Introduction
Ideberg type III and type IV fractures are unique,
involving the superior glenoid cavity, and the fracture line
commonly extends to the medial area of the coracoids (1). Surgical treatment is usually
recommended for displaced Ideberg type III fractures (2). Three approaches have been reported for
such fractures: Anterior (3,4), posterior (5,6) and
combined (7). Considerable
difficulties are associated with the exposure and fixation of a
glenoid fracture fragment around the scapular notch using these
three traditional approaches due to the acromion. To the best of
our knowledge, the treatment of Ideberg type III glenoid fractures
using an acromial approach has not been reported in the literature.
The present study describes the treatment of two cases of
complicated glenoid fractures using the acromial approach and
presents a review of the literature on the scapular glenoid
fracture.
Case report
Case 1
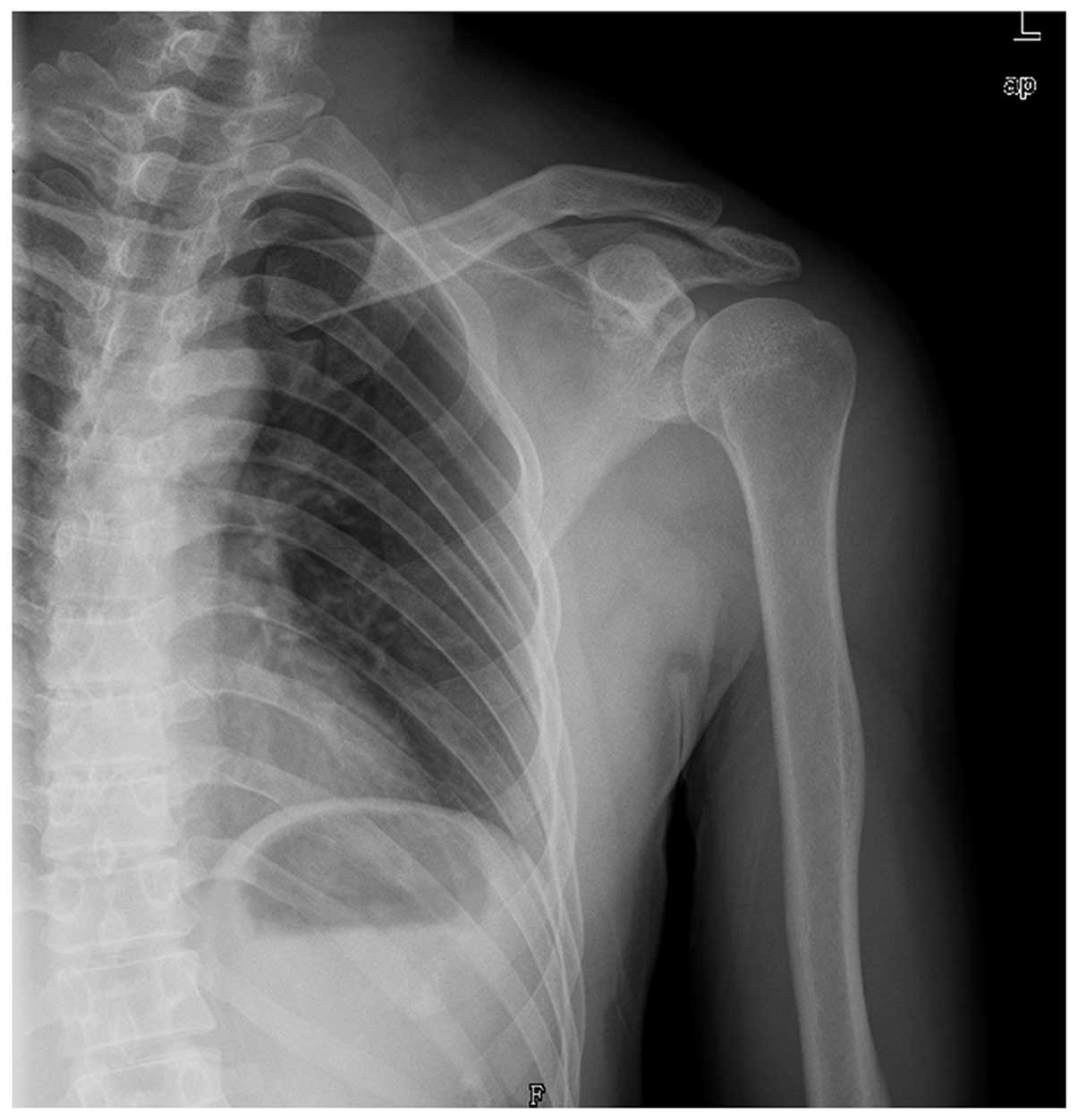
A 30-year-old man complained of pain in the left
shoulder following a direct blow from an object weighing ~100 kg.
