Introduction
Computed tomography (CT)-guided percutaneous core
needle biopsy (PCNB) of the lung is a widely accepted and
frequently used interventional radiological procedure that aims to
diagnose pulmonary pathological conditions. Common complications
include pneumothorax and pulmonary hemorrhage, both of which are
known to be generally self-resolving with no clinical intervention
required. Air embolism is a potentially life-threatening but
extremely rare complication, with an estimated incidence of
0.02–0.06% (1,2); however, the incidence of air embolism
is considered to be underestimated due to undiagnosed asymptomatic
patients (3–5). The present study reports a case of air
embolism in the coronary and spinal arteries, which, following a
CT-guided PCNB of the lung, resulted in sudden mortality. In
addition, a summary of the most common characteristics of
symptomatic air embolism, based on the present case and a review of
the literature, is presented in this study.
Case report
A 53-year-old woman visited the Second Affiliated
Hospital of Dalian Medical University (Dalian, China), with a
15-day history of a productive cough. No indications of previous
abnormalities were identified in the patient's history. Chest
CT-scan results showed multiple nodular and flake-shaped lesions in
both lungs. It was recommended that the patient be referred for a
CT-guided PCNB of the lung for pulmonary histopathological
diagnosis. Prior to the procedure, the patient was fully informed
about all the details of the procedure and subsequently signed a
written consent form. The following examinations were performed:
Blood pressure, electrocardiogram, blood cell count and coagulation
function tests, including activated partial thromboplastin and
prothrombin time tests. All results were found to be within the
normal ranges.
The CT-guided PCNB procedure was performed by a
radiologist with 11 years of experience with PCNB. A 17-gauge
introducer needle and an 18-gauge cutting biopsy needle (length, 13
cm; TSK Laboratory, Tochigi, Japan) were selected for the
