Introduction
Kawasaki disease (KD), also known as mucocutaneous
lymph node syndrome, is an acute disease that predominantly affects
children. The primary pathological characteristics of the condition
are fever and rash due to systemic vasculitis (1–3). KD
mainly affects children aged between 6 months and 4 years (4). In developed countries KD is the most
common cause of acquired heart disease in childhood (5,6). The
etiology of KD has yet to be elucidated, although it is believed to
be associated with the induction of an intense inflammatory host
response in genetically susceptible individuals by at least one
infectious agent (7,8).
An epidemiological survey conducted in California
between 1995 and 1999 (9) observed
an increasing trend in the incidence of KD in patients aged <5
years from 1997. The incidence of KD was highest among Asian
individuals, but was not associated with temperature, precipitation
rates, family size or population density (9). More recent reports have revealed
changes in the clinical characteristics of KD (10–12),
with a study by Kang et al (13) indicating an increase in the
proportion of cases of incomplete KD. This increase, as well as a
decrease in the incidence of coronary artery lesions, was
attributed to the early admission and management of patients with
KD. The authors suggested that a diagnostic strategy for incomplete
KD should be established irrespective of the presence of coronary
lesions (13). Katsumata et
al (14) reported the
characteristics of cervical computed tomography findings in KD:
They indicated that retropharyngeal lymphadenopathy and
retropharyngeal edema are relatively common features of KD on CT.
The more characteristics of this disease that are identified, the
more help in the diagnosis and treatment of KD.
In order to enhance the understanding of the
development of this disease in our local region, we performed a
retrospective study of children with KD who were admitted to the
People's Hospital of Inner Mongolia (Huhhot, China) over a 10-year
period with the aim of summarizing the clinical characteristics of
the condition and exploring the dynamic changes of the disease over
time.
Patients and methods
Patients and diagnosis
This retrospective study was conducted in the
People's Hospital of Inner Mongolia, China. The medical records of
patients diagnosed with KD were reviewed, and information recorded
between January 2003 and December 2012 was analyzed.
A diagnosis of KD was based on the fifth edition of
the KD diagnostic criteria revised by the Japanese Kawasaki
Committee in 2002, as follows (2):
i) Patients with ≥5 of the 6 major symptoms described in the
primary clinical manifestations; ii) patients exhibiting 4 of the
symptoms and either a coronary artery injury or a coronary artery
aneurysm, identified during the clinical period through
two-dimensional echocardiography or coronary angiography, following
the exclusion of other diseases that could also be diagnosed as KD.
Children meeting these diagnostic criteria, including cases
transferred from other hospitals and both typical and atypical
(incomplete KD in children) cases of KD, were accepted for
treatment in the People's Hospital of Inner Mongolia.
The following exclusion criteria were applied: i)
Patients with chronic-phase KD; ii) patients for whom a diagnosis
of KD was incorrect; iii) clinical cases occurring outside the
stated study period (2003–2012). The revised criteria from the
Seventh World Children KD Symposium (15) were referred to for the diagnosis of
coronary artery injury and aneurysms. The diagnosis of coronary
artery injury was based on reference values for the internal
diameter of the coronary artery: Children aged <3 years, ≥2.5
mm; 3–9 years, ≥3 mm; >9 years, ≥3.5 mm. For the diagnosis of
coronary aneurysm, the criteria were as follows: Mild coronary
dilatation, internal diameter ≤4 mm; medium coronary aneurysm,
internal diameter 4–8 mm; large coronary aneurysm, internal
diameter >8 mm.
Clinical and laboratory
parameters
The clinical data for 246 cases with KD were
retrospectively analyzed, and 231 cases were ultimately selected
based on the aforementioned diagnostic, inclusion and exclusion
criteria. The clinical characteristics of the enrolled patients,
including physiological state, treatments, clinical manifestations
and results of the laboratory examination and echocardiography
(coronary artery and other abnormalities), were analyzed. The
dynamic changes in KD were thus observed over the 10-year
period.