Written informed consent was obtained. The plain radiography showed
a glenoid fracture associated with an Ogawa type II acromial
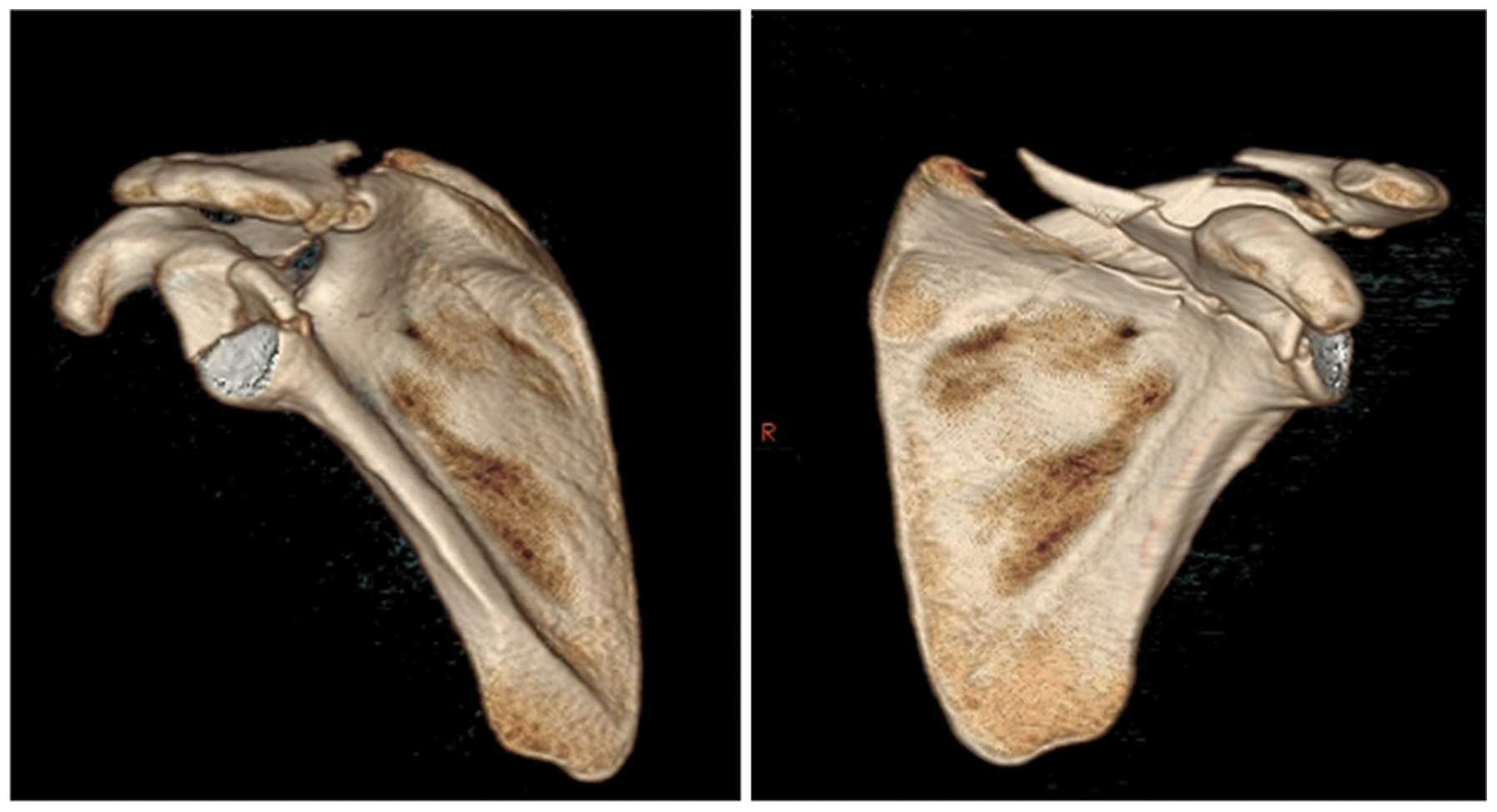
fracture (Fig. 1). Three-dimensional
computed tomography indicated a comminuted glenoid fracture
(Ideberg type III) and a displaced Ogawa type II acromial fracture
(Fig. 2). The comminuted glenoid
fracture consisted of two fragments; the anterior fragment extended
to the medial area of the coracoid, while the posterior fragment
was located around the scapular notch. The patient was admitted to
our department at the Shanghai Pudong Hospital (Shanghai, China)
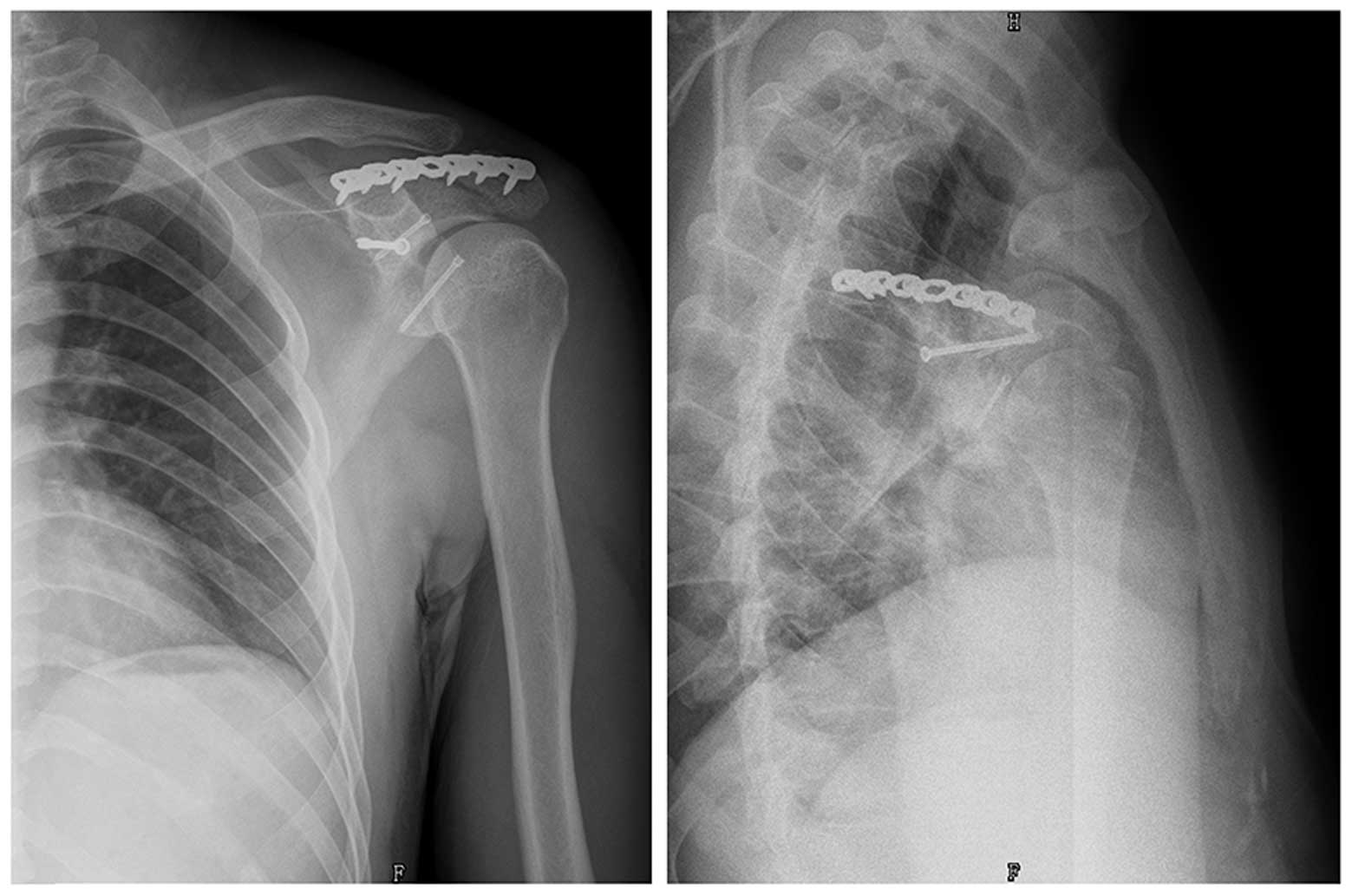
for surgery 3 days after the injury. The glenoid fracture was
addressed first using open reduction via the acromial approach,
pulling the acromial fracture segment and fixing it using three
screws. The acromial fracture was then fixed using a reconstructed
locking plate (Fig. 3).
The patient was followed-up for 13 months. No wound
or axillary nerve complications were noted. Fracture union was
achieved 8 weeks after the surgery. At the final follow-up, the
patient achieved satisfactory shoulder function. The shoulder
abduction, forward flexion and external rotation were 135, 150 and
50°, respectively, which were 25, 15 and 17° less than the
corresponding movement ranges in the contralateral shoulder,
