Introduction
Cervical cancer is the second most common malignant
tumor in women throughout the world, ranking just behind breast
cancer (1). The essential pathogenic
factor in cervical cancer is the persistence of high-risk human
papillomavirus (HPV), which is a double-stranded DNA virus with a
capsid (2).
To date, numerous studies have reported on the
integration of HPV DNA into the host genome in precancerous uterine
cervical lesions and cervical cancers (3). High-risk HPV DNA integration into the
host genome is a key factor eliciting malignant transformation in
cervical lesions; both the HPV16 integration rate and the
persistence of HPV16 infection demonstrate a positive correlation
with the cervical lesion grade (4).
Although the integration rates of HPV16 and HPV18 DNA increase with
an increase in the malignancy level, the mixed type, that is, cases
in which both free-type and integrated-type infection is present,
is much more frequently observed in HPV16 integration. The
integration of HPV16 and HPV18 into the host genome is an early
step in cervical tumor development, and the incidence rate of HPV
DNA integration increases with the aggravation of cervical lesions
(5). HPV DNA integration has been
detected in 7.4% of lesion tissues in HPV16-positive precancerous
lesions of the uterine cervix, but integration occurs only in
severe cervical lesions (6). These
findings indicate that integration is an essential event in the
progression of cervical lesions.
The Xinjiang Uygur autonomous region of China is an
area with high morbidity from cervical cancer but a low HPV
infection rate. The infection rate with high-risk HPV has been
reported to be as low as 7.25% in women of Uygur ethnicity in
Xinjiang Hotan Prefecture (7–9),
compared with 12.1% in women of Han ethnicity (10). By contrast, the cervical cancer
morbidity rate in women of Uygur ethnicity has been reported to be
as high as 526 per 100,000 (11).
The cause of the high morbidity but low HPV infection rate in Uygur
women is unclear, and the pathogenesis of HPV remains under
investigation. Loss of the E2 gene and viral gene integration into
the host genome elicits the progression of precancerous lesions
from low grade to high grade, which increases the risk of cervical
cancer (3,12,13). It
may be questioned whether viral integration occurs at earlier
stages in lesions in HPV16-infected women of Uygur ethnicity,
whether the probability of integration is higher in Uygur women
than in Han women with the same grade of lesion, and whether DNA
fragments are more likely to break in women of Uygur ethnicity than
in those of Han ethnicity. These questions motivated this
comparative study.
Since the majority of previous studies have focused
on the association of HPV16 integration with the development of
cervical cancer (14–19), in the present study, HPV16-positive
women were included as the subjects. A multiple quantitative
polymerase chain reaction (qPCR) assay was performed to determine
the copy numbers of HPV16 E2 and E6 in cervical cancer tissues and
precancerous lesions. The physical state of the virus indicated by
the E2/E6 ratio was then used to compare the HPV16 DNA integration
rate in different grades of cervical lesions and to explore the
correlation between integration and cervical lesion grade.
Additionally, the HPV16 integration rates in patients of Uygur and
Han ethnicity were compared to explore the role of HPV16
integration in different cervical lesion grades in women of
different ethnicities.
Materials and methods
Patients and specimens
The specimens were biopsy or surgical specimens from
379 women of Uygur ethnicity and 464 women of Han ethnicity with
cervical lesions treated in the Department of Gynecology of the
People's Hospital of Xinjiang Uygur Autonomous Region from August
2010 to March 2011. The specimens were reviewed by two pathologists
with high academic positions. No radiotherapy or chemotherapy was
administered prior to biopsy or surgery. Pregnancy, immunologic
insufficiency and cervical surgical history were the exclusion
criteria. The specimens were stored at −80°C prior to analysis. The
ages of the patients of Uygur ethnicity ranged from 24 to 67 years,
with a mean of 50±12-years. The patients of Han ethnicity ranged in
age from 24 to 81-years, and had a mean age of 46±14-years. The
lesion types of the patients' specimens are presented in Table I.
 | Table I.Lesion types of the specimens from
women of Uygur and Han ethnicity. |
Table I.
Lesion types of the specimens from
women of Uygur and Han ethnicity.
| Ethnicity | Inflammation | CIN I | CIN II | CIN III | Cervical cancer | Total |
|---|
| Uygur | 190 | 96 | 12 | 30 | 51 | 379 |
| Han | 250 | 113 | 14 | 50 | 37 | 464 |
Approval for this study was obtained from the
Institutional Review Board of the People's Hospital of Xinjiang
Uygur Autonomous Region (Xinjiang, China). All participants
provided written informed consent.