Statistical analysis
A database containing the clinical data was
established using Excel software (Microsoft Corp., Redmond, WA,
USA), and statistical analyses were conducted using SPSS 13.0
software (SPSS, Inc., Chicago, IL, USA). Data are presented as the
mean ± standard deviation. Data with a normal distribution were
analyzed with a variance test, while non-normally distributed data
were analyzed with a rank-sum test. Count data were analyzed with a
one-sided χ2 test. P<0.05 was considered to indicate
a statistically significant difference.
Results
Demographic data of recruited
patients
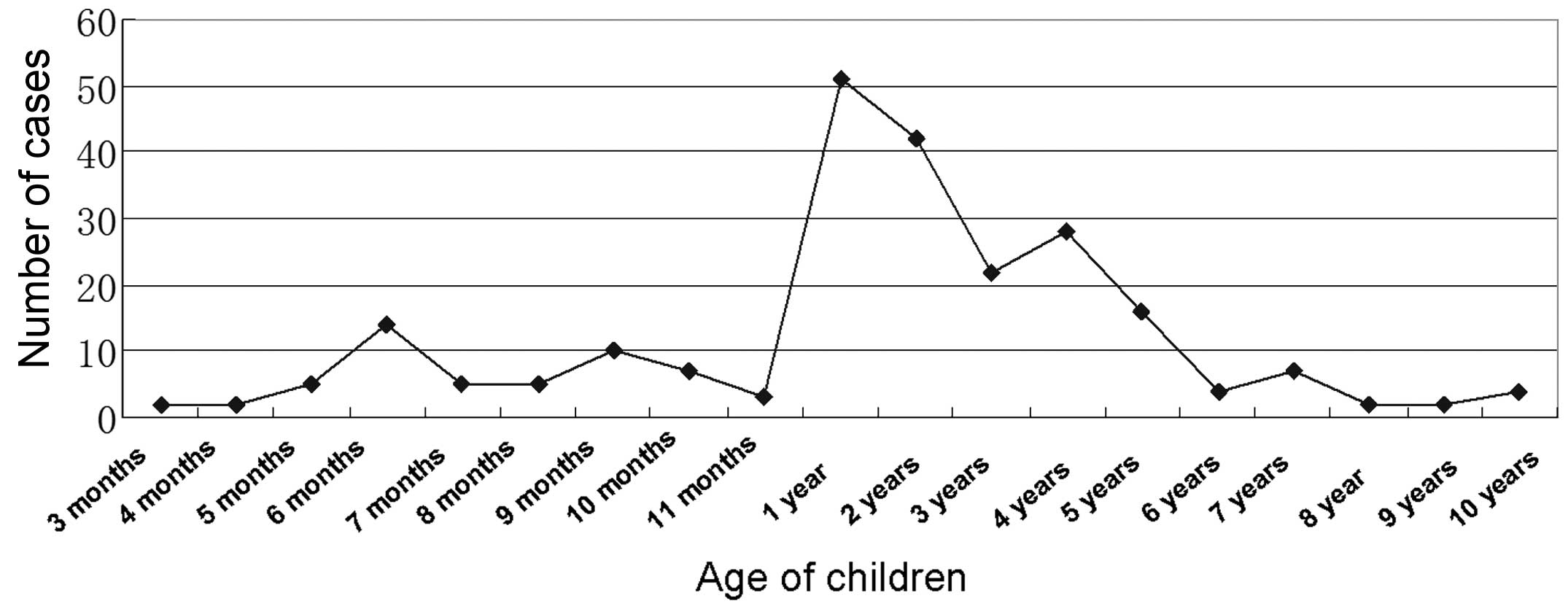
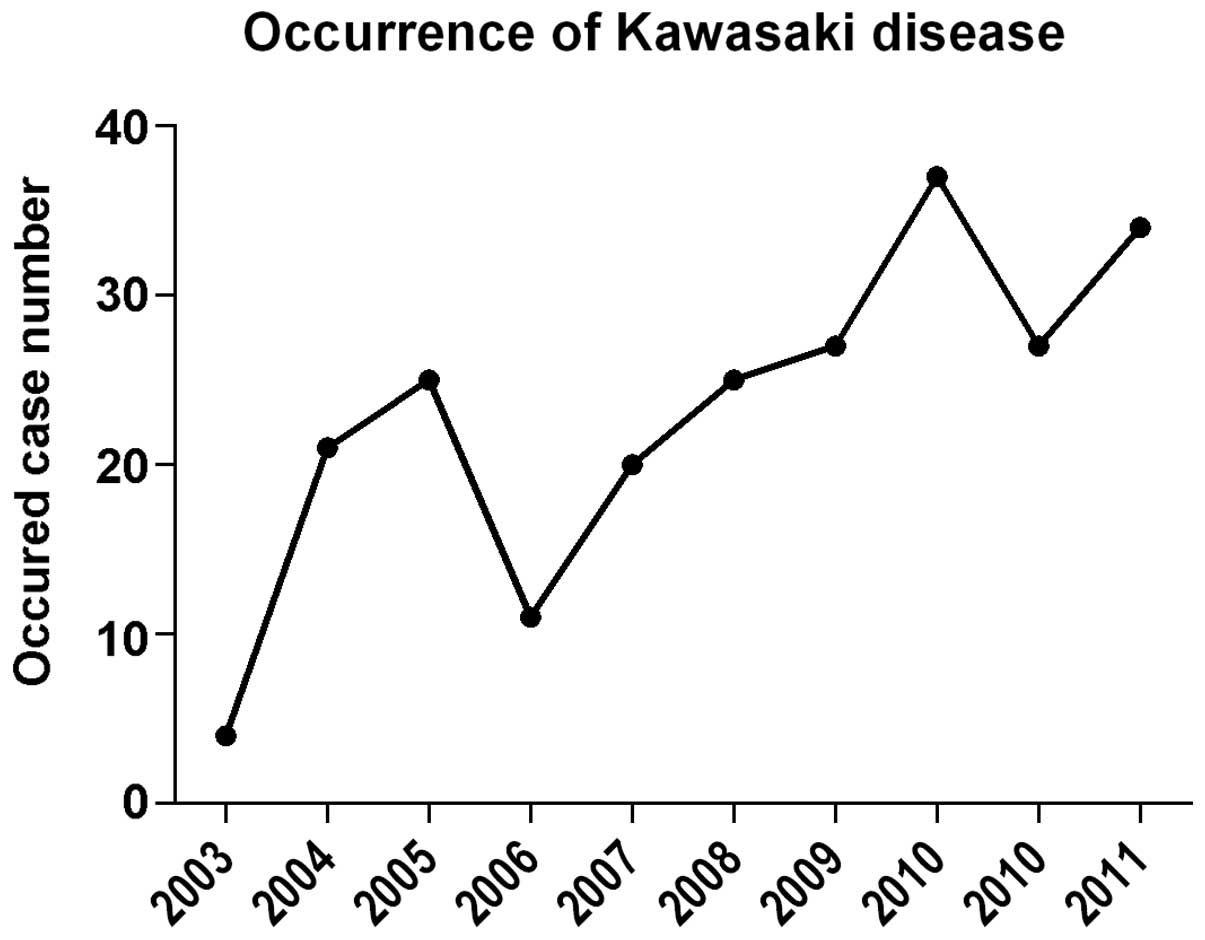
A total of 37.23% (86/231) of the cases of KD were
identified in the first five years; however, this rate was
significantly increased to 62.77% (145/231) in the last five years.