respectively. Internal rotation of the operative and contralateral
shoulders was at thoracic levels T6 and T4, respectively. The
Constant-Murley, University of California, Los Angeles (UCLA)
(8) and Disabilities of Arm,
Shoulder and Hand (DASH) (9) scores
were 84, 32 and 15 points, respectively.
Case 2
A 58-year-old man was injured in a motorbike
accident. Written informed consent was obtained. The patient
suffered a displaced distal clavicular fracture, multiple-rib
fracture and a scapular fracture involving a displaced glenoid
fracture (Ideberg type IV) (Fig.
4).
The patient was transferred to the Department of
Thoracic Surgery at the Shanghai Pudong Hospital. Following open
reduction and fixation of the fractured ribs, the patient was
admitted to our department at the Shanghai Pudong Hospital for
surgery 10 days post-injury. The surgical procedure was similar to
that in case 1. First, the glenoid fracture was addressed using an
open reduction via the acromial approach, pulling the acromial
fracture segment and fixing it using a locking plate. The acromial
and scapular fractures were then fixed using locking plates, prior
to the fixation of the distal clavicular fracture using a locking
plate (Fig. 5).
The patient was followed-up for 13.5 months. There
were no wound or axillary nerve complications. Fracture union was
achieved 9 weeks after the surgery. At the final follow-up, the
patient achieved satisfactory shoulder function. The shoulder
abduction, forward flexion and external rotation were 130, 148 and
55°, respectively, which were 28, 18 and 15° less than the
corresponding movement ranges in the contralateral shoulder,
respectively. Internal rotation of the operative and contralateral
shoulders was at thoracic levels T6.2 and T4, respectively. The
Constant-Murley, UCLA and DASH scores were 81, 29 and 18 points,
respectively.
Surgical techniques
Case 1
The patient was placed in the lateral position with
the affected side up and the forearm was draped free so that it
could be mobilized during the procedure. The position of the
incision was marked, and the incision was performed from the
posterior acromion along the middle length of the scapular spine.
The acromion was readily exposed from its subcutaneous position,
and the deltoid muscle was identified, detached from the posterior
of the scapular spine and retracted inferiorly. The trapezius
muscle was identified, detached from the anterior of the scapular
spine and retracted anteriorly. Following the removal of the
anterior and posterior soft tissue that was adhered to the
acromion, the acromial fracture fragment was raised laterally, the
affected shoulder was abducted 90° and the supraspinatus muscle
tendon was pulled superiorly together with the acromial fragment.