procedure. During the procedure, the patient was placed in a prone
position and instructed to hold her breath when required. Prior to
biopsy, a CT scan of the thorax was performed using a Siemens
Somaton Volume Zoom CT scanner (Siemens, Inc., Erlangen, Germany)
with an 8-mm slice thickness and 8-mm intervals to determine the
flake-shaped lesion in the left lower lobe adjacent to the chest
wall as the target of biopsy.
Once the patient had been moved into the CT gantry
and placed in the desired position, the needle entry site was
marked with indelible ink and radiopaque locators using a gantry
laser alignment light. A brief CT scan was repeated at a position 2
cm above and 2 cm below the selected slice during suspended
respiration. Based on these images, the appropriate table position
and needle trajectories were selected.
The biopsy procedure was conducted as follows:
Following the administration of local anesthesia via an injection
of 2% lidocaine, a 17-gauge introducer needle was inserted into the
prepped skin until the tip of the needle had reached the parietal
pleura. Under CT guidance, the introducer needle was then advanced
with a single motion along the planned trajectory to the prescribed
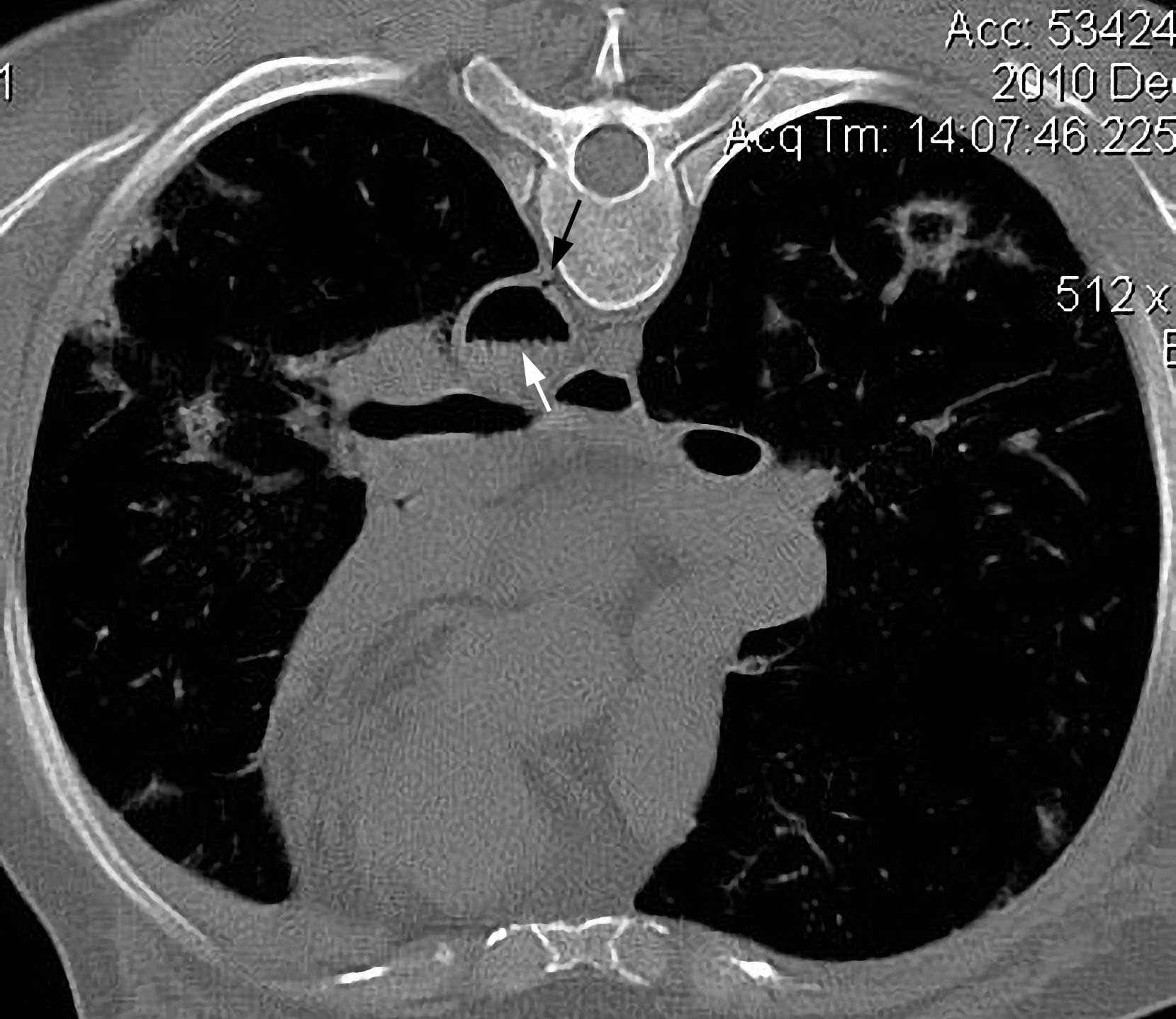
depth required to reach the surface of the lesion. A CT scan was
subsequently obtained to confirm the position of the needle tip
(Fig. 1). Once the needle tip
position had been confirmed, the internal stylet was removed and
immediately replaced by the biopsy needle, which was advanced into
the lesion for specimen procurement. Once the sample was obtained,
the biopsy needle was removed and immediately replaced by the
stylet of the introducer needle. Specimen acquisition was repeated
twice and three core biopsy samples were obtained in total; the
samples were then fixed in 10% neutral buffered formalin. Finally,
the introducer needle was removed. During the procedure, the
patient remained immobile on the CT table, did not cough and held
her breath following moderate expiration, as instructed.
