Introduction
Scabies is an itchy and highly contagious skin
disease. It is caused by an infestation by the mite Sarcoptes
scabiei. The disease is transmitted via direct skin-to-skin
contact, and severe and relentless itching is its predominant
symptom. The superficial burrows of scabies are most commonly found
on the hands, feet, wrists, elbows, back, buttocks and external
genitals (1). The majority of
dermatologists are familiar with the diagnosis of typical scabies.
However, elderly patients occasionally develop crusted scabies,
also known as Norwegian scabies (2).
A few cases of bullous scabies resembling bullous pemphigoid have
also been reported (3–6). The present study reports the case of an
elderly patient who presented with crusted scabies combined with
bullous scabies.
Case report
A 73-year-old woman developed a generalized itchy
papular eruption that particularly affected the trunk, arms and
thighs and was present for >3 months. Initially, the patient was
diagnosed with drug-induced eczema, which was treated with
antihistamine and topical corticosteroids. However, the therapeutic
effects were unsatisfactory and the intense itching remained.
Approximately 3 days prior to admission to the First Affiliated
Hospital of Chongqing Medical University (Chongqing, China) bullous
lesions started to form and spread gradually on the bilateral
thighs. There was no history of similar problems in the patient's
family.
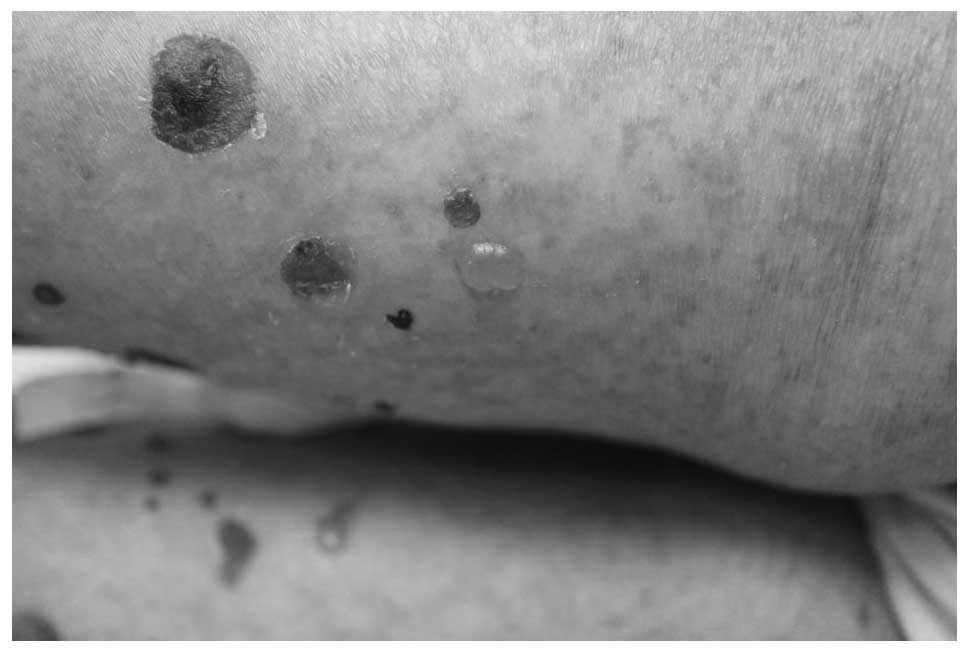
Clinical examination identified erythematous or
brownish erythematous and scabbed papular lesions on the patient's
trunk and limbs (Fig. 1). The skin
was generally dry and scaly (Fig.
2). Blisters were present on inner side of her bilateral thighs
and some of these were blood blisters (Fig. 3). Nikolsky sign testing of the
blisters was negative. The general physical examination was normal.
Biopsy of a tense bulla excised from the left thigh revealed the
formation of an subepidermal blister. A small amount of cellular
infiltration consisting mainly of neutrophils and eosinophils
within the blister and in the upper dermis was observed. The
results of direct and indirect immunofluorescence tests, aiming to
make a differential diagnosis of other skin disorders, such as
pemphigus and Bullous pemphigoid, were negative. Laboratory tests
demonstrated that the patient had a reduced red blood cell count
(3.30×1012/l) and hematocrystallin level (105.0 g/l).
Liver and kidney function, antinuclear antibody spectrum and HIV
tests were normal.
