 10 to 14 on days 12–18. Subdural
injection of urokinase was performed on postoperative days 1 and 2
to accelerate clot dissolution. The patient received a tracheotomy
on postoperative day 3. On postoperative day 5, the white-blood
cell (WBC) count was 28.6×109/l. The subdural hematoma
was clearly reduced on CT scans (Fig.
6B); thus, the drainage tube was removed. Serum sodium was
elevated to 150.9 mmol/l on postoperative day 6; serum potassium
was 2.86 mmol/l; and the WBC count was 29.7×109/l. The
patient was required to drink more water to reduce the levels of
serum in the blood, and potassium levels were increased by
intravenuous injections. Sputum cultures showed the presence of
Acinetobacter baumannii and Klebsiella pneumoniae. A
total of 2.0 g of the antibiotic meropenem was administered every 8
h for 2 weeks. Routine blood tests performed on postoperative day 7
showed reduced serum levels of prealbumin (129 mg/l) and albumin
(35.3 g/l), increased serum levels of sodium (157.1 mmol/l), and an
increased neutrophil percentage (87.9%) and neutrophil count
(21.0×109/l). Routine blood tests on postoperative day 8
showed a decreased WBC count (13.6×109/l) as well as
increased levels of globulin f (30.80 g/l), sodium (150.4 mmol/l)
and potassium (3.25 mmol/l). Potassium supplements were
administered to the patient and the hypernatremia was corrected. On
postoperative day 9, the WBC count remained at
13.6×109/l; however, the levels of sodium and potassium
ions returned to normal. The postsurgical wound healed well. The
WBC count gradually returned to normal between postoperative days
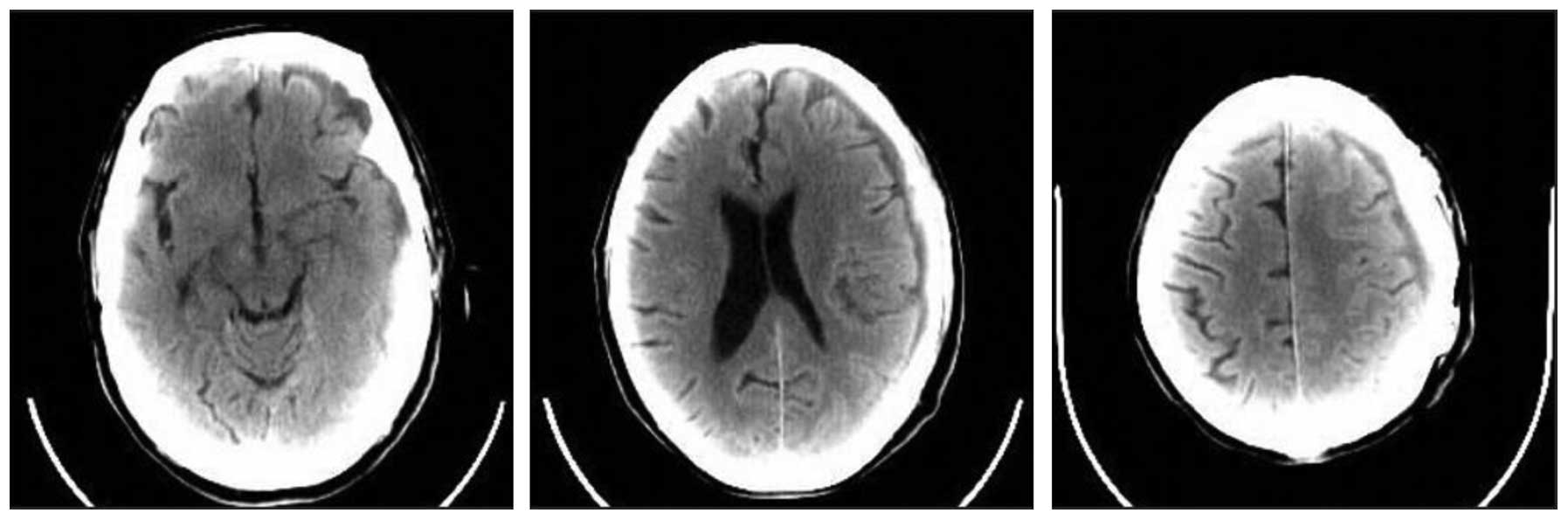
10–18. The patient was discharged on postoperative day 18; head CT
images performed at the time of discharge are shown in Fig. 7.
Discussion
The present study reported two cases in which
elderly patients benefited from trepanation and drainage of an
acute subdural hematoma. In all cases, the families of the patients
refused to consent to surgery; thus, burr-hole drainage was
selected as an alternative option for relieving intracranial
pressure. A number of studies have demonstrated that the timing of
surgical intervention is a major determinant of the outcome of
subdural hematoma treatment (4,9). The
recommended timing for evacuation of a hematoma is within 4 h of
onset; delays past this critical window of time are associated with
neuronal loss and poorer outcomes in a number of neurological
conditions, including subdural hematomas and strokes (4,10).