The patients were aged between 3 months and 10 years, and the age
of peak incidence was shown to be <1 year, which accounted for
23.5% of the cases. Notably, children <5 years old accounted for
92.5% of the total cases. The distribution of ages is shown in
Fig. 1.
With regard to the gender distribution, there were
157 cases in male patients and 74 cases in female patients. The
male-to-female ratio was 2.12:1, and a high risk of disease was
persistently found for male patients across the 10 years.
A total of 20 patients were identified as being from
an ethnic minority; among these patients, 18 were Mongolian (7.8%)
and 2 belonged to the Manchu ethnic minority (0.9%). No higher risk
of incidence was found for the Mongolian patients than for patients
of other ethnicities. In addition, it was found that there was no
obvious tendency of familial inheritance and seasonal preference in
the incidence of KD.
Diagnosis
For the initial visit of the patients with KD, the
hospital stay varied between 1 and 30 days, with an average time of
8 days and peak time of 4–7 days, which accounted for 48.3% of the
cases. Among the 231 cases, 179 children (77.5%) were hospitalized
10 days after the onset of symptoms. The majority of cases were
confirmed as KD 7 days after the initial hospitalization, while a
few cases were confirmed after 14 days. A total of 3 cases relapsed
at their secondary treatment, and the recurrence rate was 1.3%. All
relapses were the first to be experienced by the patients, and the
recurrence interval varied between 2 and 5 months. Among the 3
patients, 2 were male and 1 was female, and the age of recurrence
was <2 years.
Clinical characteristics
Fever was the most common clinical characteristic
and was observed in 87.6% of cases, lasting between 1 and 32 days
(average, 8.47 days). Among the other 5 observed characteristics,
the most frequently noted were lip changes and swollen neck glands
(65.9%), and the rarest was perianal peeling (11.4%). Two cases
exhibited swelling at the site of the Bacillus Calmette-Guérin
(BCG) vaccination (Table I). The
differences among the occurrence of different symptoms was
statistically significant, while the differences among the
distribution of the symptoms across the study period were not
statistically significant. Statistical analysis also showed that
the incidence of atypical KD increased from 10.38% in 2003 to
40.12% in 2012.
 | Table I.Clinical data for children with
Kawasaki disease in different years. |
Table I.
Clinical data for children with
Kawasaki disease in different years.
| Clinical
manifestations | 2003 (n=10) | 2004 (n=21) | 2005 (n=24) | 2006 (n=10) | 2007 (n=19) | 2008 (n=23) | 2009 (n=26) | 2010 (n=37) | 2011 (n=26) | 2012 (n=35) | χ2 | P-value |
|---|
| Fever lasting >5
days | 9 | 19 | 23 | 10 | 16 | 21 | 26 | 33 | 23 | 30 | 4.98 | 0.026 |
| Distal extremity
changes | 9 | 10 | 10 | 7 | 10 | 9 | 16 | 26 | 23 | 21 | 5.49 | 0.780 |
| Skin rash | 3 | 12 | 9 | 7 | 10 | 9 | 17 | 26 | 19 | 21 | 3.40 | 0.046 |
| Conjunctival
hyperemia | 9 | 14 | 14 | 9 | 12 | 10 | 14 | 28 | 19 | 24 | 4.60 | 0.032 |
| Lip changes | 5 | 16 | 14 | 9 | 14 | 14 | 16 | 24 | 21 | 24 | 5.19 | 0.820 |
| Cervical
lymphadenopathy | 7 | 14 | 17 | 7 | 9 | 17 | 17 | 24 | 19 | 23 | 3.43 | 0.064 |
Among the 231 cases of KD, 59 patients (25.54%)
exhibited other complications. There were 34 cases (14.72%) of
lower respiratory tract infection with abnormal chest X-ray
findings; most showed increased lung markings and one had severe
pneumonia. In addition, there were 3 cases of peripheral
hydrocephalus, 3 cases of urinary tract infection and 3 cases of
infantile diarrhea with dehydration. A further 2 cases exhibited
the complications of leukemia and aplastic anemia.