According to Wu et al (20), cervical intraepithelial neoplasia
(CIN) is pathologically characterized by cervical dysplasia and
carcinoma in situ with nuclear heterogeneity such as large,
deeply stained nucleus with different sizes and appearance and
maldistributed chromatins. Based on the degrees of cell changes and
the scales of heterotypical cells, the following grades may be
classified: 1, Mild atypical hyperplasia (CINI), in which cells
show a mild degree of heterogeneity in an untidy arrangement but
with polarity and the abnormally proliferated cells are confined to
the lower 1/3 part of the epithelial layer; 2, moderate atypical
hyperplasia (CINII), in which cells show noticeable heteromorphism
in a disordered arrangement and the abnormally proliferated cells
occupy the lower 2/3 part of the epithelial layer; and 3, severe
atypical hyperplasia and carcinoma in situ (CINIII), in
which cells show noticeable heteromorphism without polarity and the
abnormally proliferated cells occupy the lower 2/3 part of the
epithelial layer or even expand to the whole layer. Squamous cell
carcinoma (SCC) refers to the condition in which the moistening
interstitium of the focus exceeds the carcinoma in situ,
showing mesh- or mass-like confluent invasion, and the pathological
characteristics of cervicitis (N) may include cervical polyp,
cervical hypertrophy and Nabothian cysts.
Reagents
The TIANamp Genomic DNA kit for genomic DNA
extraction from blood, cells and tissue (spin column type) was
purchased from Tiangen Biotech (Beijing, China). Primers and probes
for HPV16 E2 and HPV16 E6 were synthesized by Takara Biotechnology
(Dalian, China) and are listed in Table
II. The real-time PCR SuperMix kit, containing Premix Ex Taq™
and ROX reference dye, was purchased from Takara Biotechnology. The
pCR®-XL-TOPO® 3.5 kb HPV16 plasmid and SiHa cell line DNA were
gifts from Xinjiang Key Laboratory of Biological Resources and
Genetic Engineering, Xinjiang University (Xinjiang, China).
 | Table II.Primers and probes for quantitative
polymerase chain reaction. |
Table II.
Primers and probes for quantitative
polymerase chain reaction.
| Amplified
fragments | Primers/probes | Sequence (5′→3′) | Size (bp) |
|---|
| HPV16 E2 (nt
3452–3590) | Forward primer |
GAAACACAGACGACTATCCA | 195 |
|
| Reverse primer |
TCCGTCCTTTGTGTGAGCTGT |
|
|
| Probe |
HEX-CCAAGACAGAGCCAGACAC-Eclipse |
|
| HPV16 E6 (nt
188–382) | Forward primer |
GAATGTGTGTACTGCAAGCA | 132 |
|
| Reverse primer |
GTTGTATTGCTGTTCTAATGTTGT |
|
|
| Probe |
FAM-CAGCATATGGATTCCCATCTC-Eclipse |
|
Extraction of the sample DNA
DNA was extracted from the specimens according to
the instructions provided by the manufacturer of the TIANamp
Genomic DNA kit for genomic DNA extraction from blood, cells and
tissue. Clinicopathological detection was performed with a nucleic
acid spectrophotometer (Beckman DU 700; Beckman Coulter, Inc.,
Brea, CA, USA).
Preparation of standard samples
The copy number was determined using the following
formula: Copy number = weight (g) × 6.23×1023/324.5 × 2
× length of plasmid DNA (where 6.23×1023 represents the
molecular number of 1 mol of substance and 324.5 is the average
molecular weight of a basic group). The copy number of the
pCR®-XL-TOPO® 3.5 kb HPV16 plasmid was determined to be
4.8×1010 copies/µl, and the plasmid was then stored at
−20°C. When adding the samples to the PCR mixes, the concentration
of the plasmid was diluted to 4.8×1010,
4.8×109, 4.8×108, 4.8×107,
4.8×106, 4.8×105, 4.8×104 and
4.8×103 copies/µl to serve as standard samples.
Determination of the E2 and E6 copy
number through multiple qPCR
The mixes for qPCR were prepared with the following
reagents (total volume, 30 µl): 15 µl ddH2O, 9 µl Premix
Ex Taq™ (2X), 0.6 µl ROX reference dye (50X), 0.6 µl
HPV16 E2 forward primer (10 µM), 0.6 µl HPV16 E2 reverse primer (10
μM), 0.6 µl HPV16 E6 forward primer (10 µM), 0.6 µl HPV16 E6
reverse primer (10 µM), 0.5 µl HPV16E2 Taq Man probe (20 μM), 0.5
µl HPV16E6 Taq Man probe (20 µM), and 2 µl template DNA. The
concentration of each standard DNA sample was measured three times,
and the concentrations of the specimen DNA samples were measured
twice. DNA extracted from SiHa cells was used as the negative
sample control, the prepared standard sample of 4.8×107
copies/µl was used as the positive system control, and a DNA blank
was used as the negative system control. The PCR amplification was
performed in an ABI 7500 Real-Time PCR system (Applied Biosystems
Life Technologies, Foster City, CA, USA) with the following
reaction conditions: Initial denaturation at 95°C for 30 sec
followed by PCR at 95°C for 5 sec, 58°C for 34 sec, and 72°C for 30
sec (for 40 cycles).
Statistical analysis
Samples with HPV16 E6 copy numbers >0 were
considered HPV16 positive. The numbers of cases with cervical
lesions in the different populations were expressed as an absolute
number and percentages, and the HPV16 integration rates were
expressed as the mean ± standard deviation. The data were processed
using SPSS software, version 17.0 (SPSS, Inc., Chicago, IL, USA).
The HPV16-positive rates of the different populations were compared
using the χ2 test, the HPV16 integration states in the
various cervical lesion grades of the different populations were
compared with the Kruskal-Wallis H test, and the integration states
and integration ratios within the same cervical lesion grade in the
different populations were compared using the Wilcoxon test.
