Introduction
Local anesthetics (LAs) are drugs that reversibly
block the transmission of nerve impulses, without affecting
consciousness; however, accidental intravascular injection, drug
overdose or rapid absorption from the administration site can
induce severe LA systemic toxicity (LAST). LAST is a rare but
potentially fatal complication of regional anesthesia, which may
result in cardiovascular (CVS) and central nervous system (CNS)
toxicity (1). Previously, the
treatment of LAST was a challenge, as no specific therapy was
available (2); however, it was later
observed that a lipid emulsion was able to effectively resuscitate
rats that had received an overdose of bupivacaine (3). Since then, a number of studies have
reported the successful use of lipid emulsion therapy for the
treatment of LAST (4,5). To date, intravenous lipid emulsions
have been used to treat systemic toxicity induced by a variety of
LAs, including bupivacaine, levobupivacaine, ropivacaine and
mepivacaine (6–8).
The resuscitative capacity of lipid emulsion for
LA-induced CVS toxicity has been extensively studied (9); however, the efficacy of intravenous
lipid emulsions in reducing LA-induced CNS toxicity has not been
fully characterized. Oda and Ikeda (6) reported that a lipid emulsion
effectively decreased the CNS and CVS toxicity induced by
bupivacaine and levobupivacaine in conscious rats. Furthermore,
previous clinical studies have indicated that lipid emulsion may be
effective for treating LA-induced CNS toxicity (10,11). The
‘lipid-sink’ theory suggests that lipophilic LAs are chelated by
lipid emulsions in the blood, which lowers the concentration of the
freebase form of the LA, thus reducing the availability of the LAs
to tissues and resulting in decreased toxicity (12). The majority of previous experiments
examining the effects of lipid emulsions on LAST involved the
intravenous injection of LAs, followed by the intravenous
administration of a lipid emulsion; therefore, it is difficult to
determine whether lipid emulsions can have a direct effect on the
CNS to limit toxicity.
The aim of the present study was to evaluate the
effect of intravenously administered lipid emulsions on the CNS
toxicity induced by lidocaine, levobupivacaine and ropivacaine,
which were directly perfused into the lateral ventricles of Sprague
Dawley (SD) rats. In addition, this study aimed to compare the
toxicity of these three types of LAs in a rat model of CNS
toxicity.
Materials and methods
Experimental animals
In total, 100 healthy male SD rats, aged 10 weeks
and weighing 240–300 g, were purchased from the Laboratory Animal
Center of Luzhou Medical College (Luzhou, China) and maintained in
a temperature-controlled room with a 12-h light/dark cycle and
regular access to food and water. Experimental procedures were
approved by the Laboratory Animal Care Committee at Luzhou Medical
College. All animals received care according to the Guide for the
Care and Use of Laboratory Animals (National Institutes of Health,
Bethesda, MD, USA).
Animal model and experimental
procedure
Rats were allocated at random into four main groups:
Sham (A; n=10), lidocaine (B, n=30), levobupivacaine (C; n=30) and
ropivacaine (D; n=30). Groups B–D were subsequently subdivided into
three subgroups: Toxic, post-conditioning and pre-conditioning
(n=10 per subgroup). The rats were weighed and subsequently
anesthetized with an intraperitoneal injection of 2% sodium
pentobarbital (40 mg·kg−1). Heat pads (Softron, Beijing,
China) were used for the maintenance of body temperature at 37°C.
