Introduction
Idiopathic basal ganglia calcification (IBGC), also
known as Fahr's syndrome, is a rare neurodegenerative disorder
characterized by neuropsychiatric abnormalities, parkinsonian or
choreoathetotic-type movement disturbances and extensive
symmetrical calcification of the basal ganglia and dentate nuclei
in the cerebellum (1). IBGC is a
rare calcium metabolism disorder with high genotypic and phenotypic
heterogeneity, with symptoms that cannot be explained by any
particular disorder of calcium phosphorus metabolism, or other
disease (2). There are no guidelines
for the treatment of ICBG, and there are currently no reversible
measures available to reduce the calcification. In the clinical
environment, doctors often provide treatment for the symptoms,
including pharmacologic treatment for the improvement of anxiety,
depression and obsessive-compulsive behaviors. Sobrido et al
(3) previously suggested that
at-risk asymptomatic adult family members may seek genetic
counseling, in order to make personal decisions regarding
reproduction, financial matters, and career planning. Few reports
have described psychiatric symptoms as early manifestations of
IBGC. The present study reports a case of IBGC in a middle-aged
male who first manifested schizophrenia-like psychosis and
obsessive-compulsive symptoms without evident movement disorders.
The response of the patient to treatment with olanzapine and
fluoxetine is also presented. To the best of our knowledge, this is
the first report of parkinsonism during treatment with olanzapine
and the response to fluoxetine in IBGC. The patient provided
written informed consent.
Case report
A 41-year-old, right-handed male of Han ethnicity,
was admitted to the inpatient psychiatric service of the Second
Affiliated Hospital of Zhejiang University School of Medicine
(Hangzhou, China) with schizophrenia-like psychosis and
obsessive-compulsive symptoms. For 1 month prior to admission, the
patient had complained about auditory hallucinations which
commented on him and commanded him to commit suicide; he also felt
himself to be controlled by ‘the devil’. The patient suspected that
people were always discussing him and wanted to kill him. In
addition, he had intrusive thoughts with repetitive behaviors.
Defecation was a source of worry to the patient and he repetitively
touched his anus, which he recognized to be irrational. In
addition, the patient repeatedly checked whether doors were locked
or lights were turned off, refused to go outside and stopped going
to work.
According to the patient's father, the patient had
displayed normal development. Since graduating from high school
with poor grades, he had been working as a janitor. Family history
was remarkable in that the patient's mother and grandmother had
been diagnosed with parkinsonism. In addition, his mother's elder
brother had dementia at 50 years of age and a younger brother had
schizophrenia-like psychosis requiring treatment in a psychiatric
hospital.
Neurological examination was essentially normal with
the exception of a slight bilateral tremor in the hands and a
slightly expressionless face. On mental status examination, the
patient was oriented and cooperative but nervous. He had auditory
hallucinations, delusions of reference and persecution, obsessive
ideas, repetitive behaviors and difficulty in concentration and
long-term recall. The patient was anxious and mildly depressed, but
denied homicidal ideation or suicidal behavior. Psychological
testing revealed a positive and negative syndrome scale (PANSS)
score of 82, a Yale-Brown obsessive-compulsive scale symptom
checklist (YBOCS) score of 25, and a Wechsler Adult Intelligence
Scale-Chinese Revision IQ score of 55, including a verbal IQ of 54
and a performance IQ of 63.