The two glenoid fracture fragments were visualized. First, the
anterior part combined with the coracoids was reduced manually
using clamps and fixed temporarily using K-wire. The posterior part
around the scapular notch was then reduced and fixed using K-wire.
Two screws were used to fix the anterior fracture section and one
for the posterior section. Finally, the acromial fracture was
reduced and readily fixed using a locking plate. It should be noted
that the cut supraspinatus muscle tendon should be sutured
carefully prior to managing the acromial fracture. At the end of
each step, C-arm fluoroscopy was performed to monitor the fracture
reduction and the length of the screws in the standard
anteroposterior and axillary views of the scapula.
Case 2
The patient was positioned as in case 1, again with
the forearm draped free. The position of the incision was marked,
and the incision was performed from the posterior acromion along
the entire length of the scapular spine, curving distally along the
medial border of the scapula and extending proximally to the distal
clavicle. The deltoid muscle was identified, detached from the
posterior of the scapular spine and retracted inferiorly. The
trapezius muscle was identified, detached from the anterior of the
scapular spine and retracted anteriorly. Subsequently, the
infraspinatus was visualized and bluntly separated inferiorly to
access the scapular spine and body fracture fragments. The acromial
basilar fracture line was exposed. Following the removal of the
anterior and posterior soft tissue that was adhered to the acromion
and part of the scapular spine, the acromial fracture fragment was
raised laterally, the affected shoulder was abducted 90° and the
supraspinatus muscle tendon was pulled superiorly together with the
acromial fragment. The glenoid fracture was clearly exposed,
reduced and fixed using a locking plate. The extra-articular
regions of the scapular and distal clavicular fractures were then
monitored, reduced and fixed using a locking plate.
Discussion
Scapular fractures are uncommon injuries, accounting
for 1% of all fractures; 10% of these involve the glenoid cavity
(10). Direct violent trauma is the
normal cause of scapular fractures. A direct violent force applied
laterally to the proximal humerus, which drives the humeral head
into the glenoid fossa, can lead to a glenoid fracture. When the
force of the humeral head is directed slightly superiorly, it can
result in an Ideberg type III and IV glenoid fracture, leading to a
transverse fracture of the fossa that exits along the superior
border of the scapula. When the force is sufficiently large, it
will disrupt the superior shoulder suspensory complex (SSSC),
including the acromion, acromioclavicular joint and distal clavicle
(11).
The indications for surgical treatment include
intra-articular fractures with a >5-mm articular displacement,
step-off and instability (12,13). A
further operative indication for scapular fractures is a double
disruption of the SSSC. The SSSC, which consists of the glenoid,
coracoid, acromion, distal clavicle, coracoclavicular ligaments and
acromioclavicular ligaments, secures the upper extremity to the
axial skeleton (14). While single
disruptions of the SSSC are generally stable, instability can
result when the SSSC is disrupted in two different locations
(double disruption). According to Goss (14), open reduction and internal fixation
(ORIF) are indicated for SSSC double disruptions that are
accompanied by significant displacement, as these may lead to
delayed union, malunion or nonunion, as well as long-term
functional deficits. In a study by Qin et al (11), 9 patients (1 further patient was lost
to follow-up) with Ideberg type III fractures associated with SSSC
injuries were successfully treated for glenoid fractures and SSSC
injuries.
Surgical treatment for the glenoid fracture includes
ORIF and a percutaneous arthroscopy-based procedure. Although the
latter method is minimally invasive and associated with a reduction
in approach-related morbidity, and thus a more rapid return to
function, it is demanding using the current technology. In
particular, correct screw placement remains difficult, and general
experience in the surgical management is limited (15,16).
ORIF is the standard surgical treatment for the glenoid fracture,
even when approach-related complications, including persistent
pain, reduced range of motion and weakened maximum isokinetic
muscle strength, have to be considered (17,18).