Laboratory examination results
The laboratory examination results of 231 cases are
shown in Table II. For the white
blood cell (WBC) count and the levels of C-reactive protein (CRP),
no statistically significant differences were found between the
number of normal and abnormal results. In the 226 cases with
available hemoglobin (Hb) data, the incidence of anemia was found
to be higher in children aged <2 years; among these cases, 14
exhibited severe anemia (6.19%). In the 226 cases with available
platelet (PLT) data, 41 patients exhibited enhanced PLT counts in
the course of 1–4 days (17.75%) and 88 cases exhibited enhanced PLT
counts in the course of 5–10 days (38.10%); in total, abnormal PLT
counts were found in 208 cases (90.04%) over an extended period
(>10 days). As the disease attenuated, the PLT counts returned
to normal levels. No statistically significant differences were
found in the incidence of coronary artery injury between patients
with enhanced and normal PLT levels (t=-1.001, P=0.321) or between
patients with enhanced and normal creatinine kinase-MB (CK-MB)
levels (t=-1.346, P=0.183).
 | Table II.Laboratory examination results. |
Table II.
Laboratory examination results.
| Laboratory
examination | Mean ± SD | Available
cases/abnormal cases (n/n) | Abnormality rate
(%) |
|---|
| CRP, mg/l |
64.38±47.07 | 216/133 | 61.57 |
| ESR, mm/h |
55.8±30.51 | 217/172 | 79.26 |
| WBC count,
109/l |
13.20±6.07 | 226/138 | 61.06 |
| Hb, g/l |
111.27±13.73 | 226/89 | 39.38 |
| PLT count,
109/l |
378.52±158.24 | 226/208 | 92.04 |
| CK-MB, U/l |
19.44±9.92 | 182/93 | 51.10 |
Echocardiography
Echocardiography was performed in all 231 cases. A
total of 146 patients (63.20%) were found to have coronary artery
disease; 144 of these cases were identified as coronary artery
expansion and 2 were identified as coronary artery aneurysms. The
results of the echocardiography are shown in Table III. Among the children with
coronary artery disease, 67.12% (98/146) were treated in the
primary hospital (such as the village, town or community hospital)
for the first time.
 | Table III.Echocardiography results. |
Table III.
Echocardiography results.
| Disease | Number of
cases | Rate (%) |
|---|
| Left coronary
artery | 38 | 16.45 |
| Right coronary
artery | 12 | 5.19 |
| Bilateral coronary
dilatation | 78 | 33.77 |
| Tricuspid
regurgitation | 56 | 24.24 |
| Mitral
regurgitation | 16 | 6.93 |
| Pericardial
effusion | 21 | 9.09 |
| Myocarditis | 16 | 6.93 |
| Coronary artery
aneurysms | 2 | 0.87 |
Discussion
Since 1993, a large number of studies (16–19) have
been performed in different areas of China to investigate the
epidemiology and clinic characteristics of KD, with a focus on the
differences among the different regions. The present study was a
retrospective study of patients with KD hospitalized in the
People's Hospital of Inner Mongolia over a 10-year period. Compared
with a previous report (17) on the
incidence and symptoms of the condition, an overall steady increase
in the incidence of KD was observed.