Blood tests including hemocytology, liver and kidney
function, glucose, calcium, phosphorus, parathyroid hormone,
ceruloplasmin, antinuclear antibodies, thyroid hormone, vitamin
B12, folate and ammonia were all within the normal
range. The results of the electrocardiogram, chest computerized
tomography (CT), electroencephalogram, abdominal and thyroid
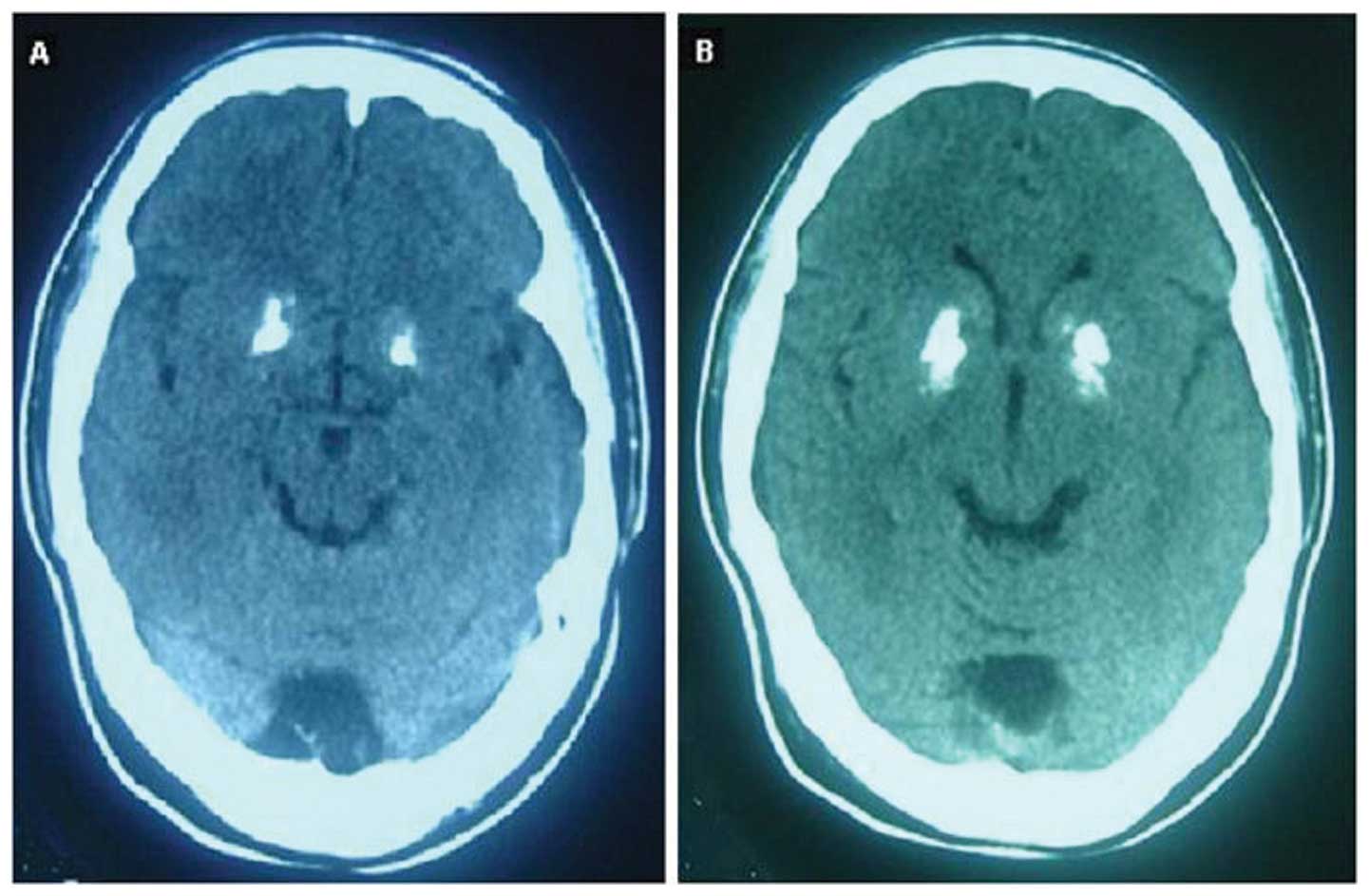
ultrasonography were all normal. The brain CT scan revealed
symmetrical calcification in the basal ganglia (Fig. 1).
The patient was therefore diagnosed with IBGC and
was prescribed 20 mg fluoxetine and 5 mg olanzapine daily. The
olanzapine dose was increased to 10 mg after 2 days. Two weeks
later, the patient's obsessions were unchanged but the psychotic
symptoms were absent; however, the patient showed a parkinsonian
gait, hypomimia, muscle rigidity and evident tremors with a
positive finger-to-nose test. His Unified Parkinson's Disease
Rating Scale (UPDRS) motor score was 25, while his PANSS score was
42 and his YBOCS score was 24. The fluoxetine dose was then
increased to 40 mg and the olanzapine dose was decreased to 5 mg.
Two weeks later, parkinsonism and obsessions improved with a UPDRS
score of 13 and a YBOCS score of 15. Treatment with the two drugs
was continued for 3 months. The patient then had no psychosis but
continued to have mild obsessions with a YBOCS score of 6 and
parkinsonian symptoms. After the olanzapine dose was decreased to
2.5 mg, the parkinsonism improved to a UPDRS score of 5. The
neuropsychiatric condition of the patient remained stable during 3
months of follow up.
In summary, the patient with IBGC exhibited
schizophrenia-like psychosis and obsessive-compulsive symptoms as
the first manifestations that required hospitalization, and also
showed mild dementia and parkinsonism. Brain CT confirmed IBGC.
Metabolic diseases including hypoparathyroidism,
pseudohypoparathyroidism and hyperparathyroidism were excluded on
the basis of normal levels of serum calcium and phosphorus. No
other significant symptoms or history suggested calcifications
following a systemic disorder such as mitochondrial encephalopathy,
tuberous sclerosis, Sturge-Weber syndrome and idiopathic
hemochromatosis (4).