Differences of P<0.05 were considered statistically significant,
with a test power of 0.8.
Results
Clinicopathological information
regarding HPV16-positive patients
Detection with a nucleic acid spectrophotometer
indicated that the extracted DNA had a concentration >150 ng/µl.
The results from the double PCR detection of HPV16 DNA in the
patients are listed in Table III.
The Uygur group and the Han group did not show any differences in
the grades of the cervical lesions.
 | Table III.Case population and rate of
HPV16-positive cervical lesions according to lesion type in women
of Uygur and Han ethnicity [n, (%)]. |
Table III.
Case population and rate of
HPV16-positive cervical lesions according to lesion type in women
of Uygur and Han ethnicity [n, (%)].
| Ethnicity | Inflammation | CIN I | CIN II | CIN III | Cervical cancer | Total |
|---|
| Uygur | 20 (10.5) | 32 (33.3) | 6 (50.0) | 20 (66.7) | 44 (86.3) | 122 |
| Han | 22 (8.8) | 34 (30.1) | 7 (50.0) | 28 (56.0) | 30 (81.1) | 121 |
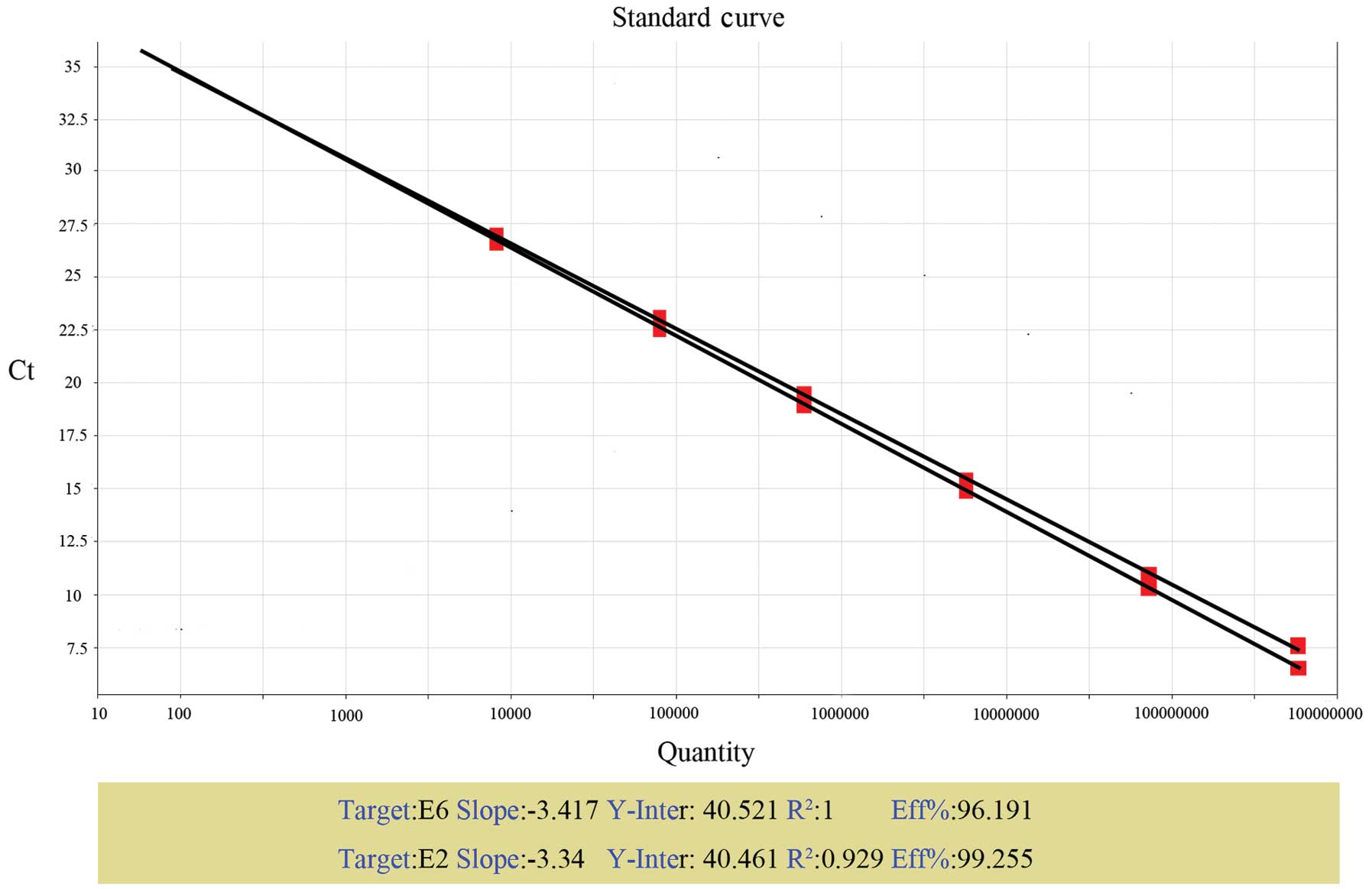
Standard curves
Standard curves were established based on the
multiple qPCR data for E2 and E6 in the standard samples (Fig. 1). The equations used to establish the
standard curves for E2 and E6 were: Ct = −3.34logX0 +
40.461 and Ct = −3.417logX0 + 40.521, where
X0 is the original copy number and Ct represents the
cycle threshold reflecting the number of cycles required for the
fluorescence intensity in the tube to reach the designated
threshold. Based on the Ct values for each tube, the E2 and E6 copy
numbers were calculated, and 20 E2/E6 ratios were obtained. Of
note, the E6 gene was not detected in one low-concentration
standard sample. The 95% confidence interval for the 20 E2/E6
ratios was calculated to be 0.81–1.20. The critical value of 0.81
was confirmed as the demarcation between HPV16 free-type infections
and integrated-type infections. Specifically, E2/E6=0 indicated an
integrated-type infection, E2/E6>0.81 indicated a free-type
infection, and 0<E2/E6<0.81 indicated a mixed-type infection
(both free-type and integrated-type).