Spontaneous breathing was maintained, and then a tail vein
puncture, tracheal intubation and femoral artery puncture were
conducted, with continuous injection of Ringer's solution (Minsheng
Pharmaceutical Group Co. Ltd., Hangzhou, China) by a computerized
infusion pump (Wego, Weihai, China) at a rate of 1
ml·kg−1·min−1. Simultaneously,
electrocardiogram, heart rate and mean arterial pressure
measurements of the rats were continuously recorded using a BL-420E
biological function experimental recorder (Chengdu Thai Union
Technology Co., Ltd., Chengdu, China). The onset of convulsions was
indicated by the appearance of tonic-clonic movement in the rat
legs and spike waves on an electroencephalogram, and the data were
recorded. Following cerebroventricular puncture, the LA was
injected gradually into the lateral ventricle using a microsyringe
at a rate of 50 µl·min−1. The dosages of the LAs,
determined by preliminary experiments, were as follows: 0.75%
lidocaine hydrochloride (200 µl·kg−1; Yashen
Pharmaceutical Co. Ltd., Linzhou, China), 0.75% levobupivacaine
hydrochloride (140 µl·kg−1; Hengrui Medicine Co. Ltd.,
Lianyungang, Jiangsu, China) and 1% ropivacaine hydrochloride (200
µl·kg−1; Hengrui Medicine Co. Ltd.). Rats in the
post-conditioning subgroups that exhibited respiratory arrest were
administered 20% lipid emulsion (Intralipid; 5 ml·kg−1;
Sino-Swed Pharmaceutical Corp. Ltd., Beijing, China) via a tail
vein injection, and were continually administered lipid emulsion
using a computerized infusion pump at a rate of 0.25
ml·kg−1·min−1. Similarly, rats in the
pre-conditioning subgroups received a tail vein injection of 20%
lipid emulsion (5 ml·kg−1), followed by infusion using a
computerized infusion pump at a rate of 0.25
ml·kg−1·min−1; however, this treatment was
administered for 30 min prior to the intracerebroventricular
injection of LA. Sham group rats received 0.9% normal saline (2
µl·kg−1), which was injected into the lateral ventricle
at a rate of 50 µl·min−1. The time between the injection
of LA and the onset of respiratory arrest and arrhythmia was
recorded in all groups. Neurological behavior was evaluated using a
previously described method (13,14), and
the resulting scores were recorded prior to the LA treatment and at
6, 12 and 24 h after treatment. At 24 h after treatment, the rats
were sacrificed. Firstly, the rats were anaesthetized by 2%
pentobarbital intraperitoneal injection, and then 4%
paraformaldehyde was perfused rapidly, with the aim of reducing
animal suffering as much as possible. The brains were excised,
fixed in 4% paraformaldehyde and embedded in paraffin blocks.
Subsequently, 4-µm sections were stained with hematoxylin and eosin
using standard protocols. Images were obtained using a Nikon
Eclipse E400 optical microscope and software package (Nikon Corp.,
Tokyo, Japan), and neuronal density in the hippocampal CA1 zone was
subsequently measured. Cones cell morphology of hippocampal CA1 was
observed under the microscope, with the same view captured under
magnification x100 and x400. The cell morphological differences
between groups were observed and neuronal density was measured.
Statistical analysis
Results are expressed as the mean ± standard
deviation. Statistical analysis was performed using SPSS software,
version 17.0 (SPSS, Inc., Chicago, IL, USA). Differences in the
heart rate, blood pressure, neurological behavior scores, neuronal
density and time from LA injection to respiratory arrest, apnea and
start of arrhythmia among the groups were examined using one-way
analysis of variance. P<0.05 was considered to indicate a
statistically significant difference.
Results
Lipid emulsion mitigates LA-induced
respiratory arrest
Prior to treatment, no differences in baseline
weight, blood pressure, heart rate and respiration were observed
among the groups (data not shown). The lateral ventricle was
punctured successfully in all rats, and 0.9% normal saline or the
respective LAs were injected. LAST onset was observed in all rats
following the injection of LA into the lateral ventricle. Rats in
the toxic subgroups all died from respiratory arrest. Rats in the
post-conditioning subgroups also exhibited respiratory arrest;
however, following the application of cardiopulmonary resuscitation
(via closed chest cardiac massage) and breathing support (assisted
with a ventilator), all rats were resuscitated from the CNS
toxicity-induced respiratory arrest. No respiratory arrest was
observed in the rats in the pre-conditioning subgroups.
