Introduction
Primary synovial chondromatosis is a rare, benign,
proliferative cartilaginous lesion that can arise from the tendon
sheath, bursa or joint synovial tissue (1,2).
Tenosynovial chondromatosis is an extra-articular version of
articular synovial chondromatosis, and it is most commonly observed
in the fingers and feet. Tenosynovial chondromatosis has rarely
been reported in the publicly available literature and is often
erroneously classified as a cartilage or soft tissue tumor. In
addition, numerous patients with tenosynovial chondromatosis are
asymptomatic, and the histological diagnosis can be challenging
(3). The present study describes a
case of tenosynovial chondromatosis in the finger tendon sheath of
a 23-year-old male patient. The literature associated with
tenosynovial chondromatosis affecting the fingers is also
reviewed.
Case report
A 23-year-old male patient was admitted to the Third
Affiliated Hospital of Sun Yat-Sen University (Guangzhou, China)
with a history of pain and progressive swelling at the proximal
interphalangeal joint of the left ring finger for the past 2 years.
The symptoms and decreased range of motion of the
metacarpophalangeal joint were greatly affecting the patient's
daily life in the weeks leading up to his admission. The patient
recalled no history of trauma or overuse of the left hand. A
physical examination of the finger revealed an ~3×2 cm irregular
mass at the volar aspect of the ring finger. The mass had a hard
texture, clear boundary and mild tenderness with pressure. The left
ring finger metacarpophalangeal joint had a decreased range of
motion of 60°. Blood biochemistry for the patient was unremarkable.
Preoperative ultrasonography of the left ring finger revealed
multiple nodules with well-defined boundaries in the tendon sheath.
Since chondromatosis rarely occurs extra-articularly, the nodules
were initially and preliminarily diagnosed as a chondroma of the
soft tissue parts.
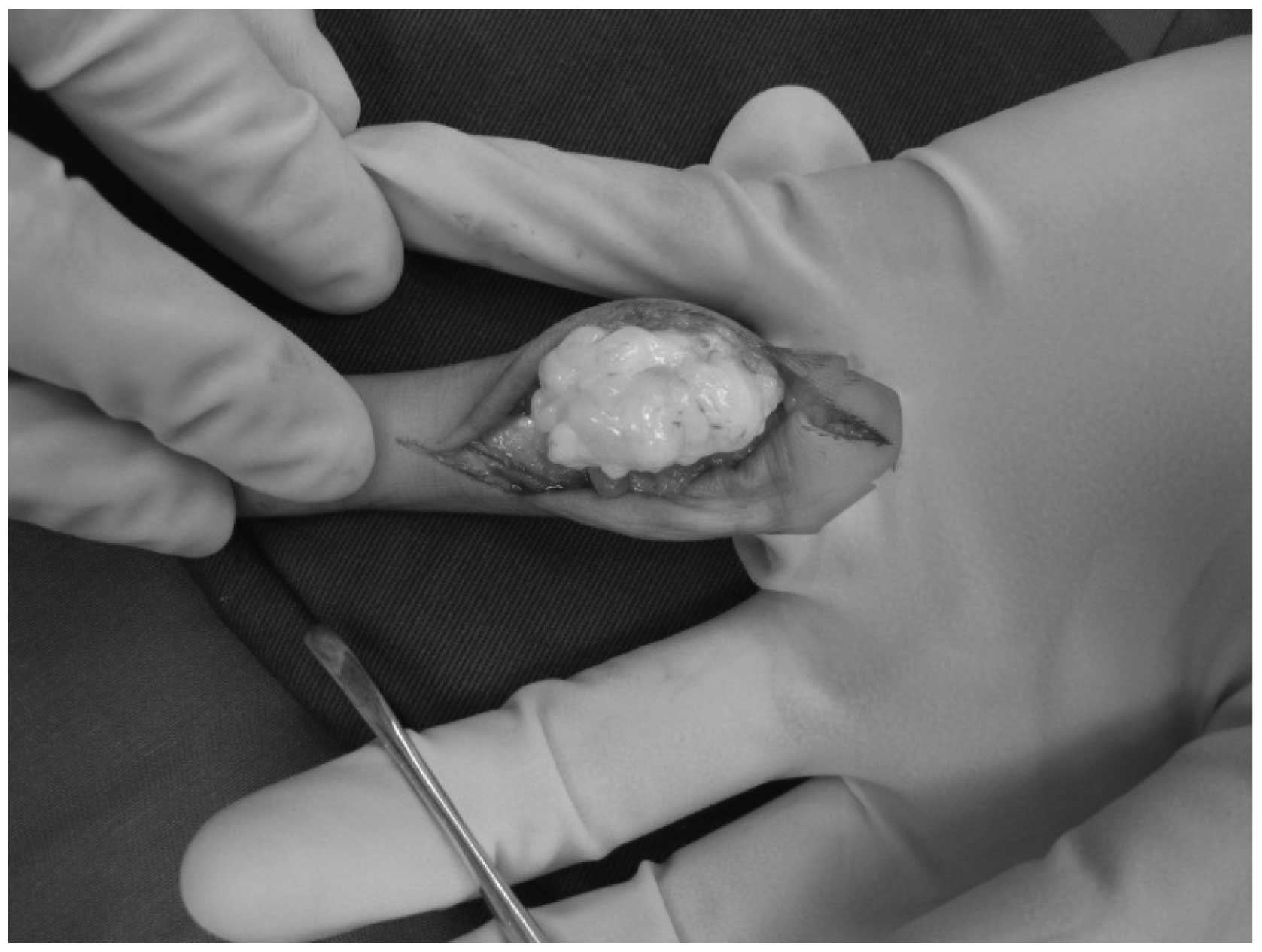
Surgical resection of the nodules was performed.
Under brachial plexus anesthesia, a ‘Z’-shaped incision was made at
the volar aspect of the left ring finger proximal phalanx to expose
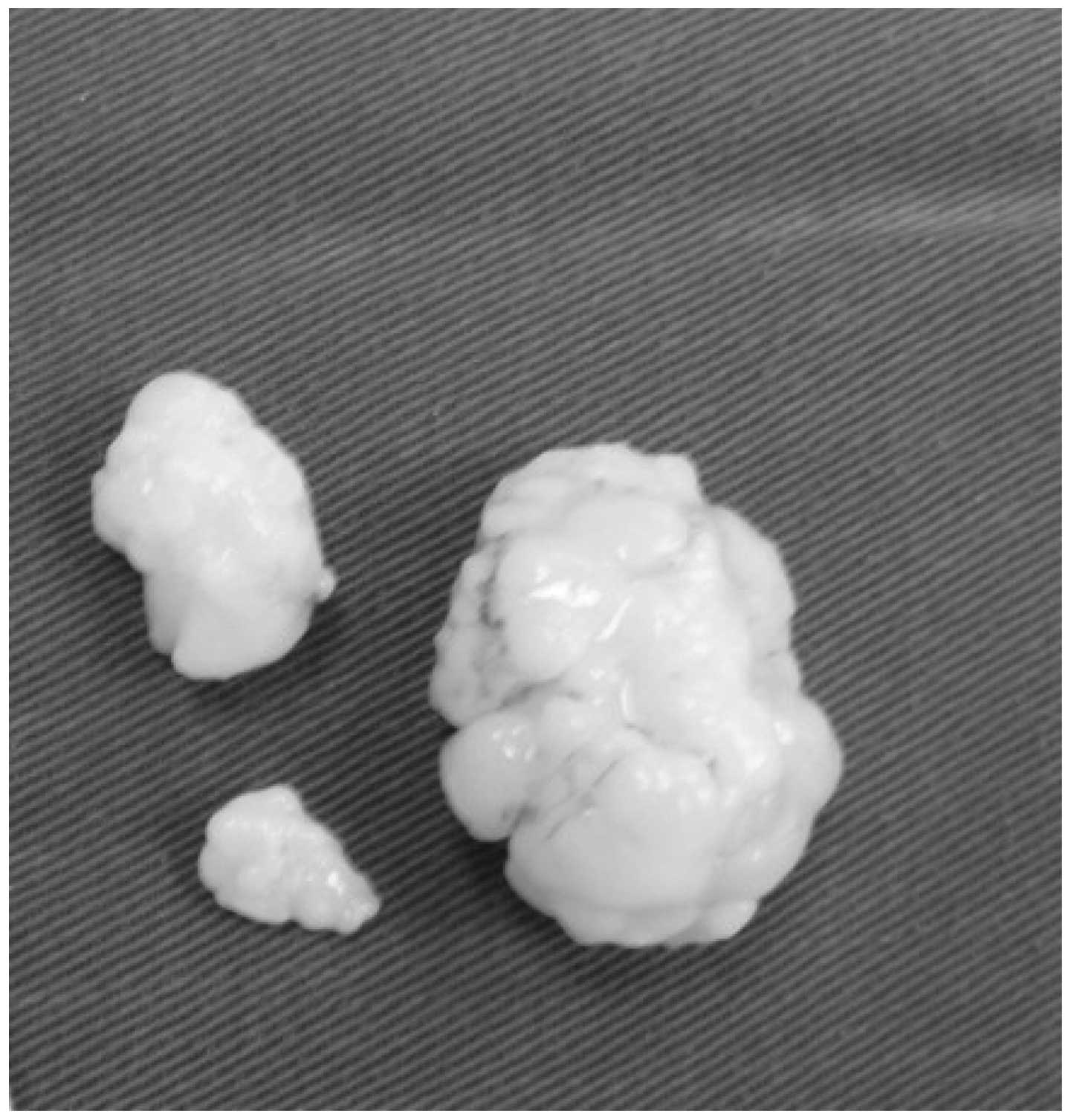
the subcutaneous tumor. Three different-sized nodules were excised
(2.0×1.5, 1.2×0.6 and 0.7×0.3 cm) during surgery. The nodules were
encapsulated loose white bodies in the flexor tendon sheath, with a
hard texture and smooth surface (Figs.
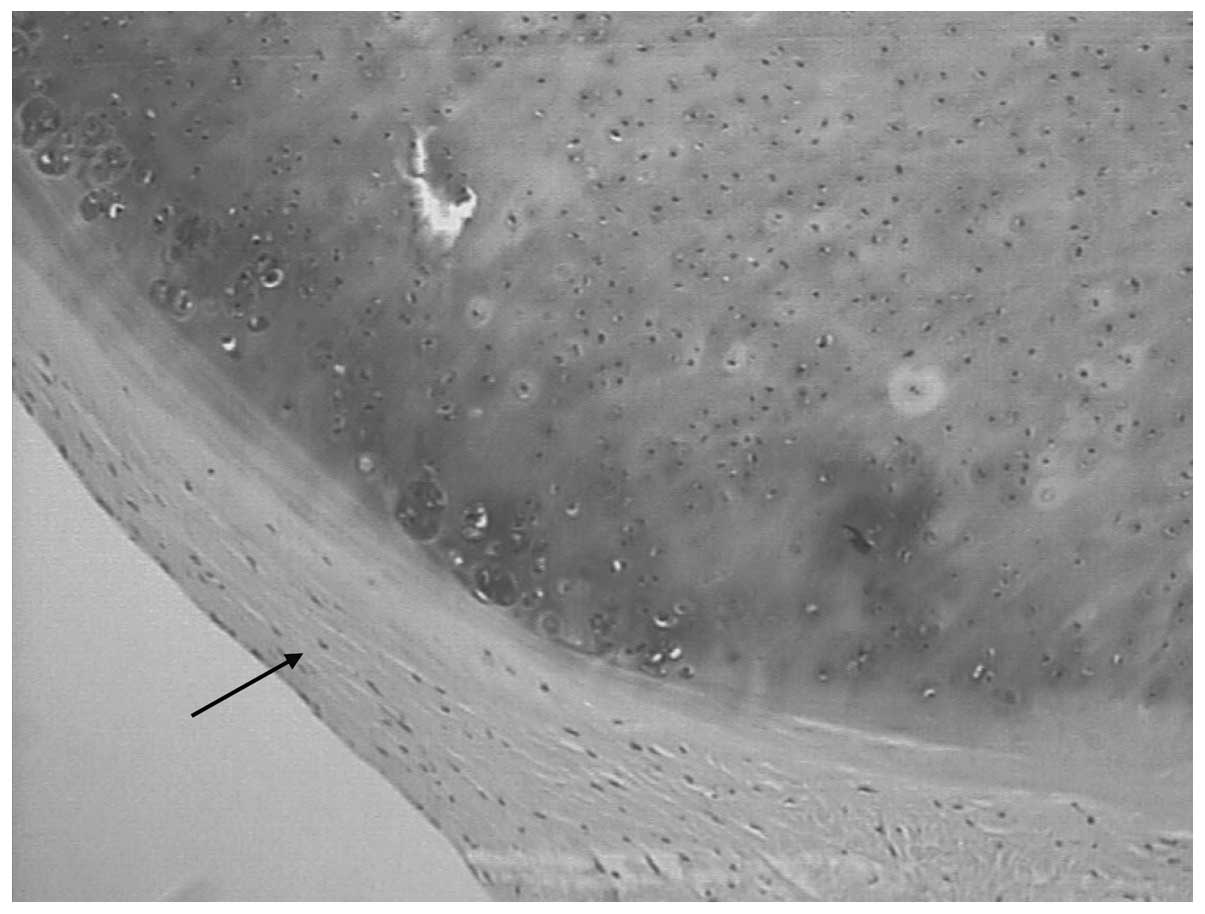