Three approaches have been recommended to reduce
glenoid fractures: Anterior (3,4),
posterior (5,6) and combined (7). The anterior approach is the most common
method for the Ideberg type III fracture due to the satisfactory
exposure, including of the intra- and extra-articular components;
however, the disadvantage of this approach is the extensive soft
tissue dissection that is required, including resection of the
subscapularis and its capsule, and the elevation of the
subscapularis from the ventral aspect of the scapular body, which
may affect the internal shoulder rotation. In addition, fractures
around the scapular notch are difficult to expose and fix using the
anterior approach (11).
The posterior approach is frequently used for the
treatment of scapular body, scapular neck and glenoid fractures
with an associated posterior articular component (19). As a result of the positioning of the
acromion, it is impossible to expose and fix the posterior-superior
articular component using the posterior approach.
Currently, there is no anatomical research on a
visible glenoid approach for the reduction and fixation of a
glenoid fracture fragment located around the scapular notch;
therefore, the approach can only be selected based on a surgeon's
experience and understanding of the shoulder anatomy. The basilar
region of the coracoid is located anterior-superior to the glenoid,
and the Ideberg type III fracture line often extends to the medial
area of the coracoid. In addition, the acromion is located upon the
posterior-superior region of the glenoid, and the component around
the scapular notch is deep and therefore difficult to expose and
fix. To the best of our knowledge, there is no relevant anatomical
research on the positional association between the acromion and the
glenoid; therefore, it is difficult to expose and fix an Ideberg
type III and IV fracture with the fragment around the scapular
notch.
Ideberg type III and IV glenoid fractures are often
associated with SSSC injuries, including acromial,
acromioclavicular joint and distal clavicular fractures. These
injuries can be monitored under direct vision using the anterior
approach, extending the incision superiorly; when associated with
acromial fracture, the additional incision would be used,
therefore, additional injuries are created.
In principle, an Ideberg type III and IV fracture
associated with an acromial fracture could be exposed and fixed by
pulling the middle or basilar acromial fragment superiorly and
pushing the supraspinatus muscle tendon. The so-called acromial
approach would require a smaller incision and cause less soft
tissue injury compared with the combined approach.
There is debate as to the existence of a superior
approach, causing less soft tissue injury and with satisfactory
exposure, for the management of an Ideberg type III fracture around
the scapular notch or associated with an acromial fracture. In the
two cases reported in the present study, we believed that the
acromial approach would afford a more visible operating space for
the glenoid around the scapular notch, enable easier exposure and
fixation of the fracture than the anterior approach and produce
less soft tissue injury than the combined approach. Furthermore, it
was considered that raising the supraspinatus muscle tendon instead
of cutting it would cause no significant limitation to the
abduction of the affected shoulder. It should be noted that the
acromial fracture line should be located in the middle of or medial
to the entire acromion. When the line is located around the
extremitas acromialis, the medial region of the acromion can
restrict the exposure and reduction. Management of the
supraspinatus muscle tendon is important, as even partial cutting
of the tendon is likely to lead to a significant limitation in the
abduction. Based on experience, we abducted the affected shoulder
to relax the supraspinatus muscle tendon, allowing the successful
elevation of the tendon to expose the glenoid fracture fragments
around the scapular notch and coracoid.
Surgical treatment of glenoid fractures is
particularly challenging with respect to the exposure of the
fracture. The glenoid fragment around the scapular notch is
extremely difficult to expose due to the acromion. Coincidentally,
the two cases in the present study were both associated with an
acromial fracture; therefore, the supraspinatus muscle tendon was
elevated in each case, satisfactorily exposing the glenoid fracture
fragments around the scapular notch and coracoid. Following
effective functional training, both patients achieved good shoulder
function. In the future, we aim to perform anatomical research on
the exposure of the glenoid fragment and to determine the visible
area of the glenoid fragment using the anterior and posterior
approaches, as well as the acromial approach. The acromial approach
may provide an alternative method for Ideberg type III glenoid
fractures around the scapular notch or associated with an acromial
fracture.