A diagnosis of bullous pemphigoid was made, and the
patient was prescribed oral prednisolone (40 mg/day) and topical
corticosteroids. However, the symptoms persisted. The therapeutic
effects of antihistamines and other antipruritic agents were
unsatisfactory. The itching worsened at night. No other
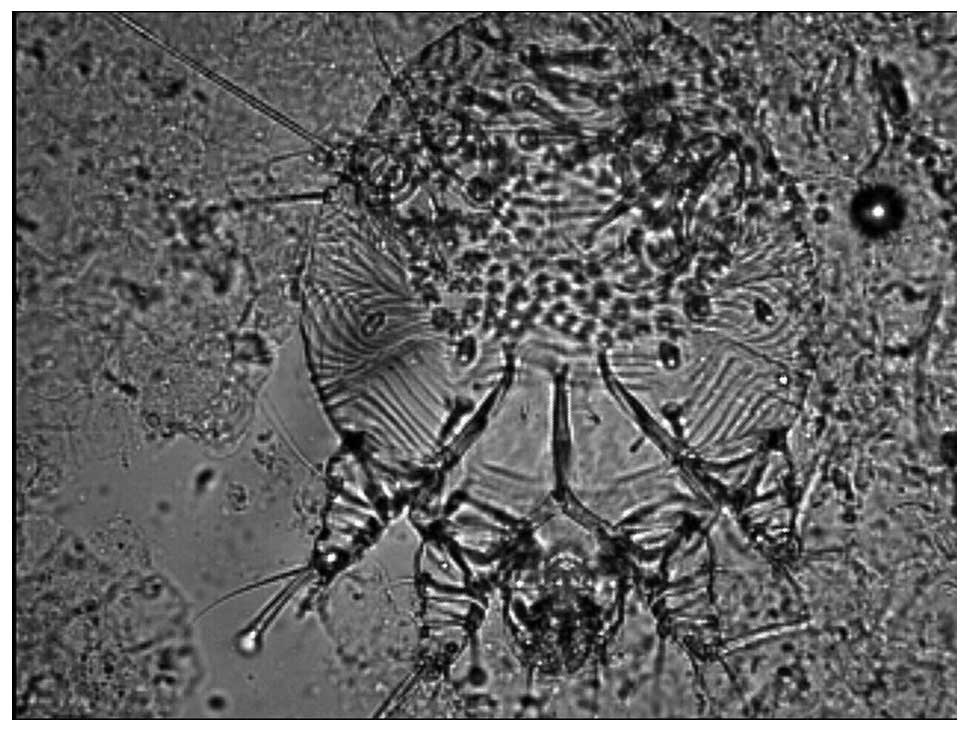
abnormalities were detected. Subsequently, direct microscopy of
scrapings from papules on the fingers revealed mites and eggs of
Sarcoptes scabiei (Fig. 4).
The clinical and pathological features, therapeutic response and
detection of scabies mites enabled the patient to be diagnosed as
having Norwegian scabies combined with bullous scabies. Therefore,
the patient was treated with 10% sulfur cream for ~7 days, which
resulted in a mild amelioration of the papules and pruritus. The
patient subsequently made a complete recovery and no recurrence was
observed during a 12-month follow-up. The present study was
approved by the Ethics Committee of the First affiliated hospital
of the Chongqing Medical University, and written informed consent
was obtained from each patient prior to the start of the study.
Discussion
To the best of our knowledge, there are very few
reports concerning Norwegian scabies combined with bullous scabies.
Scabies is usually clinically divided into common scabies and
crusted scabies. Crusted scabies, also known as Norwegian scabies,
is a more severe form usually associated with immunosuppression
(7). This disorder is very easy to
misdiagnose. When it is treated as a drug-induced eruption, eczema
or other disease with glucocorticoid, this may exacerbate the
scabies and cause blisters to develop from the original skin
lesions, as in the present case where the patient was initially
treated with prednisolone for eczema and bullous pemphigoid.
Although, scabies may present with a variety of
symptoms and signs, patients with scabies rarely present with
bullae. Patients with scabies and bullae are often misdiagnosed as
having bullous pemphigoid. In fact, clinically, it is extremely
challenging to distinguish between bullous pemphigoid and bullous
scabies, particularly when skin scrapings do not show any mites or
eggs. Light microscopy is also not sufficient to distinguish
between these diseases. In the present case, the light microscopy
of a blister revealed a subepidermal bulla on the dermoepidermal
junction. These results were consistent with bullous pemphigoid.