Trepanation and drainage is a rapid method for stabilizing a
patient with an early-stage subdural hematoma who is unable to
receive surgery in a timely manner. However, drainage through a
burr hole may only be an option during the first few hours of
developing a subdural hematoma, as coagulation may eventually
prevent blood flow through the burr hole (11). Patients who are cotreated with
anticoagulants may show more favorable treatment results with
trepanation, as these medications may maintain steady blood flow
and an open drainage tube, thereby relieving intracranial pressure
(12). In a previous study, the
insertion of a subdural evacuating port system with subsequent
drainage of a subdural hemorrhage and a craniotomy resulted in a
favorable neurological outcome and recovery for the patient
(11). Thus, the option of
trepanation and drainage may be suitable for patients who cannot
immediately receive surgery. However, the benefit must always be
weighed against potential disadvantages, which include the
potential for infection associated with the burr hole, as shown in
the present study with case 2. In case 2, the adverse event was
successfully managed with medication. Another potential
disadvantage of burr-hole drainage is that it may further delay
surgery (12). These risks need to
be weighed carefully when considering whether trepanation with
drainage is an option for a patient.
In the current study, case 1 presented a relatively
low GCS score of 4 at the time of admission to the hospital.
Initial GCS scores at the time of admission have previously been
associated with mortality rate (13). In one study, GCS scores <3 were
associated with a 93% mortality rate in patients with acute
subdural hematomas (14). Patients
in the study who had GCS scores between 4 and 6 demonstrated
mortality rates ranging from 45 to 67%, and all patients with GCS
scores ≥7 survived (14). Another
study reported a 74% mortality rate for those with GCS scores
between 3 and 5 (15). In addition
to GCS score, age is a major determinant of outcome from acute
subdural hematoma. It is estimated that the probability of a poor
outcome increases by 40–50% with every decade of life (13). Furthermore, mortality appears to be 4
times more likely in patients who are ≥65 years of age than in
adults who are <40 years of age (13). Another factor that may favorably
influence outcome is whether the patient is treated in a dedicated
neurosurgical department (13), as
occurred in the cases discussed in the present study. Based on the
associations between age and GCS score with mortality rate, the
favorable outcomes of the cases reported in the current study
suggest that trepanation with drainage may be a promising treatment
approach for elderly patients, including those with low GCS scores.
Future trials should be performed to determine if preoperative
burr-hole drainage can effectively improve the outcome and reduce
the mortality rate in elderly patients with acute subdural
hematomas.
References
|
1
|
Park JY, Moon KS, Lee JK and Jeung KW:
Rapid resolution of acute subdural hematoma in child with severe
head injury: a case report. J Med Case Rep. 7:672013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Chen SH, Chen Y, Fang WK, Huang DW, Huang
KC and Tseng SH: Comparison of craniotomy and decompressive
craniectomy in severely head-injured patients with acute subdural
hematoma. J Trauma. 71:1632–1636. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Li LM, Kolias AG, Guilfoyle MR, Timofeev
I, Corteen EA, Pickard JD, Menon DK, Kirkpatrick PJ and Hutchinson
PJ: Outcome following evacuation of acute subdural haematomas: a
comparison of craniotomy with decompressive craniectomy. Acta
Neurochir (Wien). 154:1555–1561. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Paci GM, Sise MJ, Sise CB, Sack DI,
Shackford SR, Kureshi SA, Osler TM, Yale RS, Riccoboni ST, Peck KA
and O'Reilly EB: Preemptive craniectomy with craniotomy: what role
in the management of severe traumatic brain injury? J Trauma.
67:531–536. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Mondorf Y, Abu-Owaimer M, Gaab MR and
Oertel JM: Chronic subdural hematoma - craniotomy versus burr hole
trepanation. Br J Neurosurg. 23:612–616. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Chisari C, Bertolucci F, Dalise S and
Rossi B: Chronic muscle stimulation improves muscle function and
reverts the abnormal surface EMG pattern in myotonic dystrophy: A
pilot study. J Neuroeng Rehabil. 10:942013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Johnson MJ, Bland JM, Davidson PM, et al:
The relationship between two performance scales: New York Heart
Association Classification and Karnofsky Performance Status Scale.
J Pain Symptom Manage. 47:652–658. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Amin ST, Morrow DA, Braunwald E, et al:
Dynamic TIMI risk score for STEMI. J Am Heart Assoc. 2:e0032692013.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Bulters D and Belli A: A prospective study
of the time to evacuate acute subdural and extradural haematomas.
Anaesthesia. 64:277–281. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Saver JL: Time is brain - quantified.
Stroke. 37:263–266. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Flint AC, Gean AD, Manley GT, et al:
Temporizing treatment of hyperacute subdural hemorrhage by subdural
evacuation port system placement. J Neurosurg. 115:844–848. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sagher O: Acute subdural hematoma. J
Neurosurg. 115:8422011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Leitgeb J, Mauritz W, Brazinova A, Janciak
I, Majdan M, Wilbacher I and Rusnak M: Outcome after severe brain
trauma due to acute subdural hematoma. J Neurosurg. 117:324–333.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Hatashita S, Koga N, Hosaka Y and Takagi
S: Acute subdural hematoma: severity of injury, surgical
intervention and mortality. Neurol Med Chir (Tokyo). 33:13–18.
1993. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Gennarelli TA, Spielman GM, Langfitt TW,
Gildenberg PL, Harrington T, Jane JA, Marshall LF, Miller JD and
Pitts LH: Influence of the type of intracranial lesion on outcome
from severe head injury. J Neurosurg. 56:26–32. 1982. View Article : Google Scholar : PubMed/NCBI
|