1 and 2). Histopathological
examination of the nodules revealed increased chondrocyte
cellularity and a fibrous capsule, consistent with a diagnosis of
tenosynovial chondromatosis (Fig.
3). The patient was symptom free 6 months postoperatively. At a
follow-up 1 year after that, there were no signs of recurrence.
Discussion
Synovial chondromatosis is a rare condition
characterized by the formation of multiple cartilaginous nodules in
the synovial membrane. Synovial cells are similar to mesenchymal
stem cells and are capable of giving rise to cartilage or bone
tissue under specific conditions (4). Synovial chondromatosis can involve the
joints (articular synovial chondromatosis) and the tendon sheath
(tenosynovial chondromatosis). While both intra-articular and
extra-articular synovial chondromatosis are histologically very
similar, they are distinct entities with regard to surgical
strategies and recurrence rate (5).
Various names have been given to the nodules found
in the tendon sheath, including synovial chondromatosis, synovial
cartilage metaplasia, tenosynovial osteochondroma, cartilage and
soft tissue benign tumors, and soft tissue tumors. A previous study
proposed that all these diagnoses were essentially tenosynovial
chondromatosis (6). The proper
diagnosis of tenosynovial chondromatosis is clinically challenging
due to its rarity, particularly when no calcification or
ossification is present in the tumor (2,3).
Secondary synovial chondromatosis is caused by degenerative or
traumatic lesions, which lead to the formation of intra-articular
cartilage.
In 1977, Milgram described synovial chondromatosis
as occurring in the following three distinct phases: i) active
intrasynovial disease with no free loose bodies; ii) transitional
lesions with osteochondral nodules in the synovial membrane and
osteochondral bodies lying free within the joint cavity; and iii)
multiple free osteochondral bodies with quiescent intrasynovial
disease (5,7).
Tenosynovial chondromatosis most frequently affects
the hands and feet (8). A total of
26 cases of tenosynovial chondromatosis in the fingers, including
the present case, have been documented in the literature (1–4,6,8,9). These cases include 14 males and 13
females, ranging from 30 to 60 years of age. The right hand (16
cases) was more frequently affected than the left hand (8 cases).
In the two remaining cases, there was one incidence of bilateral
disease, and 1 case where the affected hand was not specified.