Discussion
The major clinical features of IBGC are movement
disorders, which may be associated with cognitive deficits and
psychiatric disturbances. There have been few reports of
obsessive-compulsive symptoms in IBGC or psychiatric symptoms as
the initial manifestation of IBGC. The patient in the current study
initially presented with a schizophrenia-like psychosis and
obsessive-compulsive symptoms. The brain abnormalities found in
schizophrenia and obsessive-compulsive disorder (OCD) reveal the
involvement of similar brain regions, including the frontal lobe,
basal ganglia and thalamus (5). We
considered both psychiatric symptoms to be shown simultaneously and
linked to the basal ganglia pathology in this patient.
There are no guidelines for the treatment of IBGC,
and drug therapy aims only to alleviate the symptoms. Few data on
appropriate psychotropic treatment have ever been reported, and the
use of neuroleptics is complicated by the risk of worsening the
underlying movement disorders. Rosenblatt and Leroi suggested that
high-potency neuroleptics or atypical antipsychotics could be used
in IBGC (6). Shoyama et al
reported that an IBGC patient with schizophrenia-like psychosis
became well when treated with low-dose risperidone without
worsening parkinsonism (1). Mishra
et al used olanzapine 30 mg to treat an patient with IBGC
and Capgras syndrome (7). The
patient in the current study clearly had parkinsonism after being
treated with an olanzapine dose of 10 mg but improved when the dose
was decreased to 2.5 mg, suggesting that the tolerance to
antipsychotics of patients with IBGC may vary. The management of
OCD in basal ganglia disorders follows the treatment for idiopathic
OCD. Fluoxetine was the first selective serotonin reuptake
inhibitor antidepressant and the effective dose range is 40–60 mg
in OCD therapy (8). The current case
was treated with fluoxetine 40 mg, which showed definite efficacy
and was well tolerated.
The present case demonstrates that patients with
IBGC may exhibit schizophrenia-like psychosis and
obsessive-compulsive symptoms as the first manifestations of the
condition. IBGC should be considered as part of the differential
diagnosis in the evaluation of initial psychiatric symptoms, and
brain CT is a useful adjuvant examination. Low-dose olanzapine is
effective and should be increased cautiously to avoid worsening
parkinsonism. Fluoxetine is an effective drug to treat
obsessive-compulsive symptoms in IBGC.
Acknowledgements
This study was partly supported by grants from
Zhejiang Science and Technology Research Fund in China (No.
2012C33119) and Zhejiang Medical Science Research Fund in China
(No. 2012KYB095) provided to Weibo Liu.
References
|
1
|
Shoyama M, Kitabata Y, Kaku T and
Shinosaki K: Evaluation of regional cerebral blood flow in Fahr
disease with schizophrenia-like psychosis: A case report. AJNR Am J
Neuroradiol. 26:2527–2529. 2005.PubMed/NCBI
|
|
2
|
Oliveira JR, Spiteri E, Sobrido MJ, Hopfer
S, Klepper J, Voit T, Gilbert J, Wszolek ZK, Calne DB and Stoessl
AJ: Genetic heterogeneity in familial idiopathic basal ganglia
calcification (Fahr disease). Neurology. 63:2165–2167. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Sobrido MJ, Hopfer S and Geschwind DH:
Familial idiopathic basal ganglia calcificationGeneReviews
(Internet). Pagon RA, Bird TD, Dolan CR and Stephens K: University
of Washington; Seattle: 1993–2004 updated. September 20–2007
|
|
4
|
Vakaet A, Rubens R, de Reuck J and vander
Eecken H: Intracranial bilateral symmetrical calcification on
CT-scanning: A case report and a review of the literature. Clin
Neurol Neurosurg. 87:103–111. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Venkatasubramanian G, Rao NP and Behere
RV: Neuroanatomical, neurochemical and neurodevelopmental basis of
obsessive-compulsive symptoms in schizophrenia. Indian J Psychol
Med. 31:3–10. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Rosenblatt A and Leroi I: Neuropsychiatry
of Huntington's disease and other basal ganglia disorders.
Psychosomatics. 41:24–30. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Mishra BR, Prakash R, Mishra BN, Praharaj
SK and Sinha VK: Capgras syndrome associated with Fahr's disease. J
Neuropsychiatry Clin Neurosci. 21:354–355. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Etain B and Bonnet-Perrin E: Value of
fluoxetine in obsessive-compulsive disorder in the adult: Review of
the literature. Encephale. 27:280–289. 2001.(In French). PubMed/NCBI
|