HPV16 integration rates in different
grades of cervical lesions
The HPV16 integration ratios in cervical lesions of
different grades were detected. In the positive system control, the
ratio of E2/E6 was 0.96. E2 and E6 were not detected in the
negative system control. In the negative sample control, the ratio
of E2/E6 was 0. The integration state of HPV16 in the patients of
Uygur and Han ethnicity is shown according to lesion grade (N, CIN
I, CIN II/III or SCC) in Table IV.
According to the Kruskal-Wallis H test for multi-sample
comparisons, the type distribution within the same population
showed a significant difference (P<0.05); specifically, as the
lesion grade increased, the proportion of free-type HPV16
infections decreased, and the proportion of integrated-type
infections increased. Between the Uygur and Han populations, the
proportions of integration showed no significant differences within
the same cervical lesion grade (P>0.05).
 | Table IV.Comparison of the integration states
of HPV16 [n, (%)]. |
Table IV.
Comparison of the integration states
of HPV16 [n, (%)].
|
| Uygur (n=122) | Han (n=121) |
|
|
|---|
|
|
|
|
|
|
|---|
| Lesion grade | Free | Mixed | Integrated | Free | Mixed | Integrated | Za | P-value |
|---|
| N | 16 (13.11) | 4 (3.28) | 0 (0) | 15 (12.40) | 7 (5.79) | 0 (0) | −0.86 | 0.39 |
| CIN I | 19 (15.57) | 13 (10.66) | 0 (0) | 17 (14.05) | 17 (14.05) | 0 (0) | −0.76 | 0.45 |
| CIN II/III | 8 (6.56) | 17 (13.93) |
1 (0.82) | 9 (7.44) | 25 (20.66) |
1 (0.83) | −0.34 | 0.73 |
| SCC | 9 (7.36) | 32 (26.23) |
3 (2.46) | 7 (5.79) | 21 (17.36) |
2 (1.65) | −0.26 | 0.80 |
| χ2b |
| 26.18 |
|
| 16.14 |
|
|
|
| P-value |
| 0.00 |
|
| 0.00 |
|
|
|
HPV16 integration rates within
different cervical lesion grades in patients of Uygur and Han
ethnicities
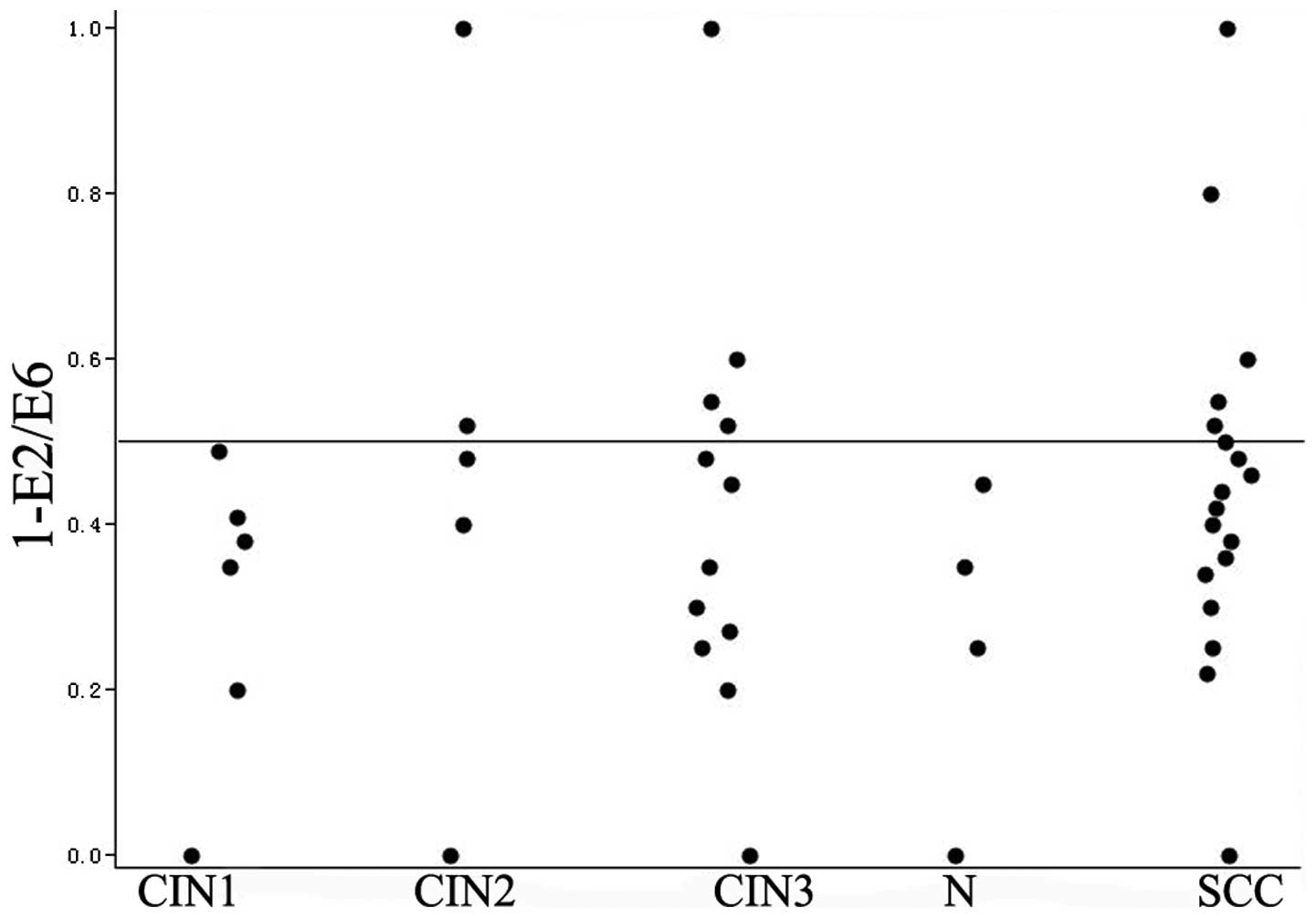
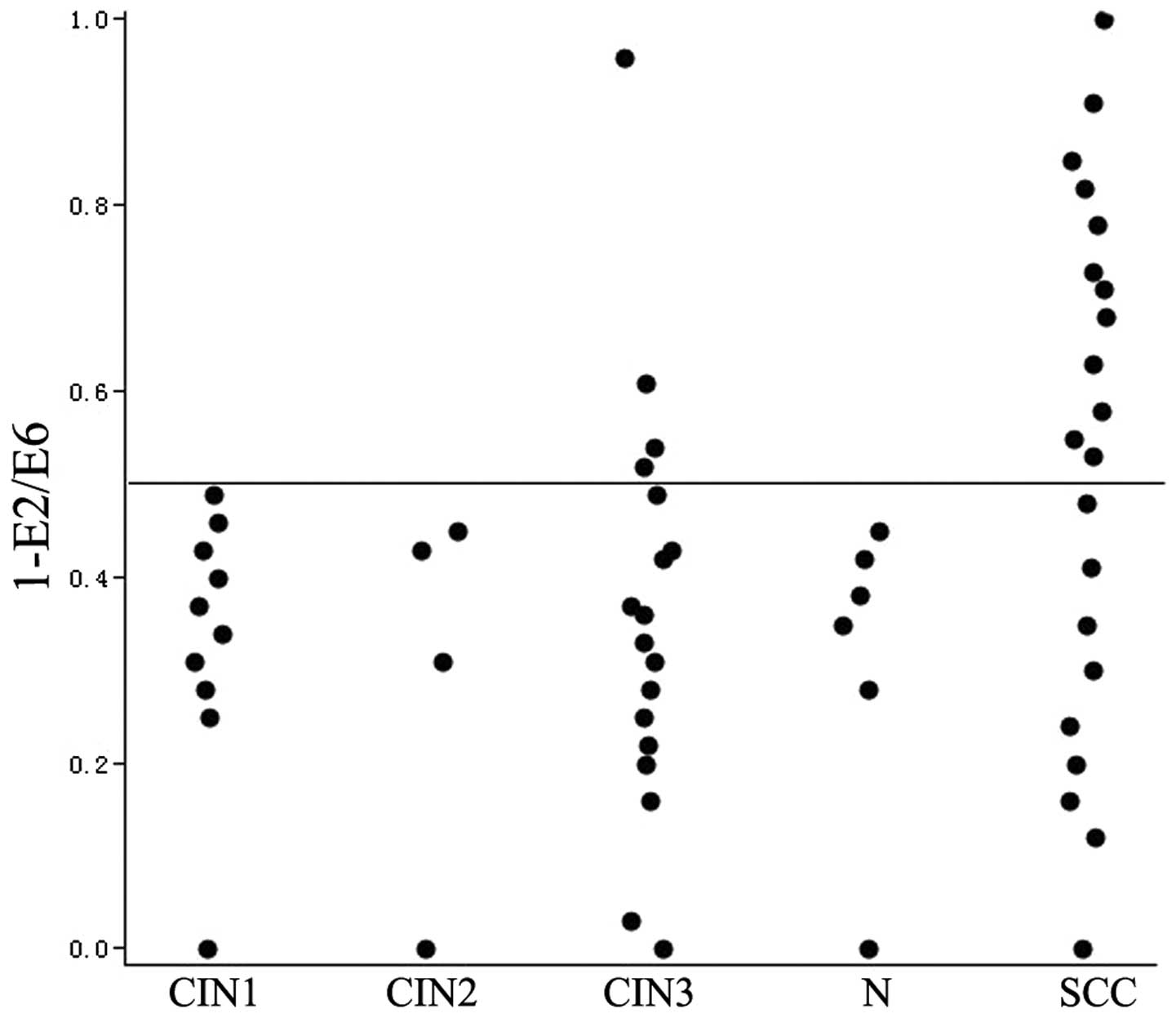
The integration rate was defined as 1-E2/E6. The
HPV16 integration rates for the lesions of grades N, CIN I, CIN II,
CIN III and SCC are shown in Figs. 2
and 3. In the Uygur patients with
lesion grades N and CIN I and in the Han patients with lesion
grades N, CIN I and CIN II, the integration rates were <0.5. In
the lesions of grades N, CIN I, CIN II, CIN III and SCC in patients
of either Uygur or Han ethnicity, the integration rate of HPV16
appeared to increase as the grade of the cervical lesions
increased; however, the increase was not found to be statistically
significant according to the Kruskal-Wallis H test (Uygur:
χ2=2.44, P=0.30; Han: χ2=4.12, P=0.13).
