Introduction
Bietti's crystalline dystrophy (BCD), first
described in 1937 (1), is a rare
autosomal recessive disorder characterized by crystal deposition in
the retina and occasionally at the corneal limbus, followed by
retinal degeneration, pigment clumping and choroidal sclerosis
(2). BCD is reported to be a
recessive degenerative eye disease caused by germline mutations in
the CYP4V2 gene (3). BCD is rare in
white populations but relatively common in Asian populations
(3). In particular, the IVS6 to
8delTCATACAGGTCATCGCG/insGC mutation in the CYP4V2 gene is a common
in Japanese patients with BCD (4).
Furthermore, prevalence was 3% of nonsyndromic retinitis pigmentosa
(RP) cases in BCD (5). The corneal
deposits are detected in ~33% of patients, and when corneal changes
are absent the condition is termed Bietti's crystalline retinopathy
(BCR) (6,7).
BCR is characterized by crystal deposition in the
retina, and then retinal degeneration, pigment clumping, and
choroidal sclerosis but without corneal limbus changes (8). It is usually onsets in the third decade
of life (9). Spectral-domain optical
coherence tomography (SD-OCT) showed that most crystalline deposits
in BCR were located adjacent to the inner side of the retinal
pigment epithelium (RPE) layer (10).
In certain cases, choroidal neovascularization (CNV)
is associated with BCR. To the best of our knowledge, there are few
reports investigating the treatment of BCR. Therefore, the present
study reports a novel case of CNV in BCR treated by intravitreal
bevacizumab injection, which has previously been successfully
applied in the treatment of classic CNV in RP (11,12).
Case report
The patient was admitted to First Hospital of China