Effect of pre- and post-conditioning
on time to respiratory arrest and apnea
Following the intracerebroventricular injection of
LA, the time to respiratory arrest was compared among the toxic
subgroups. The data showed no significant differences between the
toxic subgroups of groups B and C (P>0.05); however, these
subgroups differed significantly compared with the group D toxic
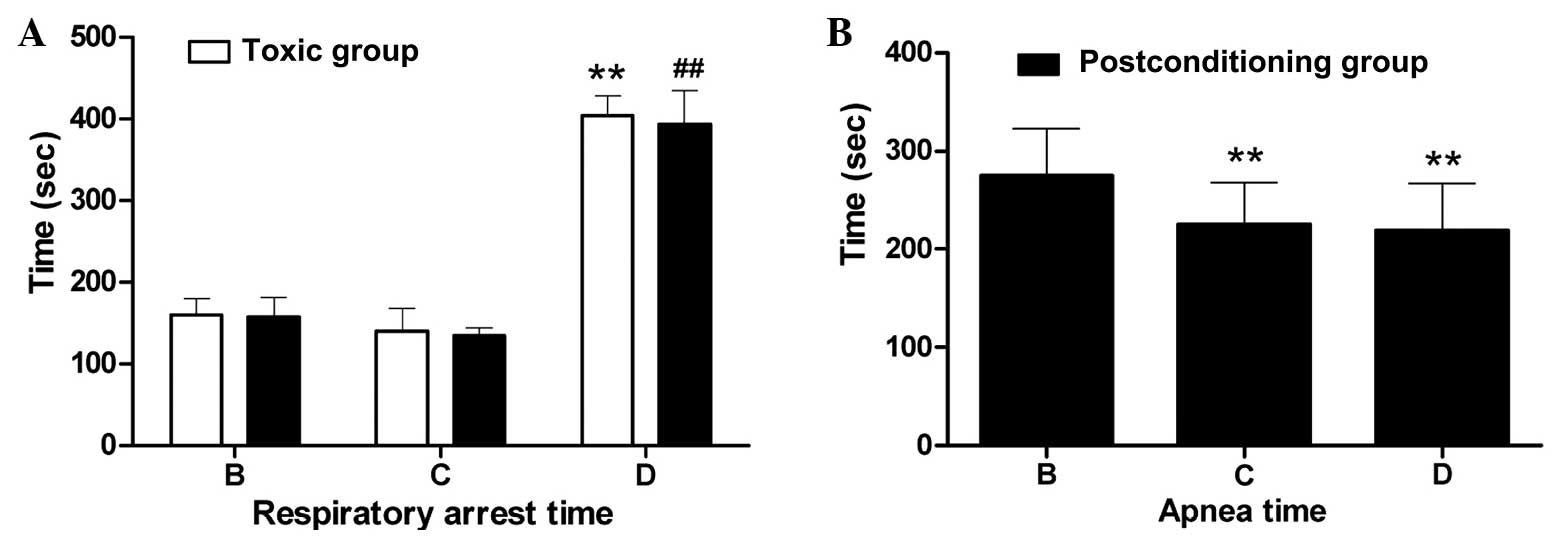
subgroup (P<0.01; Fig. 1A).
Similarly, no significant differences were detected between the
post-conditioning subgroups of groups B and C (P>0.05), while
significant differences were observed between these subgroups and
the group D post-conditioning subgroup (P<0.01; Fig. 1A). Within groups B, C and D, no
significant differences were observed in respiratory arrest time
between the respective toxic and post-conditioning subgroups
(P>0.05; Fig. 1A). No respiratory
arrest was exhibited by rats in the pre-conditioning subgroup rats
of groups B–D. With regard to apnea time, significant differences
were detected among the post-conditioning subgroups of groups B, C
and D (P<0.01; Fig. 1B). The
decreasing order of recovery time was as follows: Lidocaine (group
B) > levobupivacaine (group C) > ropivacaine (group D).