Between the Uygur and Han patients, there was no
significant difference in the HPV16 integration rate within the
same grade of lesion (Wilcoxon test of 2 independent samples,
P>0.05; Table V). Irrespective of
the differences between the two populations, the Uygur and Han
patients were considered as one sample to increase the sample size.
As the grade of the lesions increased from N to CIN I, CIN II/III
and SCC, the integration rate increased gradually, and the increase
was statistically significant (Kruskal-Wallis H,
χ2=8.42, P=0.02).
 | Table V.Comparison of the HPV16 integration
rates between the patients of Uygur and Han ethnicity with the same
cervical lesion grades (mean ± standard deviation). |
Table V.
Comparison of the HPV16 integration
rates between the patients of Uygur and Han ethnicity with the same
cervical lesion grades (mean ± standard deviation).
| Grade | Uygur | Han | Za | P-value |
|---|
| N | 0.16±0.12 | 0.13±0.10 | −0.57 | 0.60 |
| CIN I | 0.27±0.18 | 0.23±0.15 | −0.54 | 0.59 |
| CIN II/III | 0.38±0.26 | 0.32±0.22 | −0.58 | 0.56 |
| SCC | 0.41±0.24 | 0.51±0.30 | −0.56 | 0.58 |
Discussion
In this study, the proportion of integration within
the same cervical lesion grade demonstrated no statistically
significant difference between Uygur and Han ethnicities. Even in
the group of patients with CIN II/III grade lesions, the
integration ratio in the women of Han ethnicity appeared to be
higher than that in the women of Uygur ethnicity. Neither of these
findings is able to account for the high morbidity but low HPV
infection rate observed in the Xinjiang Uygur population. Based on
the results of this study, there are four potential explanations.
First, E2 contains an N terminus, C terminus and hinge region. In
the study by Zhang et al, the miss rates for the N terminus,
hinge region and C terminus were 71.88, 50.00 and 21.88%,
respectively (21). It may be
possible that frequent fractures occur outside of the hinge region
in women of Uygur and Han ethnicity in Xinjiang. This possibility
is dependent on the complete detection and analysis of the fracture
sites of E2, and even of E1, to identify whether actual differences
in HPV16 integration rates exist between Uygur and Han women.
Second, the small sample size limited the detection accuracy; thus,
increasing the sample size might improve the detection power in
further studies. Third, no consensus has been reached regarding the
pathogenesis of HPV16 integration into the host genome during
cervical cancer development. Among patients with CIN I, CIN II/III
and SCC from France, the HPV16 integration rates were 64, 83.3 and
82%, respectively. Although the integration rate increased as the
grade of the lesion increased, this change was not statistically
significant, which might be attributable to the small sample size
(22). Another previous study of CIN
and cervical cancer cases revealed that the average HPV16
integration rate was 68%, and the researchers concluded that HPV16
integration is not an essential pathogenic factor in the
development of cervical cancer (23). In addition, a previous study
demonstrated different proportions of HPV16 integration within the
same cervical lesion grade from different areas in the world
(20). Finally, in women with
cervical cancer, multiple infections occur more often in Uygur
women than in Han women. As a carcinogenic mechanism, multiple
infections might facilitate amplification of the telomerase RNA
component (TERC) gene, resulting in the higher morbidity of
cervical cancer in Uygur women than in Han women (24). Certainly, certain customs and
conditions of the Uygur population, including early marriage, early
pregnancy, multiple births, poor health habits, inconvenient
transportation, insufficient medical facilities and lack of a
cervical cancer screening system, may also substantially contribute
to the high morbidity of cervical cancer.