Medical University (Shenyang, China) on October 1, 2011, with no
prior medical history. Informed consent was obtained from the
patient. A 26-year-old man complained of blurred vision in the
right eye for 2 months, with night blindness in the left and right
eyes since late childhood. The patient's best-corrected visual
acuity (BCVA) was 36/60 in the right eye and 60/60 in the left eye.
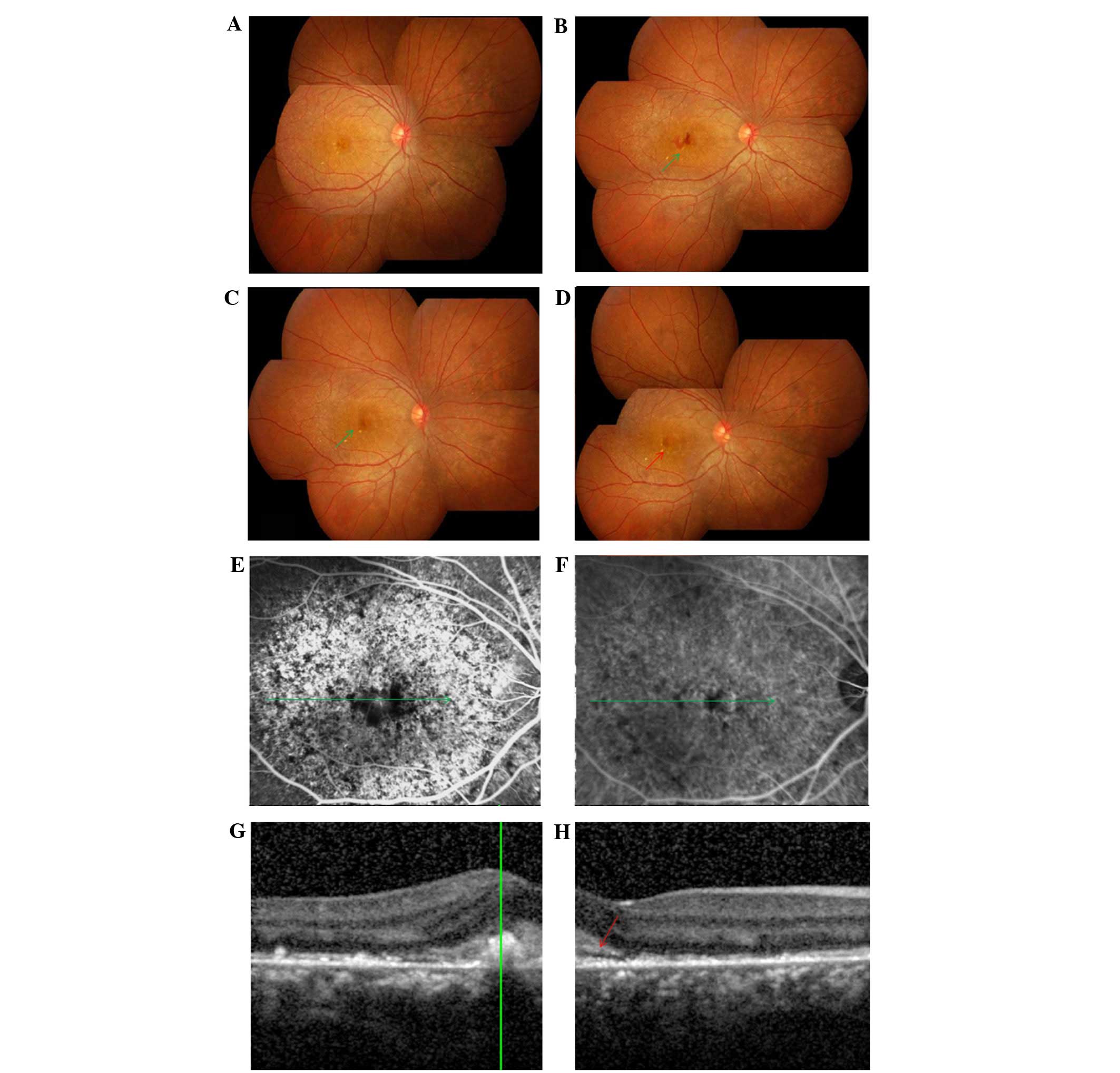
The fundus examination revealed marked, widely distributed,
crystalline degeneration in both eyes, without bony spicules. Six
days after the patient's visit, foveal subretinal hemorrhage
appeared in the right eye (Fig. 1).
The visual field results showed impaired peripheral vision in both
eyes. Afterwards, a diagnosis of BCR was determined based on the
description of BCR characteristics in Chinese patients (8).
Fluorescein angiography (FA) indicated extra
choroidal vessels across the posterior pole. The enhanced
perifoveal hyperfluorescence in FA was diagnosed as CNV, which
corresponded with the spectral domain optical coherence tomography
(SD-OCT) results, whereas it was not clear in indocyanine green
angiography (ICGA) (Fig. 1).
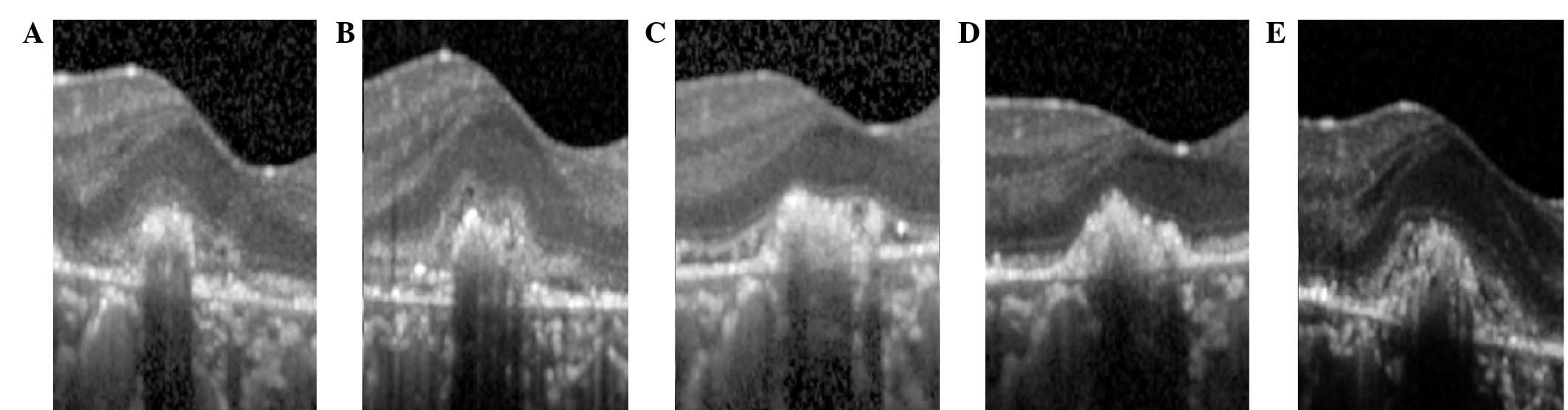
Following diagnosis, bevacizumab was intravitreally injected (1.25
mg/0.05 ml) once. In the first and fourth week after the injection,
it was observed that the foveal hemorrhage had been gradually
absorbed, and the results of SD-OCT examination showed the
regression and stabilization of the CNV. The exudation between the
subretinal space and CNV was absorbed completely. At 3 months after
the injection, however, the CNV reoccurred (Fig. 2), with a BCVA of 48/60 in the right
eye. The patient stopped attending follow-up appointments.