Heart rate, blood pressure and
arrhythmia
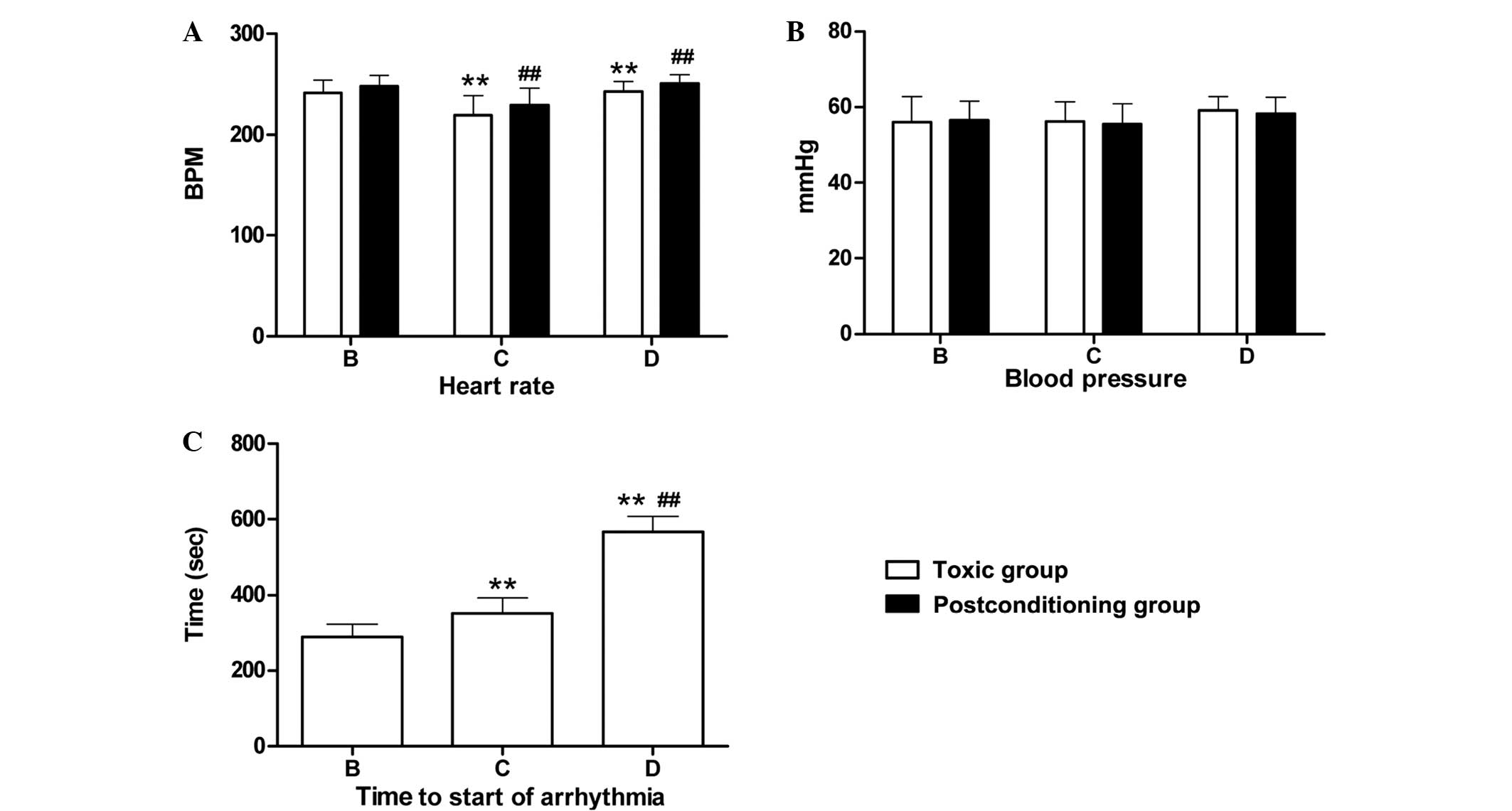
Heart rates were measured when respiratory arrest
occurred in the toxic and post-conditioning subgroups following the
intracerebroventricular injection of LA. No significant difference
in heart rate was observed between the toxic subgroups of groups C
and D (P>0.05); however, significant differences were detected
between these subgroups and the toxic subgroup of group B
(P<0.01; Fig. 2A). Similar
results were observed among the post-conditioning subgroups of
groups B, C and D. Within groups B–D, there were no significant
differences in heart rate between the respective toxic and
post-conditioning subgroups (P>0.05; Fig. 2A). Similarly, no significant
differences in blood pressure were detected when respiratory arrest
occurred among the respective toxic and post-conditioning subgroups
following the intracerebroventricular injection of the LAs
(Fig. 2B). Arrhythmia was detected
only in the toxic subgroups of groups B, C and D. The types of
arrhythmia detected included bradycardia, premature contraction and
irregular heartbeats. Significant differences in the time from LA
injection to arrhythmia onset were detected among groups B, C and D
(P<0.01). The decreasing order of onset time was as follows:
Ropivacaine (group D) > levobupivacaine (group C) > lidocaine
(group B) (Fig. 2C).