Following the withdrawal of the needle, the patient
exhibited mild cough and hemoptysis. A postprocedural CT scan of
the entire thorax was performed, and a small pneumothorax was
observed (Fig. 2). Following the
removal of the patient from the gantry, the radiologist noted that
the patient was unresponsive and the pulse of the carotid artery
was not palpable. Although immediate cardiopulmonary resuscitation
(CPR) was performed with 100% oxygen (O2) administration
through a respirator, the patient could not be revived and
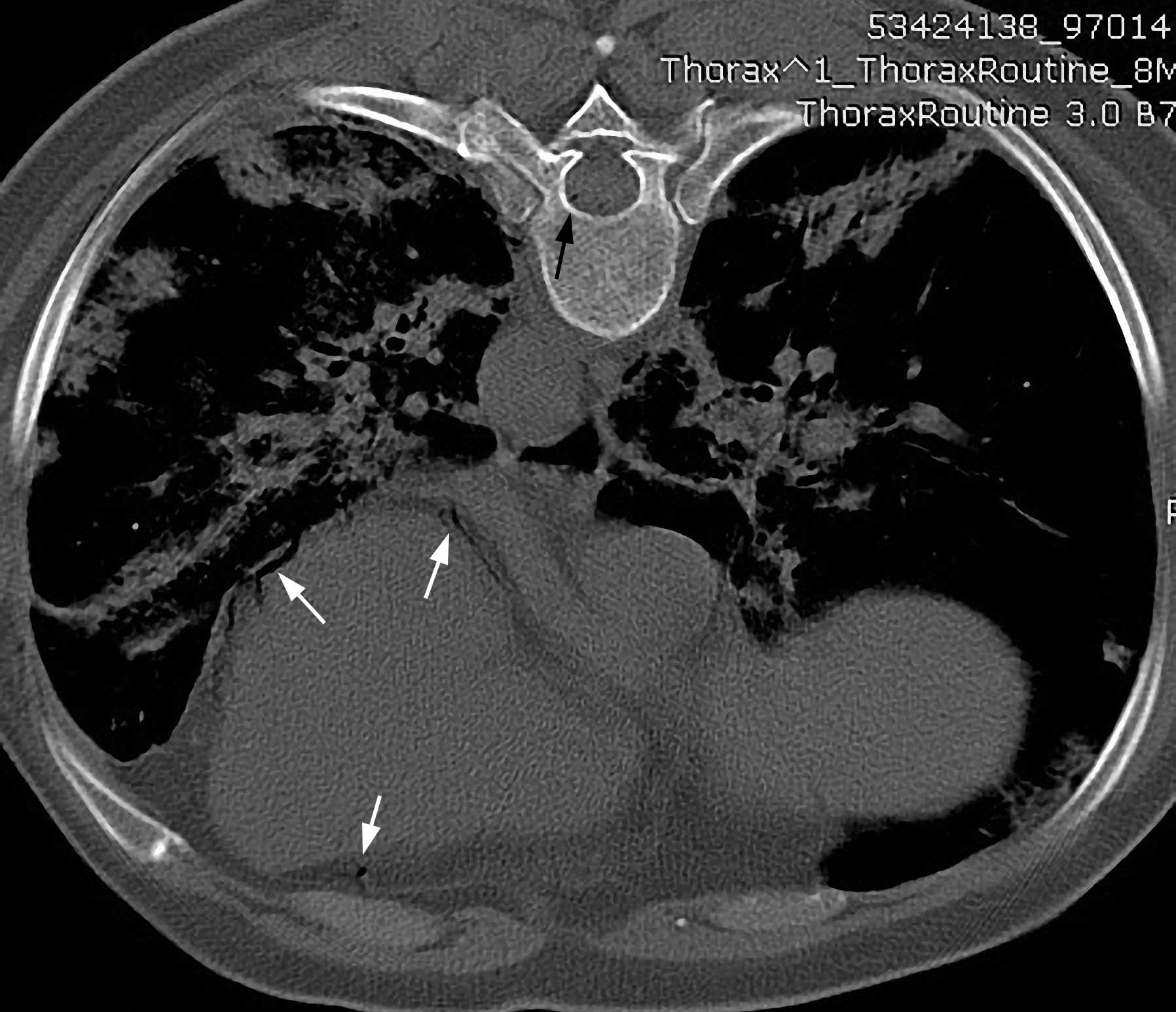
succumbed on the CT table ~1 h after the biopsy. A review of the
postprocedural CT images revealed a considerable volume of air in
the descending aorta and left ventricle and a smaller volume in the
coronary and spinal arteries (Figs.