Acknowledgements
This study was funded by the Key Disciplines Group
Construction Project of Pudong Health Bureau of Shanghai (grant no.
PWZxq2014-03).
References
|
1
|
Ideberg R, Grevsten S and Larsson S:
Epidemiology of scapular fractures. Incidence and classification of
338 fractures. Acta Orthop Scand. 66:395–397. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Owens BD and Goss TP: Surgical approaches
for glenoid fractures. Tech Shoulder Elbow Surg. 5:103–115. 2004.
View Article : Google Scholar
|
|
3
|
Cole PA, Gauger EM and Schroder LK:
Management of scapular fractures. J Am Acad Orthop Surg.
20:130–141. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Anavian J, Gauger EM, Schroder LK,
Wijdicks CA and Cole PA: Surgical and functional outcomes after
operative management of complex and displaced intra-articular
glenoid fractures. J Bone Joint Surg Am. 94:645–653. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Schandelmaier P, Blauth M, Schneider C and
Krettek C: Fractures of the glenoid treated by operation. A 5- to
23-year follow-up of 22 cases. J Bone Joint Surg Br. 84:173–177.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Adam FF: Surgical treatment of displaced
fractures of the glenoid cavity. Int Orthop. 26:150–153. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Gramstad GD and Marra G: Treatment of
glenoid fractures. Tech Shoulder Elbow Surg. 3:102–110. 2002.
View Article : Google Scholar
|
|
8
|
Amstutz HC, Hoy AL Sew and Clarke IC: UCLA
anatomic total shoulder arthroplasty. Clin Orthop Relat Res.
155:7–20. 1981.PubMed/NCBI
|
|
9
|
Longo UG, Vasta S, Maffulli N and Denaro
V: Scoring systems for the functional assessment of patients with
rotator cuff pathology. Sports Med Arthrosc. 19:310–320. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zlowodzki M, Bhandari M, Zelle BA, Kregor
PJ and Cole PA: Treatment of scapula fractures: Systematic review
of 520 fractures in 22 case series. J Orthop Trauma. 20:230–233.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Qin H, Hu CZ, Zhang XL, Shen LX, Xue ZC
and An ZQ: Surgical treatment of Ideberg type III glenoid fractures
with associated superior shoulder suspensory complex injury.
Orthopedics. 36:e1244–e1250. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Bauer G, Fleischmann W and Dussler E:
Displaced scapular fractures: Indication and long-term results of
open reduction and internal fixation. Arch Orthop Trauma Surg.
114:215–219. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Soslowsky LJ, Flatow EL, Bigliani LU and
Mow VC: Articular geometry of the glenohumeral joint. Clin Orthop
Relat Res. 181–190. 1992.PubMed/NCBI
|
|
14
|
Goss TP: The scapula: Coracoid, acromial,
and avulsion fractures. Am J Orthop (Belle Mead NJ). 25:106–115.
1996.PubMed/NCBI
|
|
15
|
Yang HB, Wang D and He XJ:
Arthroscopic-assisted reduction and percutaneous cannulated screw
fixation for Ideberg type III glenoid fractures: A minimum 2-year
follow-up of 18 cases. Am J Sports Med. 39:1923–1928. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Gras F, Marintschev I, Aurich M, Rausch S,
Klos K and Hofmann GO: Percutaneous navigated screw fixation of
glenoid fractures. Arch Orthop Trauma Surg. 133:627–633. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Raiss P, Baumann F, Akbar M, Rickert M and
Loew M: Open screw fixation of large anterior glenoid rim
fractures: Mid- and long-term results in 29 patients. Knee Surg
Sports Traumatol Arthrosc. 17:195–203. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Scheibel M, Magosch P, Lichtenberg S and
Habermeyer P: Open reconstruction of anterior glenoid rim
fractures. Knee Surg Sports Traumatol Arthrosc. 12:568–573. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Gauger EM and Cole PA: Surgical technique:
A minimally invasive approach to scapula neck and body fractures.
Clin Orthop Relat Res. 469:3390–3399. 2011. View Article : Google Scholar : PubMed/NCBI
|