The proportion of HPV16 integration can provide a
cross-sectional perspective of the integration incidence in a
population and might reflect the difficulty of integration in
different cervical lesion grades. The integration rate can also
provide a longitudinal perspective of integration and may indicate
the intensity of viral integration in individuals. This latter
aspect might be beneficial for disease assessments of individual
patients (25) and could trigger
shunting effects that affect the prognosis of HPV-positive CIN II
cases (26). The results of the
present study demonstrate different degrees of HPV16 integration
between different grades of CIN and cervical cancer in the study
population. In the N, CIN I, CIN II/III and SCC groups, the
proportion of free HPV16 decreased as the lesion grade increased,
but the proportion of integration (mixed- and fractured-type)
increased gradually. The integrated type was found in CIN II/III
and SCC lesions, and the percentage of the integrated type was
highest in SCC. Specifically, as the grade of the cervical lesion
increased, a larger rate of HPV16 integration was observed, which
revealed that HPV16 integration into the host genome is a key
pathogenic factor in cervical cancer. This finding is consistent
with studies of women of Han ethnicity in Sichuan and Hubei
conducted by Zheng et al (27), Shi et al (28) and Li et al (29).
The mean integration rates in the N, CIN I, CIN
II/III and SCC groups demonstrated no statistically significant
differences between the Uygur and Han patients. When the
differences between the populations were ignored and the Uygur and
Han women were considered as one sample, it was found that the
integration rate increased as the lesion grade increased from N to
CIN I, CIN II/III and SCC to a statistically significant degree.
This finding indicates that an increased sample size might help to
elucidate the association between viral integration and the
progression of cervical lesions. Once the association between
increasing viral integration and cervical lesion progression is
established, the comparison between Uygur and Han ethnicities will
become significant.
A previous study detected HPV16 in cases graded as
N, CIN I, CIN II/III and SCC with median HPV16 E2/E6 ratios of
0.75, 0.58, 0.51 and 0.36, respectively. The ratio tended to
decrease with increasing cervical lesion grade (22). That investigation revealed that viral
loads >22,000 copies/1,000 cells and yielding an E2/E6 ratio
<0.5 tend to progress into higher grade lesions. This finding
may guide further studies concerning the integration rate in Han
women using larger sample populations.
In conclusion, HPV16 integration was found to be an
essential factor contributing to the progression of cervical
lesions in women of Uygur and Han ethnicity, and no differences in
HPV integration were observed between the two populations. In
addition, no correlation was observed between the integration rate
and the progression of the cervical lesion grade. In further
studies, larger sample sizes and more sensitive detection methods
are required to explore the objective pathogenesis of the high
cervical cancer morbidity in women of Uygur ethnicity.
Acknowledgements
The authors thank the staff of the Department of
Gynecology of Xinjiang Uygur Autonomous Region People's Hospital
for assistance during the study. This study was supported by the
National Natural Science Foundation of China (grant no.
81160317).
References
|
1
|
Cornelison TL: Humanpapillomavirus
genotype 16 vaccine for cervical cancer prophylaxis and treatment.
Cirr Opin Oncol. 12:466–473. 2000. View Article : Google Scholar
|
|
2
|
Muñoz N, Bosch FX, de Sanjosé S, Herrero
R, Castellsagué X, Shah KV, Snijders PJ and Meijer CJ:
International Agency for Research on Cancer Multicenter Cervical
Cancer Study Group: Epidemiologic classification of human
papillomavirus types associated with cervical cancer. N Engl J Med.
348:518–527. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Pett M and Coleman N: Integration of
high-risk human papillomavirus: A key event in cervical
carcinogenesis? J Pathol. 212:356–367. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Jiang SQ, Tu SA, Zhou JL, Mai M, Bi J, Ru
X, Sha L, Xu X, Hai R and Ai M: Investigation and analysis of
gynecopathy in Cele county of Xinjiang, China. Zhongguo Fu You Bao
Jian. 21:524–526. 2006.(In Chinese).
|
|
5
|
Li N and Dai M: Human papillomavirus in
China: A multiple-centric cross sectional study. Zhonghua Ji Bing
Kong Zhi Za Zhi. 12:411–415. 2008.(In Chinese).
|
|
6
|
Li L, Pan Q, Liu XF, Wu YP, Qiao YL, Ma Y,
Chen F, Zhu K, Liu XW, RE Z, et al: A cross-sectional study: The
prevalence and distribution characteristic of HPV infection in
Uygur women in Xinjiang. Ai Zheng Jin Zhan. 2:114–118. 2010.(In
Chinese).
|
|
7
|
Li J, Li LK, Ma JF, Wei LH, Niyazi M, Li
CQ, Xu AD, Wang JB, Liang H, Belinson J and Qiao YL: Knowledge and
attitudes about human papillomavirus (HPV) and HPV vaccines among
women living in metropolitan and rural regions of China. Vaccine.
27:1210–1215. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Cricca M, Venturoli S, Leo E, Costa S,
Musiani M and Zerbini M: Disruption of HPV 16 E1 and E2 genes in
precancerous cervical lesions. J Virol Methods. 158:180–183. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Li W, Wang W, Si M, Han L, Gao Q, Luo A,
Li Y, Lu Y, Wang S and Ma D: The physical state of HPV16 infection
and its clinical significance in cancer precursor lesion and
cervical carcinoma. J Cancer Res Clin Oncol. 134:1355–1361. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Huang LW, Chao SL and Lee BH: Integration
of human papillomavirus type-16 and type-18 is a very early event
in cervical carcinogenesis. J Clin Pathol. 61:627–631. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Matovina M, Sabol I, Grubisić G, Gasperov
NM and Grce M: Identification of human papillomavirus type 16
integration sites in high-grade precancerous cervical lesions.