2 and 3). These findings led to
the diagnosis of air embolism of the left ventricle and systemic
arterial circulation. Histopathology of the obtained specimen
revealed inflammatory lesions.
Discussion
CT-guided PCNB is a well-established and minimally
invasive procedure for the diagnosis of indeterminate pulmonary
lesions. Cases of air embolism as a complication of CT-guided PCNB
are extremely rare, but also life-threatening (1,2);
however, the incidence rate of air embolism is believed to have
been underestimated due to undiagnosed asymptomatic cases.
Single-institutional, retrospective, observational studies based on
the evaluation of CT scan images have suggested a higher incidence
(3–5). Hiraki et al (3) found four cases of air embolism among
1,010 CT-guided lung biopsies based on postprocedural CT scans of
the entire thorax, which gave an incidence rate of 0.4%. Ibukuro
et al (4) estimated an
incidence rate of 0.21%, based on a retrospective review of 1,400
CT-guided lung biopsies. Of note, Freund et al (5) showed that the radiological incidence of
systemic air embolism complicating PCNB was 3.8%, whereas the
clinically apparent incidence was 0.49%. The finding that the
radiological incidence rate of air embolism is considerably higher
than the clinically apparent incidence rate indicates that
asymptomatic cases can lead to an overall underdiagnosis of this
complication. Despite this higher radiological incidence rate,
however, air embolism remains a relatively rare occurrence.
The present study described a case of fatal air
embolism in the coronary and spinal arteries, which occurred
immediately after a CT-guided PCNB of the lung. The patient was the
first case of systemic air embolism among 1,100 lung biopsies
performed over an 11-year time span, since CT-guided PCNB was
introduced at the Second Affiliated Hospital of Dalian Medical
University. To the best of our knowledge, this is also the first
case of CT scan-confirmed air embolism in the spinal artery.
Despite the uncommonness of air embolism, its
consequences can potentially be fatal; the occurrence of systemic
air embolism can cause a rapid deterioration of the patient's
cardiac and/or neurological condition, and requires prompt
management and specialized treatment (5). The clinical manifestations of air
embolism vary, depending on the exact location of the arterial
embolus and the volume of air disseminated into the vessels. Once
air enters the systemic circulation, it is distributed to
respective arterial end beds. The systems most vulnerable to
end-arterial occlusion by these bubbles are the cerebral and
coronary circulation systems, which are sometimes affected
simultaneously (3,5). Even if only a small volume of air
enters the systemic arterial circulation, functional end arteries
can be occluded by air bubbles. An experimental study has
demonstrated that 2 ml air directly injected into the cerebral
circulation is sufficient to have a fatal effect, and that 0.5–1.0
ml air injected into the coronary artery can lead to cardiac arrest
(6). The patient of the present
study suffered sudden cardiac arrest and immediate loss of
consciousness following the lung biopsy. According to the
postprocedural chest CT-scan images, we propose that cardiac arrest
as a result of coronary air embolism directly led to neurological
lesions, due to potential spinal artery embolism, and then sudden
mortality; however, the possibility of air embolisms in the
cerebral circulation cannot be excluded without confirmation by a
brain CT scan. Despite promptly providing CPR with 100%
O2 administration, the severity of the condition did not
allow further diagnosis or definitive therapy.
Due to the frequent performance of CT-guided PCNB of
the lung, case reports of air embolisms complicating the procedure
have been increasing in number. The characteristics of symptomatic
air embolism, based on the present and previously reported cases,
are summarized in the following section (3,7–24). In the majority of cases, the clinical
symptoms of air embolism occur either during or immediately
following needle biopsy. Shi et al (23), however, reported a case with a
delayed onset (6 h after the procedure). Subjects with symptomatic
air embolism usually present with a rapid deterioration of cardiac
and/or cerebral status, which can result in sudden mortality. The
occurrence of air embolism appears to have no association with the
size of the biopsy needle (17-gauge to 23-gauge) or the biopsy
methods, such as fine needle aspiration, needle core biopsy,
automated core biopsy and coaxial needle biopsy. Air embolism has
occurred when patients have suspended respiration during eupnea and
at the end of inhalation or expiration. In these symptomatic cases,
the lesions that underwent biopsy ranged from peripheral to hilar
lesions, and the pulmonary parenchyma was penetrated at a needle
depth of 0.5–6.3 cm (3). Pulmonary
lesions included diffuse, ground-glass opacities, cystic lesions,
solid masses and benign and malignant tumors.