Neurobehavioral scores and neuronal
density
Prior to LA injection, neurological behavior scores
were normal in all groups. Following treatment, all the rats in the
toxic subgroups died. The neurological scores of rats in the post-
and pre-conditioning subgroups of groups B, C and D were
significantly reduced compared with the scores of the sham group
rats at the corresponding time-points following treatment
(P<0.01). The neurological behavior of groups B, C and D treated
after 6, 12 and 24 h was significantly lower than the sham group
(P<0.01). There was no statistically significant difference
between pre- and post-conditioning subgroups of groups B, C and D
at different time-points, respectively (P>0.05). Differences
were statistically significant in the sham group at 6, 12 and 24 h
time-points; toxic group, pre- and post-conditioning subgroups are
significantly different from rat models treated for 24 h
(P<0.01; Table I). Results for
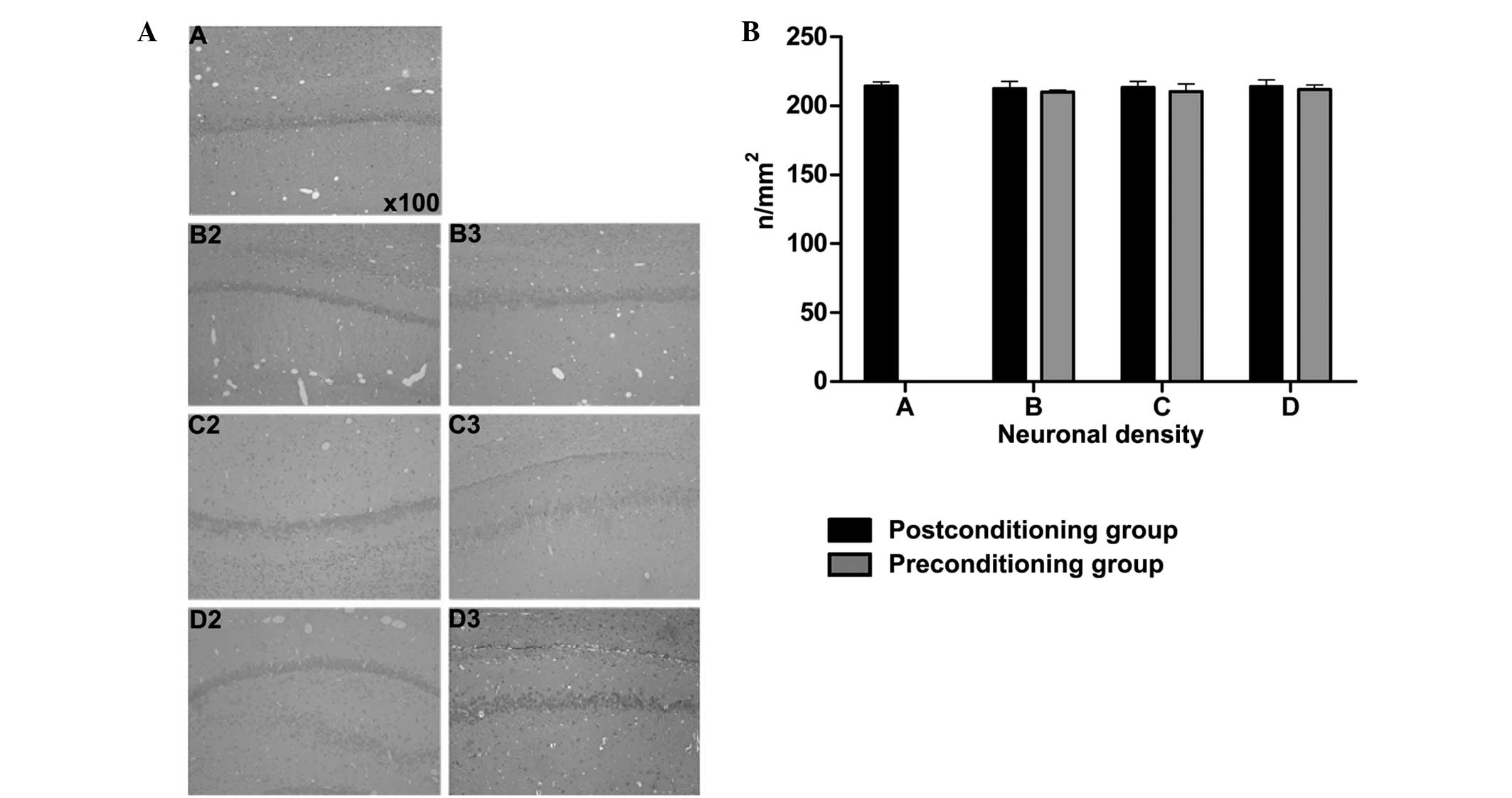
the neuronal density in the rat hippocampal CA1 zones are presented
in Fig. 3A and B. The results showed
that the neuronal hippocampal density was normal in each group at
24 h after treatment, with no significant differences observed
among the various treatment groups (P>0.05).
 | Table I.Neurological behavior scores at
various time-points (mean± standard deviation). |
Table I.
Neurological behavior scores at
various time-points (mean± standard deviation).
| Group | Baseline | 6 h | 12 h | 24 h |
|---|
| Sham (A) | 17.50±1.27 |
12.70±0.95b–g |
14.90±0.99b–g |
15.90±0.74b–g |