Gynecol Oncol. 113:120–127. 2007. View Article : Google Scholar
|
|
12
|
Tinelli A, Vergara D, Leo G, Malvasi A,
Casciaro S, Leo E, Montinari MR, Maffia M, Marsigliante S and
Lorusso V: Human papillomavirus genital infection in modern
gynecology: Genetic and genomic aspects. Eur Clinics Obst Gynaecol.
3:1–6. 2007. View Article : Google Scholar
|
|
13
|
Arias-Pulido H, Peyton CL, Joste NE,
Vargas H and Wheeler CM: Human papillomavirus type 16 integration
in cervical carcinoma in situ and in invasive cervical cancer. J
Clin Microbiol. 44:1755–1762. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Bosch FX, Manos MM, Muñoz N, Sherman M,
Jansen AM, Peto J, Schiffman MH, Moreno V, Kurman R and Shah KV:
International Biological Study on Cervical Cancer (IBSCC) Study
Group: Prevalence of human papillomavirus in cervical cancer: A
worldwide perspective. J Natl Cancer Inst. 87:796–802. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Pirami L, Giache V and Becciolini A:
Analysis of HPV 16, 18, 31 and 35 DNA in pre-invasive and invasive
lesions of the uterine cervix. J Clin Pathol. 50:600–604. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kalantari M, Blennow E, Hagmar B and
Johansson B: Physical state of HPV16 and chromosomal mapping of the
integrated form in cervical carcinomas. Diagn Mol Pathol. 10:46–54.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kristiansen E, Jenkins A and Holm R:
Coexistence of episomal and integrated HPV16 DNA in squamous cell
carcinoma of the cervix. J Clin Pathol. 47:253–256. 1994.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Park JS, Hwang ES, Park SN, Ahn HK, Um SJ,
Kim CJ, Kim SJ and Namkoong SE: Physical status and expression of
HPV genes in cervical cancers. Gynecol Oncol. 65:121–129. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Dürst M, Kleinheinz A, Hotz M and Gissmann
L: The physical state of human papillomavirus type 16 DNA in benign
and malignant genital tumours. J Gen Virol. 66:1515–1522. 1985.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Wu XX, Niyazi M, Zhu KC, et al: Status of
HPV16 infection in cervical lesions in Uygur women and its clinical
significance. Zhong Guo Zhong Liu. 21:394–397. 2012.(In
Chinese).
|
|
21
|
Zhang S, Cai HB and Ding XH: Different
deletion states of HPV16 E2 gene in C-terminal hinge region and
N-terminal in cervical lesions. Xiandai Fuchanke Jinzhan.
19:728–731. 2010.(In Chinese).
|
|
22
|
Saunier M, Monnier-Benoit S, Mauny F,
Dalstein V, Briolat J, Riethmuller D, Kantelip B, Schwarz E, Mougin
C and Prétet JL: Analysis of human papillomavirus type 16 (HPV16)
DNA load and physical state for identification of hpv16-infected
women with high-grade lesions or cervical carcinoma. J Clin
Microbiol. 11:3678–3685. 2008. View Article : Google Scholar
|
|
23
|
Sathish N, Abraham P, Sridharan G, Shaji
RV, Chandy G and Peedicayil A: E2 sequence variations of HPV 16
among patients with cervical neoplasia seen in the Indian
subcontinent. Gynecol Oncol. 95:363–369. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Liu KJ, Liu Q and Tang HF: Study on
genotypes of human papilloma virus infected Uigur and Han women
with cervical cancer and their relationships with TERC gene
amplification. Zhongguo Fuchanke Linchuang Zazhi. 6:449–452.
2008.(In Chinese).
|
|
25
|
Li HH: The study on the corralation
between cervical cancer and HPV DNA integration, E2 disruption,
ratio of HPV E2/E6. Zhongguo Mian Yi Xue Za Zhi. 26:670–673.
2010.(In Chinese).
|
|
26
|
Li Li, Mayinuer Niyazi, Wenhua Zhang, et
al: A cross-section population study on different cervical cancer
screening methods in uygur women of xinjiang. Zhongguo Zhongliu.
19:238–242. 2010.(In Chinese).
|
|
27
|
Zheng Y, Peng ZL, Lou JY and Wang H:
Detection of HPV16 integration status in preinvasive and invasive
cervical carcinoma. Zhongguo Kang Ai Xie Hui. 33:961–964. 2006.(In
Chinese).
|
|
28
|
Shi YM, Ye H, Xiao CY, Chen JL, Wang YQ
and Wu JF: Change and significance of HPV integrated state in
cervical lesions. Shandong Yi Yao. 49:1–3. 2009.
|
|
29
|
Li KZ, Jin Z, Fang Y, Ai JH, et al: Study
on the correlation between integrated state of HPV-16 and the
occurrence of cervical cancer. Zhongguo Fu You Bao Jian.
26:4241–4244. 2011.(In Chinese).
|