However, there are some differentiating features. Firstly, although
bullous scabies can affect individuals of any age, bullous
pemphigoid is more common in the elderly. While true bullous
pemphigoid always shows linear C3 or IgG deposition in the basement
membrane zone (BMZ), bullous scabies may show linear and granular
deposition in the BMZ, particularly when the result of indirect
immunofluorescence testing is negative (8). In the present case, the results of
direct and indirect immunofluorescence examinations were negative,
which is consistent with the diagnosis of bullous scabies. The
itchiness and severity of bullous scabies may be worse at night.
With bullous scabies, there is sometimes is a family history, since
the disease is a contagious infestation. Lastly, bullous pemphigoid
usually exhibits a good response to oral prednisolone while bullous
scabies can persist and is relieved quickly by antiscabies
drugs.
Immunopathogenesis is considered to play an
important role in the development of bullous scabies. It has been
suggested that the bullous pemphigoid-like eruptions in scabies are
caused by the induction of BMZ-reactive autoantibodies by scabies
mites. Mites may injure the BMZ directly or through their lytic
enzymes, resulting in a change in or release of bullous pemphigoid
antigen and, subsequently, the initiation of an immunological
response with autoantibody production (9,10).
Therefore, the deposition of C3 or IgG in the BMZ can sometimes be
observed. Alternatively, a mite component may play an antigenic
role that cross-reacts with the bullous pemphigoid antigen
resulting in auto-antibody production (11). Some cases test positive for cultures
for Staphylococcus aureus. In such cases, bullous lesions
might result from superinfection with S. aureus, with a
mechanism similar to the development of blisters in bullous
impetigo (6,12). However, the exact mechanism of
bullous lesion development requires further evaluation.
Physicians should be aware of the possibility of
bullous scabies in patients who have bullous pemphigoid-like
eruptions associated with pruritic papules that show a poor
response to steroids. However, scabies infestation-induced bullous
pemphigoid should be included in the differential diagnosis.
Steroids are ineffective for the treatment of bullous scabies, and
classical antiscabieticides are the best treatment options. The
present case was successfully treated topically with 10% sulfur
cream. When topical treatment is difficult, ivermectin (200 mg/kg
orally) is an alternative effective option.
References
|
1
|
Hicks MI and Elston DM: Scabies. Dermatol
Ther. 22:279–292. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kolar KA and Rapini RP: Crusted
(Norwegian) scabies. Am Fam Physician. 44:1317–1321.
1991.PubMed/NCBI
|
|
3
|
Nakamura E, Taniguchi H and Ohtaki N: A
case of crusted scabies with a bullous pemphigoid-like eruption and
nail involvement. J Dermatol. 33:196–201. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Balighi K, Robati RM and Hejazi N: A
dilemma: Bullous-pemphigoid-like eruption in scabies or
scabies-induced bullous pemphigoid. Dermatol Online J.
12:132006.PubMed/NCBI
|
|
5
|
Gutte RM: Bullous scabies in an adult: A
case report with review of literature. Indian Dermatol Online J.
4:311–313. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ansarin H, Jalali MH, Mazloomi S,
SoltaniArabshahi R and Setarehshenas R: Scabies presenting with
bullous pemphigoid-like lesions. Dermatol Online J.
12:192006.PubMed/NCBI
|
|
7
|
Towersey L, Cunha MX, Feldman CA, Castro
CG and Berger TG: Dermoscopy of Norwegian scabies in a patient with
acquired immunodeficiency syndrome. An Bras Dermatol. 85:221–223.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Salo OP, Reunala T, Kalimo K and Rantanen
T: Immunoglobulin and complement deposits in the skin and
circulating immune complexes in scabies. Acta Derm Venereol.
62:73–76. 1982.PubMed/NCBI
|
|
9
|
Veraldi S, Scarabelli G, Zerboni R, Pelosi
A and Gianotti R: Bullous scabies. Acta Derm Venereol. 76:167–168.
1996.PubMed/NCBI
|
|
10
|
Kaur S and Thami GP: Bullous scabies in an
adult. Clin Exp Dermatol. 28:93–94. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ostlere LS, Harris D and Rustin MH:
Scabies associated with a bullous pemphigoid-like eruption. Br J
Dermatol. 128:217–219. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Herman PS: Letter: Scabies and bullae.
JAMA. 231:11341975. View Article : Google Scholar : PubMed/NCBI
|