The mechanism of air embolism complicating needle
lung biopsy remains unclear, even following autopsy (20); however, a number of hypotheses have
been proposed regarding possible pathways whereby air is introduced
into the systemic circulation during a needle biopsy of the lung
(9,10). First, air may directly enter the
pulmonary vein through the needle when the tip of the biopsy needle
is lodged in a pulmonary vein and communicates between the
pulmonary vein and the atmosphere when the inner stylet is removed
and the atmospheric pressure exceeds the pulmonary venous pressure.
Secondly, when a needle simultaneously traverses the alveolus and
the pulmonary artery, air can access the pulmonary arterial system
and reach the pulmonary venous circulation by traversing the
pulmonary microvasculature. Thirdly, bronchial-venous or
alveolar-venous fistulas may develop when a needle simultaneously
traverses an air-containing space (e.g., alveolar, bronchus,
cavitary or cystic lesion) and adjacent pulmonary vein, allowing
air to enter the pulmonary vein when the patient coughs or the
Valsalva maneuver is performed, both of which can increase airway
pressure beyond pulmonary venous pressure. Cases of air embolism
without any obvious triggers (e.g. cough, Valsalva maneuver and
positive pressure ventilation) may be associated with a quiet
expiration that forwards air into the pulmonary vein. In the
present study, it appeared improbable that air had entered the
pulmonary vein directly through the needle, since the hollow of the
needle was kept occluded at all times and the patient suspended
respiration as instructed during the biopsy. Considering the rapid
deterioration of the patient's condition and the large volume of
air detected in the systemic circulation by CT scan, we
hypothesized that the formation of an alveolar-venous or
bronchial-venous fistula was the most probable cause of air
embolism.
Studies have indicated that pathological pulmonary
abnormalities may predispose a patient to an increased risk of air
embolism (12,24). It is believed that, following lung
biopsy and needle withdrawal, a large number of alveolar-venous or
bronchial-venous fistulas can develop along the needle trajectory.
During vascular injury, the walls of small vessels usually retract,
adhere spontaneously and become sealed. Extravasated and then
coagulated blood may promote extravascular tamponade, which can
prevent air in the alveoli or bronchi from entering the vein;
however, pathological pulmonary abnormalities, such as
inflammation, forms of vasculitis, e.g. Wegener's granulomatosis,
and interstitial disease, which are risk factors of air embolism,
may interfere with the healing process and result in prolonged
exposure of the vessel lumen to the airway (3,24).
Ghafoori and Varedi (11) presumed that an increased probability
of air embolism could be associated with the size of the needle and
the coaxial techniques. It has been suggested that larger gauge
needles are associated with an increased risk of involving the
pulmonary vein and coaxial system, which, following the removal of
the internal stylet, is associated with an increased risk of
contact with the atmosphere. This postulation, however, is
controversial, since a case of systemic air embolism that used fine
needles and did not involve the coaxial method has been reported
(21).
Identifying the risk factors for air embolism and
understanding their mechanisms will facilitate the development and
implementation of adequate preventive measures prior to and during
biopsy. Several precautionary measures have been proposed in order
to minimize the risk of air embolism, such as avoiding biopsy
through cystic or cavitary lesions or bullae, using a stylet to
keep the needle closed airtight throughout the procedure,
instructing the patient to suspend breathing during manipulation of
the biopsy needle and minimizing the amount of aerated lung tissue
penetrated while attempting to reach the lesion (12,22).