The results of the present study showed that
approximately two-thirds of the cases of KD occurred in the latter
5 years of the 10-year period. The age distribution of the children
with KD ranged between 3 months and 10 years, with a peak incidence
in children aged <1 year. This finding was consistent with the
results of previous epidemiological investigations in Shanghai
(17,18) and Japan (20), while the age was a little younger
than results from other regions, including Beijing and Jilin (1–2
years old) (21,22). The gender ratio of KD was shown to be
2.12:1, which was lower than the ratios found in Zhejiang (2.3:1)
(19) and Guangdong (2.23:1)
(23) and higher than those in other
regions of China, including Taiwan (1.62:1), and Japan (1.32:1)
(20–22). The recurrence rate of KD was 1.3%,
which was consistent with that in reports from Beijing (1.4%) and
Shanghai (1.2%) in the same period and lower than that reported for
Japan (2.2%) (20). The present
study showed that the incidence of KD in Mongolian children was not
significantly higher than that in other ethnic groups, and no
significant family tendency was observed for this disease. With
regard to the clinical manifestations of KD, the present results
were similar to but slightly different from those of previous
reports (17–19). In 2 cases, redness was found at the
site of the BCG vaccination, which may serve as a reference for the
early diagnosis of KD.
Consistent with improvements in the diagnosis and
treatment of the condition, the incidence of atypical KD in the
present study showed an increasing trend, which is consistent with
reports from other regions of China (16–19,23).
In recent years, laboratory examinations for
children with KD have shown considerable improvements. Parameters
such as WBC, PLT, Hb, CRP and erythrocyte sedimentation rate (ESR)
have been routinely used in the diagnosis of KD and have become
essential indicators for observing the dynamic changes in the
disease, despite their non-specificity, due to the wide-spread
abnormalities in these parameters in the majority of patients with
KD (24–26). Increases in CRP and ESR in the acute
phase have been identified as diagnostic indicators for both
typical and atypical KD (27).
Currently, the reference values for the diagnosis of incomplete KD
are as follows: CRP ≥30 mg/l or ESR >40 mm/h (28); these values should be combined with
clinical observations. In the present study, 61.06% of patients
were observed to have an increased WBC count in the acute phase,
with the remaining patients exhibiting a delayed increase following
the acute phase, which suggests a lack of support for the
association between the incidence of KD and infection.
No significant association was observed between an
increased PLT count and the occurrence of coronary artery injury
among the 231 cases; this result varied from that of another
report, in which it was concluded that an increase in PLT levels
was a risk factor for coronary artery injury among KD cases
(29). This difference may have been
associated with the small sample size in the present study. In
addition, the present study showed a lack of association between
increased CK-MB and coronary artery injury, which contradicted a
previous report in which the levels of CRP and CK-MB were
significantly correlated in cases of KD and were suggested to be
important predictors of coronary artery and myocardial damage
(30). Further verification is
therefore required for any definite conclusion.
In the present study, 63.20% of the total 231
patients with KD were found to have coronary artery disease, which
is similar to the result from Jilin (63.26%) during the same
period, while generally higher than the results from the rest of
the country and significantly higher than those from Japan
(31) and South Korea (32). Notably, fever was the most common
clinical observation in the primary diagnosis of patients with KD
and with a risk of coronary artery disease; this was attributed to
the scattered residence of patients living in Inner Mongolia, as
well as the limited medical care available to these patients,
leading to a delay in treatment and the aggravation of disease. The
2 patients with coronary aneurysms in this study were both from
remote areas; this has not been reported in previous studies. By
reviewing the dynamic changes in KD over a 10-year period, an
arc-shaped change can be observed for the general trend of coronary
artery injury in KD. In the first 3 years the occurrence of KD
showed a steady increase (Fig. 2),
which could be attributed to the lack of knowledge about atypical
KD and the referral of numerous patients to more advanced hospitals
in the adjacent provinces; in the middle 4 years, with the
improvement of clinical conditions, the rates of KD detection
increased; in the latter 3 years, the early diagnosis and treatment
of KD effectively prevented the occurrence of coronary artery
injury, particularly in the final two years when the majority of
the cases of coronary artery disease were found to be mild
expansions, with few cases of severe coronary artery aneurysms and
expansion. At present, there are few reports concerning the
dynamics changes in coronary artery injury in KD in the country
(33,34).
In conclusion, KD has become a major cause of
acquired heart disease in children (2,35).