Discussion
The present study investigated multimodality imaging
approaches for analyzing the phenotypes and treatment effects of
anti-vascular endothelial growth factor (VEGF) in CNV secondary to
BCR. It has been reported that visual acuity is relatively good
during the early stages of BCR, with subsequent progressive but
gradual visual loss over decades due to chorioretinal atrophy
(13). Intravitreal injections of
anti-VEGF drugs have recently been considered to be effective in
treating CNV, by improving vision or at least halting its
progressive loss (14).
We believe that the CNV in the present case was a
focal minimal lesion with low activity. This is proposed on the
basis that due to the young age of the patient there was a more
active retinal pigment epithelial (RPE), enveloping the CNV and
promoting its involution (15).
Furthermore, the destruction of the choriocapillaris complex may
have reduced the activity of the subretinal CNV. Fong et al
(16) found that delayed choroidal
filling was observed in all stages of BCR in early ICGA, as well as
a relative derangement of the inner choroidal circulation, as
indicated by late hypofluorescence. Finally and crucially, ICGA
failed to reveal the outline of this CNV, possibly as the large
indocyanine green molecule was not able to flow into the tiny
vessel structure of the lesion. By contrast, due to the lack of RPE
and the smaller fluorescein sodium molecule, FA is able to show a
lesion of this type by enhanced perifoveal abnormal
hyperfluorescence. Similarly, the exudative features of myopic CNV
are more evident when observed using FA (17).
Bevacizumab is a humanized recombinant monoclonal
antibody that is able to bind all VEGF subtypes, with a lower
affinity, longer onset of action and reduced cost compared with
ranibizumab (18). Furthermore,
bevacizumab is more effective than photodynamic therapy (19). It is possible that local, tiny,
low-activity CNVs are insensitive to bevacizumab. Similarly, myopic
CNV with a thinner subfoveal/inferior choroid at baseline may
indicate poor anatomic outcome following intravitreal anti-vascular
endothelial growth factor (VEGF) treatment (20). In addition, there were other factors,
such as onset age and gender, that influence the prognosis. Plafker
et al (21) found that VEGF
production in elderly patients may be reduced compared with younger
patients, and that the aging of RPE cells may lead to impaired
cellular functions including the production of cytokines such as
VEGF. In addition, Wang et al (22) found that males had a higher risk of
recurrence of CNV activity than females. In the present study, the
subretinal CNV relapsed and exudated during the third month after
treatment.
To the best of our knowledge, the present report is
the first from China to describe the clinical characteristics of
CNV in BCR and to report the efficacy of anti-VEGF therapy
according to SD-OCT evaluation. Based on the present results, we
propose that the CNV lesion was a local, tiny, low-activity,
subretinal CNV. The observations in the present case may aid the
treatment of this condition.
References
|
1
|
Gupta B, Parvizi S and Mohamed MD: Bietti
crystalline dystrophy and choroidal neovascularisation. Int
Ophthalmol. 31:59–61. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Mansour AM, Uwaydat SH and Chan CC:
Long-term follow-up in Bietti crystalline dystrophy. Eur J
Ophthalmol. 17:680–682. 2007.PubMed/NCBI
|
|
3
|
Nakano M, Kelly EJ, Wiek C, Hanenberg H
and Rettie AE: CYP4V2 in Bietti's crystalline dystrophy: Ocular
localization, metabolism of ω-3-polyunsaturated fatty acids, and
functional deficit of the p.H331P variant. Mol Pharmacol.