| Lidocaine (B) |
|
|
|
|
| 1 | 16.40±1.07 | 0 | 0 | 0 |
| 2 | 16.60±0.84 |
9.00±0.67a,c–e |
9.40±0.70a |
12.40±1.17a |
| 3 | 16.70±0.95 |
10.0±1.05a,b,d,e |
10.09±1.45a |
12.80±1.39a |
| Levobupivacaine
(C) |
|
|
|
|
| 1 | 16.10±1.20 | 0 | 0 | 0 |
| 2 | 15.30±0.95 |
8.10±0.32a–c,f,g |
9.10±0.57a |
11.70±0.95a,g |
| 3 | 15.80±0.92 |
7.90±0.88a–c,f,g |
9.20±0.63a |
11.50±0.85a,g |
| Ropivacaine (D) |
|
|
|
|
| 1 | 15.80±1.03 | 0 | 0 | 0 |
| 2 | 16.10±0.88 |
8.80±0.63a,d,e |
9.00±0.47a |
11.90±1.10a |
| 3 | 16.30±1.16 |
9.00±0.67a,d,e |
9.70±0.67a |
12.30±0.67a |
Discussion
Previous animal studies and human case reports have
provided increasing evidence in support of the use of lipid
emulsions for the treatment of patients suffering from LA-induced
toxicity (3–5,15,16).
Weinberg et al (3)
demonstrated that LA-induced cardiotoxicity could be treated
effectively using 10, 20 and 30% lipid emulsions. Animal studies
using rats and dogs determined that the use of lipid emulsion as a
pretreatment or during resuscitation offered successful recovery
from bupivacaine overdose (15,17).
Previous studies have predominantly focused on the effective
resuscitative effect of lipid emulsion on LA-induced CVS toxicity
(9); however, the capacity of
intravenous lipid emulsions to effectively reduce LA-induced CNS
toxicity has remained incompletely understood. Furthermore, based
on the lipid-sink theory, the combined intravenous injection of LAs
and lipid emulsion has made it difficult to determine whether lipid
emulsions can have a direct effect on the CNS to prevent toxicity
(12).