Considering the threat of coronary artery injury to the health of
the patient, it is suggested that clinical staff, as well as
researchers, should pay more attention to the early diagnosis and
standard treatment of KD, as well as long-term follow-up visits.
Furthermore, it is necessary to enhance the clinical knowledge of
KD in primary hospitals, such as village hospitals.
References
|
1
|
Ogata S, Tremoulet AH, Sato Y, et al:
Coronary artery outcomes among children with Kawasaki disease in
the United States and Japan. Int J Cardiol. 168:3825–3828. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ayusawa M, Sonobe T, Uemura S, et al:
Kawasaki Disease Research Committee; Revision of diagnostic
guidelines for Kawasaki disease (the 5th revised edition). Pediatr
Int. 47:232–234. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Newburger JW, Takahashi M, Gerber MA, et
al: Committee on Rheumatic Fever, Endocarditis, and Kawasaki
Disease; Council on Cardiovascular Disease in the Young; American
Heart Association: Diagnosis, treatment, and long-term management
of Kawasaki disease: A statement for health professionals from the
Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease,
Council on Cardiovascular Disease in the Young, American Heart
Association. Pediatrics. 114:1708–1733. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Bayers S, Shulman ST and Paller AS:
Kawasaki disease: Part I. Diagnosis, clinical features, and
pathogenesis. J Am Acad Dermatol. 69:5012013.PubMed/NCBI
|
|
5
|
JCS Joint Working Group, . Guidelines for
diagnosis and management of cardiovascular sequelae in Kawasaki
disease (JCS 2008) - digest version. Circ J. 74:1989–2020. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Eleftheriou D, Levin M, Shingadia D,
Tulloh R, Klein NJ and Brogan PA: Management of Kawasaki disease.
Arch Dis Child. 99:74–83. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Emi M, Keicho N, Tokunaga K, et al:
Association of diffuse panbronchiolitis with microsatellite
polymorphism of the human interleukin 8 (IL-8) gene. J Hum Genet.
44:169–172. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kaneko K, Obinata K, Katsumata K, Tawa T,
Hosaka A and Yamashiro Y: Kawasaki disease in a father and
daughter. Acta Paediatr. 88:791–792. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Chang RK: Epidemiologic characteristics of
children hospitalized for Kawasaki disease in California. Pediatr
Infect Dis J. 21:1150–1155. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Golshevsky D, Cheung M and Burgner D:
Kawasaki disease - the importance of prompt recognition and early
referral. Aust Fam Physician. 42:473–476. 2013.PubMed/NCBI
|
|
11
|
Daniels LB, Gordon JB and Burns JC:
Kawasaki disease: Late cardiovascular sequelae. Curr Opin Cardiol.
27:572–577. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Neudorf U: Kawasaki disease in children
and adolescents. Z Rheumatol. 70:838–843. 2011.(In German).
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kang HJ, Kim GN and Kil HR: Changes of
clinical characteristics and outcomes in patients with Kawasaki
disease over the past 7 years in a single center study. Korean J
Pediatr. 56:389–395. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Katsumata N, Aoki J, Tashiro M,
Taketomi-Takahashi A and Tsushima Y: Characteristics of cervical
computed tomography findings in Kawasaki disease: A single-center
experience. J Comput Assist Tomogr. 37:681–685. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
JCS Joint Working Group, . Guidelines for
diagnosis and management of cardiovascular sequelae in Kawasaki
disease (JCS 2013). Digest version. Circ J. 78:2521–2562. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Jiao F, Yang L, Qiao J, Li Y, Zhang T and
Liu C: Epidemiological and clinical characteristics of Kawasaki
disease in Shanxi province. Zhonghua Liu Xing Bing Xue Za Zhi.