There have been 5 cases of tenosynovial chondromatosis in the
thumb, 3 cases affecting the index finger, 9 cases affecting the
middle finger, and 5 cases affecting the ring or pinky finger. The
flexor tendon was involved in all of the reported cases, but the
extensor tendon was never involved. Patients with tenosynovial
chondromatosis usually present with no history of trauma. The two
most common symptoms are painless swelling that can occur over
several months to several years and mild tenderness when pressure
is applied. Many patients are asymptomatic, while others develop a
trigger finger deformity or carpal tunnel syndrome. Due to the
atypical clinical manifestations and the slow disease process,
clinical treatment for tenosynovial chondromatosis is often delayed
(3,4,9).
Plain radiography of tenosynovial chondromatosis may
show extra-articular soft tissue swelling with multiple small
calcifications or ossifications. A large calcified body with
clusters may suggest a lobular mass (3,5,7). Synovial swelling may lead to bone
corrosion, though a periosteal reaction is rarely observed. In
patients with a long history of tenosynovial chondromatosis, round,
oval or elongated mineralizations can be seen within the tendon
sheath, although the adjacent joint is usually not affected.
Computed tomography (CT) of tenosynovial
chondromatosis can clearly identify the calcified nodules and their
exact locations as well as cortical erosion (10). Detection of tenosynovial
chondromatosis with magnetic resonance imaging (MRI) depends on the
degree to which the nodules have mineralized. In the majority of
cases, the nodules display a muscle-like signal intensity on
T1-weighted images and exhibit high signal intensity on T2-weighted
images (11). In the present case,
preoperative ultrasonography revealed multiple nodules with
well-defined boundaries in the tendon sheath. Thus, ultrasonography
represents a convenient and cost-effective alternative to CT or MRI
for the detection of tenosynovial chondromatosis.
Gross examination of the excised tumor often shows
multiple, white, transparent, lobular cartilage nodules, which are
easily isolated from the synovial tendon sheath. There can be
thousands of nodules of various shapes, ranging in size from a few
millimeters to several centimeters, located in the synovial
membrane or synovial tendon sheath. In the majority of cases of
tenosynovial chondromatosis, closely packed smaller cartilage
nodules in the tendon sheath merge into larger nodules (1,5,6). Histopathologic examination may show
hyaline cartilage nodules surrounded by synovial membrane.
Chondrocytes show mild or moderate atypia. Certain cases show a
mucinous change, calcification or ossification, with nodules
surrounded by giant cells. As the histologic appearance of
tenosynovial chondromatosis is atypical, an erroneous diagnosis of
chondrosarcoma can easily be made. However, chondrosarcoma rarely
occurs in the hands or feet, a fact that can aid in the
differential diagnosis (1,3,5).
Tenosynovial chondromatosis should be differentiated
from several other lesions that give rise to bone cartilage
formation. Soft tissue tumors should be considered first, as they
occur more frequently than synovial chondromatosis and have a much
lower recurrence rate. Soft tissue tumors are usually solitary,
well-encapsulated, and generally occur in a younger patient
population, ranging from 10 to 39 years of age. This disease has
rarely been reported to have malignant transformation (3,5,12). Chondrosarcoma should also be
considered due to a small risk for malignant transformation.
Evidence of aggressive behaviors through imaging, such as cortical
erosion or periosteal reaction, is indicative of chondrosarcoma
with malignancy. A definitive diagnosis of chondrosarcoma results
from histologic findings, as chondrosarcoma predominantly
originates from the bone (5).
Secondary synovial chondromatosis is usually caused by
osteochondral fracture or joint surface exfoliation. Periosteal
chondroma mainly occurs in children and young adults and
predominantly affects the proximal humerus (6). Other differential diagnoses that can be
ruled out by a histologic examination include tenosynovial giant
cell tumor, calcifying aponeurotic fibroma, tumoral calcinosis,
hydroxy-apatite deposition disease, a foreign body, and
inflammatory arthritis.