In the present case, the clinical suspicion of
systemic air embolism was based on the initial clinical
manifestation: A rapid deterioration of the
neurological/cardiovascular status. The postprocedural CT scan of
the entire thorax, rather than just the target area of the biopsy,
was essential in order to provide a definitive diagnosis and to
detect evidence of air density in the pulmonary vein, left atrium
and ventricle and systemic circulation (7). We propose that a CT scan of the brain
be considered whenever manifestations of cerebral abnormalities
occur during or following lung biopsy.
When a patient exhibits any suspicious symptoms of
air embolism during biopsy, the needle has to be instantly removed.
In such a case, it is recommended that the patient is placed in
either the right lateral decubitus or Trendelenburg position, which
can prevent air from entering the systemic circulation from the
left ventricle, with immediate administration of 100% O2
(25). Prompt CPR is necessary for a
patient with a potentially fatal air embolism, and the
stabilization of vital signs is the primary goal of treatment. In
addition, hyperbaric O2 therapy is a definitive therapy
for systemic air embolism and has been demonstrated to improve
survival rate and neurological recovery. This therapy should be
administered as soon as initial stabilization has been achieved
(8,12).
In the present case, a fatal air embolism
complicating CT-guided lung biopsy occurred, despite the proximity
of the lesion that underwent biopsy to the chest wall. During the
procedure, the patient did not cough and was instructed to suspend
breathing when required. The biopsy was performed by an experienced
radiologist. Although previous studies have made certain
recommendations and proposed certain precautions that could
contribute to the reduction of the risk of air embolism, none of
these proposals has succeeded in completely removing the risks. In
order to achieve optimal outcomes for the patient, prompt
recognition and urgent resuscitation are crucial for initial
stabilization, following which a diagnostic confirmation can be
made and definite treatments can be initiated. Standardized
protocols for the early recognition and management of this rare but
life-threatening complication should be developed.
Acknowledgements
The authors would like to thank Professor Changhong
Liu and Professor Xu Zhang of the Department of Thoracic Surgery
and Professor Ning Zhu of the Department of Cardiology of the
Second Affiliated Hospital, Dalian Medical University for their
contributions to this study.
References
|
1
|
Richardson CM, Pointon KS, Manhire AR and
Macfarlane JT: Percutaneous lung biopsies: A survey of UK practice
based on 5,444 biopsies. Br J Radiol. 75:731–735. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Tomiyama N, Yasuhara Y, Nakajima Y, Adachi
S, Arai Y, Kusumoto M, Eguchi K, Kuriyama K, Sakai F, Noguchi M, et
al: CT-guided needle biopsy of lung lesions: A survey of severe
complication based on 9783 biopsies in Japan. Eur J Radiol.
59:60–64. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hiraki T, Fujiwara H, Sakurai J, Iguchi T,
Gobara H, Tajiri N, Mimura H and Kanazawa S: Nonfatal systemic air
embolism complicating percutaneous CT-guided transthoracic needle
biopsy: Four cases from a single institution. Chest. 132:684–690.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ibukuro K, Tanaka R, Takeguchi T, Fukuda
H, Abe S and Tobe K: Air embolism and needle track implantation
complicating CT-guided percutaneous thoracic biopsy:
Single-institution experience. AJR Am J Roentgenol. 193:W430–W436.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Freund MC, Petersen J, Goder KC, Bunse T,
Wiedermann F and Glodny B: Systemic air embolism during
percutaneous core needle biopsy of the lung: Frequency and risk
factors. BMC Pulm Med. 12:22012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ho AM and Ling E: Systemic air embolism
after lung trauma. Anesthesiology. 90:564–575. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ohashi S, Endoh H, Honda T, Komura N and
Satoh K: Cerebral air embolism complicating percutaneous
thin-needle biopsy of the lung: Complete neurological recovery
after hyperbaric oxygen therapy. J Anesth. 15:233–236. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sato K, Miyauchi K, Shikata F, Murakami T,
Yoshioka S and Kawachi K: Arterial air embolism during percutaneous
pulmonary marking under computed tomography guidance. Jpn J Thorac
Cardiovasc Surg. 53:404–406. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Mansour A, AbdelRaouf S, Qandeel M and
Swaidan M: Acute coronary artery air embolism following CT-guided
lung biopsy. Cardiovasc Intervent Radiol. 28:131–134. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Cheng HM, Chiang KH, Chang PY, Chou YF,
Huang HW, Chou AS and Yen PS: Coronary artery air embolism: A
potentially fatal complication of CT-guided percutaneous lung
biopsy. Br J Radiol. 83:e83–e85. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ghafoori M and Varedi P: Systemic air
embolism after percutaneous transthoracic needle biopsy of the
lung. Emerg Radiol. 15:353–356. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Um SJ, Lee SK, Yang DK, Son C, Kim KN, Lee
KN and Kim YS: Four cases of a cerebral air embolism complicating a
percutaneous transthoracic needle biopsy. Korean J Radiol.