21:97–99. 2000.(In Chinese). PubMed/NCBI
|
|
17
|
Jiao F, Yang L, Li Y, et al: Epidemiologic
and clinical characteristics of Kawasaki disease in Shaanxi
Province, China, 1993–1997. J Trop Pediatr. 47:54–56. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Wang D, Hu B, Wang F, Zhang T and Liu C:
Study on the epidemiological features of Kawasaki disease in
Jiangsu. Zhonghua Liu Xing Bing Xue Za Zhi. 21:94–96. 2000.(In
Chinese). PubMed/NCBI
|
|
19
|
Zou LX and Gong FQ: Clinical features of
recurrent Kawasaki disease in 20 children. Zhongguo Dang Dai Er Ke
Za Zhi. 10:617–619. 2008.(In Chinese). PubMed/NCBI
|
|
20
|
Nakamura Y, Yashiro M, Uehara R, et al:
Epidemiologic features of Kawasaki disease in Japan: Results of the
2009–2010 nationwide survey. Tainjin Yi Yao. 22:216–221. 2012.
|
|
21
|
Kayiran SM, Dindar A and Gurakan B: An
evaluation of children with Kawasaki disease in Istanbul: A
retrospective follow-up study. Shiyong Yi Xue Za Zhi (Sao Paulo).
65:1261–1265. 2010.
|
|
22
|
Zhang X, Zhang Z, Liu S and Sun J:
Epidemiologic survey of Kawasaki disease in Jilin from 1999 through
2008. Pediatr Cardiol. 33:272–279. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Li XH, Li XJ, Li H, Xu M and Zhou M:
Epidemiological survey of Kawasaki disease in Sichuan province of
China. J Trop Pediatr. 54:133–136. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Satou GM, Giamelli J and Gewitz MH:
Kawasaki disease: diagnosis, management, and long-term
implications. Cardiol Rev. 15:163–169. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Yi DY, Kim JY, Choi EY, Choi JY and Yang
HR: Hepatobiliary risk factors for clinical outcome of Kawasaki
disease in children. BMC Pediatr. 14:512014. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Schnautz LS and Leggett P: Kawasaki
disease: A ride for little girls too! Crit Care Nurs Clin North Am.
20:265–271. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Liu R, He B, Gao F, Liu Q and Yi Q:
Relationship between adipokines and coronary artery aneurysm in
children with Kawasaki disease. Transl Res. 160:131–136. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Billoo AG, Lone SW, Siddiqui S and Atiq H:
Incomplete Kawaski disease: Are we missing it? J Pak Med Assoc.
59:42–43. 2009.PubMed/NCBI
|
|
29
|
Fu J, Zhang HY and Yang YZ: High risk
factors of coronary artery lesions caused by Kawasaki Disease.
Tianjin Med J. 40:679–681. 2012.(In Chinese).
|
|
30
|
Chen QJ, Lei XM, Zuo YX and Jiang L:
Relationship between serum C-reaction protein and myocardiac
enzymology, coronary artery lesions in children with Kawasaki
Disease. J Pract Med. 22:4116–4117. 2010.(In Chinese).
|
|
31
|
Ogawa S: Biochemical and immunological
laboratory findings in Kawasaki disease. Nihon Rinsho. 66:315–320.
2008.(In Japanese). PubMed/NCBI
|
|
32
|
Park YW, Han JW, Hong YM, et al:
Epidemiological features of Kawasaki disease in Korea, 2006–2008.
Pediatr Int. 53:36–39. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Xing Y, Wang H, Yu X, Chen R and Hou Y:
Assessment of coronary artery lesions in children with Kawasaki
disease: Evaluation of MSCT in comparison with 2-D
echocardiography. Pediatr Radiol. 39:1209–1215. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Xu MG, Men LN, Zhao CY, et al: The number
and function of circulating endothelial progenitor cells in
patients with Kawasaki disease. Eur J Pediatr. 169:289–296. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Dimitriades VR, Brown AG and Gedalia A:
Kawasaki disease: Pathophysiology, clinical manifestations, and
management. Curr Rheumatol Rep. 16:4232014. View Article : Google Scholar : PubMed/NCBI
|