82:679–686. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Wada Y, Itabashi T, Sato H, Kawamura M,
Tada A and Tamai M: Screening for mutations in CYP4V2 gene in
Japanese patients with Bietti's crystalline corneoretinal
dystrophy. Am J Ophthalmol. 139:894–899. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Mataftsi A, Zografos L, Millá E, Secrétan
M and Munier FL: Bietti's crystalline corneoretinal dystrophy: A
cross-sectional study. Retina. 24:416–426. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Jurklies B, Jurklies C, Schimdt U and
Wessing A: Biettis crystalline dystrophy of the retina and cornea.
Retina. 19:168–171. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Welch R: Biettis tapetoretinal
degeneration with marginal corneal dystrophy: Crystalline
retinopathy. Trans Am Ophthalmol Soc. 75:164–179. 1977.PubMed/NCBI
|
|
8
|
Liu DN, Liu Y, Meng XH and Yin ZQ: The
characterization of functional disturbances in Chinese patients
with Bietti's crystalline dystrophy at different fundus stages.
Graefes Arch Clin Exp Ophthalmol. 250:191–200. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Saatci AO, Doruk HC and Yaman A: Cystoid
Macular Edema in Bietti's Crystalline Retinopathy. Case Rep
Ophthalmol Med. 2014:9648922014.PubMed/NCBI
|
|
10
|
Kojima H, Otani A, Ogino K, Nakagawa S,
Makiyama Y, Kurimoto M, Guo C and Yoshimura N: Outer retinal
circular structures in patients with Bietti crystalline
retinopathy. Br J Ophthalmol. 96:390–393. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Malik A, Sood S and Narang S: Successful
treatment of choroidal neovascular membrane in retinitis pigmentosa
with intravitreal bevacizumab. Int Ophthalmol. 30:42–58. 2010.
View Article : Google Scholar
|
|
12
|
Parodi M Battaglia, Iacono P and Bandello
F: Antivascular endothelial growth factor in hereditary
dystrophies. Dev Ophthalmol. 46:107–110. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Bernauer W and Daicker B: Biettis
corneal–retinal dystrophy: A 16-year progression. Retina. 12:18–20.
1992. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Parodi M Battaglia, De Benedetto U,
Knutsson KA, Scotti F, Librando A, Bandello F and Iacono P:
Juxtafoveal choroidal neovascularization associated with retinitis
pigmentosa treated with intravitreal bevacizumab. J Ocul Pharmacol
Ther. 28:202–204. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Glaser BM, Campochiaro PA, Davis JL Jr and
Jerdan JA: Retinal pigment epithelial cells release inhibitors of
neovascularization. Ophthalmology. 94:780–784. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Fong AM, Koh A, Lee K and Ang CL: Bietti's
crystalline dystrophy in Asians: Clinical, angiographic and
electrophysiological characteristics. Int Ophthalmol. 29:459–470.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Leveziel N, Caillaux V, Bastuji-Garin S,
Zmuda M and Souied EH: Angiographic and optical coherence
tomography characteristics of recent myopic choroidal
neovascularization. Am J Ophthalmol. 155:913–919. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Iu LP and Kwok AK: An update of treatment
options for neovascular age-related macular degeneration. Hong Kong
Med J. 13:460–470. 2007.PubMed/NCBI
|
|
19
|
Schouten JS, La Heij EC, Webers CA,
Lundqvist IJ and Hendrikse F: A systematic review on the effect of
bevacizumab in exudative age-related macular degeneration. Graefes
Arch Clin Exp Ophthalmol. 247:1–11. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ahn SJ, Woo SJ, Kim KE and Park KH:
Association between choroidal morphology and anti-vascular
endothelial growth factor treatment outcome in myopic choroidal
neovascularization. Invest Ophthalmol Vis Sci. 54:2115–2122. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Plafker SM, O'Mealey GB and Szweda LI:
Mechanisms for countering oxidative stress and damage in retinal
pigment epithelium. Int Rev Cell Mol Biol. 298:135–177. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Wang H, Barteselli G, Freeman WR, Lee SN,
Chhablani J, El-Emam S and Cheng L: Temporal pattern of
resolution/recurrence of choroidaln neovascularization during
bevacizumab therapy for wet age-related macular degeneration. Int J
Ophthalmol. 6:600–605. 2013.PubMed/NCBI
|