Tenosynovial chondromatosis is characterized by a
slow progression that can last for decades. There are also reports
that the nodules can spontaneously be resorbed (12). Malignant chondrosarcoma has been
documented in 5% of 53 cases of synovial chondromatosis (13). By contrast, to the best of our
knowledge, no malignant cases of tenosynovial chondromatosis have
been reported. Although the association between complete synovial
excision and the low relapse rate is not yet clear, most doctors
recommend complete removal the loose bodies. Therefore, delicate
surgical dissection around the nodules and satellite nodules and a
synovectomy are necessary (3,12). In
the present case, the patient underwent successful surgical removal
of the loose bodies and the surrounding synovial membrane and was
followed up for 1.5-years without recurrence.
The reported recurrence rates for tenosynovial
chondromatosis vary considerably. In some studies with relatively
small sample sizes, no recurrence or a very low recurrence rate was
reported. However, one study reported a high recurrence rate of 88%
in a larger cohort of 37 cases of tenosynovial chondromatosis in
the hands and feet (6). The
recurrence of synovial chondromatosis or tenosynovial
chondromatosis can take several months to several years (4–6,9).
The literature reviewed in this study indicate that
no available methods are able to apply to the total nature of
synovial chondromatosis preoperatively. However, ultrasonography
may represent a convenient and cost-effective alternative to CT or
MRI imaging for early diagnosis. As for treatment, resection is the
preferred method for synovial chondromatosis.
Acknowledgements
This study was supported by the Science and
Technology Program of Guangzhou (No. 2011Y1-00033-4)
References
|
1
|
Khadilakar MS, Patil AA, Shah NS, Deshmukh
SD and Anand M: Extra-osseous tenosynovial chondromatosis of the
middle finger: A case report. J Orthop Surg (Hong Kong).
20:406–408. 2012.PubMed/NCBI
|
|
2
|
Gil Albarova, Morales-Andaluz J, Castiella
T and Seral F: Tenosynovial chondromatosis of the third finger.
Arch Orthop Trauma Surg. 120:239–240. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ueo T, Kashima K, Daa T, Kashima N, Tsuji
K, Hisaoka M and Yokoyama S: A case of tenosynovial chondromatosis
with tophus-like deposits. APMIS. 112:624–628. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Chan WL, Hung LK, Griffith JF, Louis TC
and Ho PC: Tenosynovial osteochondromatosis of both flexor and
extensor tendons. Hand Surg. 9:89–95. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Milgram JW: Synovial osteochondromatosis:
A histopathological study of thirty cases. J Bone Joint Surg Am.
59:792–801. 1977.PubMed/NCBI
|
|
6
|
Fetsch JF, Vinh TN, Remotti F, Walker EA,
Murphey MD and Sweet DE: Tenosynovial (extraarticular)
chondromatosis: An analysis of 37 cases of an underrecognized
clinicopathologic entity with a strong predilection for the hands
and feet and a high local recurrence rate. Am J Surg Pathol.
27:1260–1268. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Cebesoy O, Isik M, Subasi M, Karsli B and
Pamukcu U: Extra-articular tenosynovial chondromatosis mimicking a
neoplastic disease in the first web space of the hand. Oman Med J.
27:316–318. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
De Benedetti MJ and Schwinn CP:
Tenosynovial chondromatosis in the hand. J Bone Joint Surg Am.
61:898–903. 1979.PubMed/NCBI
|
|
9
|
Bui Mansfield, Rohini D and Bagg M:
Tenosynovial chondromatosis of the ring finger. AJR Am J
Roentgenol. 184:1223–1224. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ho YY and Choueka J: Synovial
chondromatosis of the upper extremity. J Hand Surg Am. 38:804–810.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Murphey MD, Vidal JA, Fanburg-Smith JC and
Gajewski DA: Imaging of synovial chondromatosis with
radiologic-pathologic correlation. Radiographics. 27:1465–1488.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Christoforou D, Strauss EJ, Abramovici L
and Posner MA: Benign extraosseous cartilage tumours of the hand
and wrist. J Hand Surg Eur Vol. 37:8–13. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Apte SS and Athanasou NA: An
immunohistological study of cartilage and synovium in primary
synovial chondromatosis. J Pathol. 166:277–281. 1992. View Article : Google Scholar : PubMed/NCBI
|