10:81–84. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Bou-Assaly W, Pernicano P and Hoeffner E:
Systemic air embolism after transthoracic lung biopsy: A case
report and review of literature. World J Radiol. 2:193–196. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Higashino T, Noma S, Nishimoto Y, Endo J,
Taguchi Y and Shindo T: Cerebral air embolism as a complication of
computed tomography-guided marking of the lung: Depiction of air
inflow route from a pulmonary vein to the left atrium. J Thorac
Imaging. 26:W26–W29. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Hirasawa S, Hirasawa H, Taketomi-Takahashi
A, Morita H, Tsushima Y, Amanuma M and Endo K: Air embolism
detected during computed tomography fluoroscopically guided
transthoracic needle biopsy. Cardiovasc Intervent Radiol.
31:219–221. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Lederer W, Schlimp CJ, Glodny B and
Wiedermann FJ: Air embolism during CT-guided transthoracic needle
biopsy. BMJ Case Rep. 30:20112011.
|
|
17
|
Wu YF, Huang TW, Kao CC and Lee SC: Air
embolism complicating computed tomography-guided core needle biopsy
of the lung. Interact Cardiovasc Thorac Surg. 14:771–772. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Singh A, Ramanakumar A and Hannan J:
Simultaneous left ventricular and cerebral artery air embolism
after computed tomographic-guided transthoracic needle biopsy of
the lung. Tex Heart Inst J. 38:424–426. 2011.PubMed/NCBI
|
|
19
|
Kuo HL, Cheng L and Chung TJ: Systemic air
embolism detected during percutaneous transthoracic needle biopsy:
Report of two cases and a proposal for a routine postprocedure
computed tomography scan of the aorto-cardiac region. Clin Imaging.
34:53–56. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Arnold BW and Zwiebel WJ: Percutaneous
transthoracic needle biopsy complicated by air embolism. AJR Am J
Roentgenol. 178:1400–1402. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kamiyoshihara M, Sakata K, Ishikawa S and
Morishita Y: Cerebral arterial air embolism following CT-guided
lung needle marking. Report of a case. J Cardiovasc Surg (Torino).
42:699–700. 2001.PubMed/NCBI
|
|
22
|
Lattin G Jr, O'Brien W Sr, McCrary B,
Kearney P and Gover D: Massive systemic air embolism treated with
hyperbaric oxygen therapy following CT-guided transthoracic needle
biopsy of a pulmonary nodule. J Vasc Interv Radiol. 17:1355–1358.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Shi L, Zhang R, Wang Z and Zhou P: Delayed
cerebral air embolism complicating percutaneous needle biopsy of
the lung. Am J Med Sci. 345:501–503. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Kau T, Rabitsch E, Celedin S, Habernig SM,
Weber JR and Hausegger KA: When coughing can cause stroke-a
case-based update on cerebral air embolism complicating biopsy of
the lung. Cardiovasc Intervent Radiol. 31:848–853. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Balsara ZN and Burks DD: Hyperbaric oxygen
therapy for arterial air embolism. AJR Am J Roentgenol.
188:W982007. View Article : Google Scholar : PubMed/NCBI
|