In the present study, an SD rat model was employed
in which LAs were directly perfused into the lateral ventricle. The
LAs were thus able to cross the blood-brain barrier and perfuse
into the ventricle, inducing CNS, but not CVS, toxicity. This model
facilitated the specific examination of the effect of lipid
emulsions on LA-induced CNS toxicity. The results showed that rats
in the toxic subgroups all died from breathing arrest following the
injection of LA into the lateral ventricle. However, in rats
treated with lipid emulsion following LA injection, respiration was
restored and all rats were resuscitated from CNS toxicity-induced
respiratory arrest. Rats pretreated with lipid emulsion prior to
the injection of LA exhibited no respiratory arrest. Further
experiments revealed no significant differences in heart rate or
blood pressure following respiratory arrest between the toxic and
post-conditioning subgroups. In addition, no significant
differences were detected in neurological behavior scores and
neuronal density in the hippocampal CA1 zone among the post- and
pre-conditioning subgroups of groups B, C and D at different points
following treatment. Collectively, these results suggest that
post-conditioning with lipid emulsion is able to mitigate the
effects of CNS toxicity, while pre-conditioning is able to prevent
LA-induced CNS toxicity. To the best of our knowledge, the present
study is the first to examine the resuscitative effects of lipid
emulsion on LA-induced CNS toxicity.
In contrast to numerous clinical reports describing
the effect of lipid emulsion on the overdose of various LAs, such
as bupivacaine, levobupivacaine, ropivacaine and lidocaine
(4,5,10,18), the
majority of animal studies have investigated bupivacaine. Few
studies have examined the effects of lipid emulsion on the toxicity
of LAs other than bupivacaine in animals (19). In the present study, the toxicity of
three types of LA, lidocaine, levobupivacaine and ropivacaine, was
examined and compared. The data showed that lipid emulsion was able
to decrease the CNS toxicity induced by all three LAs, but that the
toxicity of the three LAs differed. The relative respiratory
recovery time observed for each of the LAs was as follows, in
decreasing order: Lidocaine > levobupivacaine > ropivacaine.
Furthermore, in decreasing order, the time from the LA injection to
the onset of arrhythmia was as follows: Ropivacaine >
levobupivacaine > lidocaine. These results suggest that the
relative toxicity of the three LAs is as follows: Lidocaine >
levobupivacaine > ropivacaine. The lipophilicity of these LAs is
known to be as follows: Lidocaine > levobupivacaine >
ropivacaine (16,20–23).
Notably, the apparent toxicity of these three LAs correlates with
their lipophilicity, which is consistent with the lipid-sink
theory.
In conclusion, the present study suggests that lipid
emulsion post-conditioning is able to mitigate LA-induced CNS
toxicity, while pre-conditioning is able to prevent LA-induced CNS
toxicity in rats. Further studies are required to elucidate the
mechanism underlying the interaction between lipid emulsions and
LAs in CNS toxicity.
Acknowledgements
This study was supported by grants from the Medical
Scientific Research Foundation of Sichuan Province (China), Health
and Family Planning Commission of Sichuan Province (no. 110334),
the Affiliated Hospital of Luzhou Medical College of Sichuan
Province (no. 11208). The authors would like to thank Dr Changhe
Ren and Master Liqun Mo for help with experimental methods and Dr
Jun Zhou for the data analysis.
References
|
1
|
Wolfe JW and Butterworth JF: Local
anesthetic systemic toxicity: Update on mechanisms and treatment.
Curr Opin Anaesthesiol. 24:561–566. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Zink W and Graf BM: Toxicology of local
anesthetics. Clinical, therapeutic and pathological mechanisms.
Anaesthesist. 52:1102–1123. 2003.(In German). View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Weinberg GL, VadeBoncouer T, Ramaraju GA,
Garcia-Amaro MF and Cwik MJ: Pretreatment or resuscitation with a
lipid infusion shifts the dose-response to bupivacaine-induced
asystole in rats. Anesthesiology. 88:1071–1075. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Rosenblatt MA, Abel M, Fischer GW,
Itzkovich CJ and Eisenkraft JB: Successful use of a 20% lipid
emulsion to resuscitate a patient after a presumed
bupivacaine-related cardiac arrest. Anesthesiology. 105:217–218.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Litz RJ, Popp M, Stehr SN and Koch T:
Successful resuscitation of a patient with ropivacaine-induced
asystole after axillary plexus block using lipid infusion.
Anaesthesia. 61:800–801. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Oda Y and Ikeda Y: Effect of lipid
emulsion on the central nervous system and cardiac toxicity of
bupivacaine and levobupivacaine in awake rats. J Anesth.
27:500–504. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sakai T, Manabe W, Kamitani T, Takeyama E
and Nakano S: Ropivacaine-induced late-onset systemic toxicity
after transversus abdominis plane block under general anesthesia:
Successful reversal with 20% lipid emulsion. Masui. 59:1502–1505.
2010.(In Japanese). PubMed/NCBI
|
|
8
|
Dix SK, Rosner GF, Nayar M, et al:
Intractable cardiac arrest due to lidocaine toxicity successfully
resuscitated with lipid emulsion. Crit Care Med. 39:872–874. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Weinberg GL: Treatment of local anesthetic
systemic toxicity (LAST). Reg Anesth Pain Med. 35:188–193. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Foxall G, McCahon R, Lamb J, Hardman JG
and Bedforth NM: Levobupivacaine-induced seizures and
cardiovascular collapse treated with Intralipid. Anaesthesia.
62:516–518. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lange DB, Schwartz D, DaRoza G and Gair R:
Use of intravenous lipid emulsion to reverse central nervous system
toxicity of an iatrogenic local anesthetic overdose in a patient on
peritoneal dialysis. Ann Pharmacother. 46:e372012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Weinberg G, Lin B, Zheng S, et al:
Partitioning effect in lipid resuscitation: Further evidence for
the lipid sink. Crit Care Med. 38:2268–2269. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Dong WK, Bledsoe SW, Eng DY, et al:
Profound arterial hypotension in dogs: Brain electrical activity
and organ integrity. Anesthesiology. 58:61–71. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Dong WK, Bledsoe SW, Chadwick HS, Shaw CM
and Hornbein TF: Electrical correlates of brain injury resulting
from severe hypotension and hemodilution in monkeys.
Anesthesiology. 65:617–625. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Weinberg G, Ripper R, Feinstein DL and
Hoffman W: Lipid emulsion infusion rescues dogs from
bupivacaine-induced cardiac toxicity. Reg Anesth Pain Med.
28:198–202. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Mulroy MF: Systemic toxicity and
cardiotoxicity from local anesthetics: Incidence and preventive
measures. Reg Anesth Pain Med. 27:556–561. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Aumeier C, Kasdor B, Gruber M, et al:
Lipid emulsion pretreatment has different effects on mepivacaine
and bupivacaine cardiac toxicity in an isolated rat heart model. Br
J Anaesth. 112:735–741. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Litz RJ, Roessel T, Heller AR and Stehr
SN: Reversal of central nervous system and cardiac toxicity after
local anesthetic intoxication by lipid emulsion injection. Anesth
Analg. 106:1575–1577, table of contents. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ok SH, Sohn JT, Baik JS, et al: Lipid
emulsion reverses Levobupivacaine-induced responses in isolated rat
aortic vessels. Anesthesiology. 114:293–301. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Mather LE, Copeland SE and Ladd LA: Acute
toxicity of local anesthetics: Underlying pharmacokinetic and
pharmacodynamic concepts. Reg Anesth Pain Med. 30:553–566. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Groban L: Central nervous system and
cardiac effects from long-acting amide local anesthetic toxicity in
the intact animal model. Reg Anesth Pain Med. 28:3–11. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Chang DHT, Ladd LA, Copeland S, et al:
Direct cardiac effects of intracoronary bupivacaine/levobupivacaine
and ropivacaine in the sheep. Br J Pharmacology. 132:649–658. 2001.
View Article : Google Scholar
|
|
23
|
Casati A, Chelly JE, Cerchierini E, et al:
Clinical properties of levobupivacaine or racemic bupivacaine for
sciatic nerve block. J Clin Anesth. 14:111–114. 2002. View Article : Google Scholar : PubMed/NCBI
|