Introduction
Local body tissues subjected to long-term pressure
receive restricted blood flow and exhibit nutrient deficiency and
the loss of normal functions, which may lead to tissue ulceration
and necrosis, i.e. pressure ulcers (PUs) (1,2). PUs are
a commonly observed complication in long-term bedridden patients
suffering from a range of diseases, including coma, quadriplegia,
senility and weakness, traumatic fixation and severe malnutrition
(3,4). A number of methods have been used to
promote wound healing in PUs, with the primary method being the
local application of drugs. Drugs based on Traditional Chinese
Medicine, Western medicine and a combination of Chinese and Western
medicine have been employed for the treatment of PUs (5,6).
Recently, with the development of stem cell technology, treatments
aimed at various refractory diseases have additionally been
developed (7–9). Human amniotic epithelial cells (hAECs)
express embryonic stem cell markers, such as stage-specific
embryonic antigen 3 (SSEA-3), SSEA-4, TRA-1-81, fibroblast growth
factor 4 and Rex1d, in addition to pluripotent cell transcription
factors, such as octamer-binding transcription factor 4 (Oct-4) and
Nanog. hAECs may be induced to differentiate into cells of the
three germinal layers in vivo and in vitro, and thus
may be used as an experimental substitute for embryonic stem cells
(10–12). In the present study, Sprague Dawley
rats were used to establish a model to observe the effects of hAECT
in treating stage III PU. Wound tissue samples were extracted at
different time-points to detect the anti-inflammatory and tissue
growth-promoting effects of the cells and to determine the
expression of vascular growth-related factors. The aim of the study
was to analyze the possible mechanisms underlying the effects of
hAECs and to provide a basis for future preclinical studies using
hAECs to treat stage III refractory PU.
Materials and methods
Acquisition of human amnion
hAECs for transplantation into rats were obtained
from the placenta of parturient women recruited from the Department
of Obstetrics of the Affiliated Hospital of Zunyi Medical College
(Zunyi, China). Informed consent was obtained from all patients.
The amniotic membrane was peeled from the fresh placenta of each
parturient patient that underwent a full-term C-section. Patients
were excluded if they exhibited such diseases as hepatitis B,
hepatitis C, syphilis and HIV.
Culture and identification
The amniotic membrane was peeled from the fresh
placenta under aseptic conditions. After being washed with freshly
prepared D-Hank's solution (Sigma-Aldrich, St. Louis, MO, USA), the
amniotic membrane was cut into 2×2-cm pieces and digested in 0.02%
EDTA-containing 0.05% trypsin solution (Fuzhou Maixin Biotechnology
Development, Co., Ltd., Fuzhou, China), and 10% fetal bovine serum
(FBS) (Fuzhou Maixin Biotechnology Development, Co., Ltd.) was used
to terminate the digestion. The cell precipitate, comprising the
primary hAECs, was resuspended in low-glucose Dulbecco's modified
Eagle's medium containing 1% β-mercaptoethanol, 1% GlutaMAX™, 10%
FBS, 10 ng/ml epidermal growth factor and 1% non-essential amino
acid (all reagents supplied by Hyclone Laboratories, Inc., Logan,
UT, USA). The separated primary cells were seeded into a
25-cm2 culture flask at a density of 5×105
cells/ml. After 72–96 h, when the cell confluence was >80%,
0.125% trypsin and 0.02% EDTA solution was used for the digestion,
subculture and identification.
Flow cytometric analysis and
immunocytochemical staining were performed to identify the
hAECs
The 3–4 generations of hAMSCs were collected, and
the cell density was adjusted to 2×105 cells/ml. Then,
200 µl cell suspension was taken, and 10 µl monoclonal CD44-PE
(cat. no. 550989), CD90-FITC (cat. no. 555595), CD105-PerCP-Cv5.5
(cat. no. 560839), CD73-APC (cat. no. 560847), CD34-PE (cat. no.
555822), CD45-PE (cat. no. 555483), CD11b-PE (cat. no. 555388),
CD19-PE (cat. no. 55413) and CDDR-PE (cat. no. 559868) antibodies
(Shanghai Sangon Biological Engineering Technology and Services
Co., Ltd., Shanghai, China) were added, respectively, followed by
incubation at room temperature for 25 min. Next, 2 ml
phosphate-buffered saline (PBS) containing 1 g/l NaN
(Sigma-Aldrich) was added to each tube. After mixing, the mixture
was centrifuge at 168 × g for 5 min and the supernatant was
discarded. Following a further oscillation, the cells were
suspended in PBS. Subsequently, 200 µl 4% paraformaldehyde
(Sigma-Aldrich) was added to each tube. The mixture was detected
using a FACSCanto II flow cytometry cell analyzer (BD Biosciences,
Franklin Lakes, NJ, USA), and the data were analyzed using Cell
Quest software (BD Biosciences).
Preparation of animal model and
grouping
A total of 96 adult male Sprague Dawley rats,
weighing 120–150 g, were purchased from Chongqing Tengxin Bill
Experimental Animals Sales Co., Ltd. [license no. SCXK (Yu)
2012-0005; Chongqing, China]. Model preparation was performed in
accordance with the method in China patent no. ZL201420090436X
(13). The rats were separated into
the model, conventional treatment, hAECT and control groups (n=24
per group). In the model group, each rat was fitted with a medical
sterile applicator (Shanghai Precision Scientific Instruments Co.,
Ltd., Shanghai, China) to protect the wound following surgery,
which was changed daily. In the conventional treatment group, the
wounds were disinfected with 0.5% povidone-iodine and then exposed
to infrared light for 15–20 min, once per day, and covered with
0.5% povidone-iodine solution, with the gauze saturated with
solution but not dripping. A medical sterile applicator was used to
fix the iodine gauze after the disinfection. Each of the steps,
including disinfection, infrared-light irradiation and
povidone-iodine gauze redressing, was performed daily under sterile
conditions. In the hAECT group, each rat was immediately
subcutaneously injected with hAEC (passage 4/5) single-cell
suspension. The cell density was adjusted to 1×106/ml
with D-PBS. The wound was divided into 8 parts, and 8 points were
selected from the center and edges of the wound; 0.03 ml cell
suspension was injected into each transplantation point. In the
normal control group, the rats had their leg hair shaved and were
fixed on the operating table under anesthetic (1/100 g Propofol;
Sigma-Aldrich), in a similar manner to the rats in the other
groups, but did not undergo modeling or treatment. This study was
conducted with approval from the Animal Ethics Committee of Zunyi
Medical College (Zunyi, China).
Determination of survival status of
hAECs
The survival status of hAECs in rat skin tissue was
determined using an immunofluorescence staining method. The tissue
sections were washed with PBS three times, for 5 min per time. Then
the specimens were treated with 0.3% Triton-X100 (Sigma-Aldrich)
for 15 min, followed by blocking using 10% normal goat serum
(Fuzhou Maixin Biotechnology Development Co., Ltd.) for 30 min. A
primary monoclonal mouse anti-human nucleus-specific antigen
antibody (1:100; WBB1281; Wuhan Boster Biological Technology, Ltd.,
Wuhan, China) was added, followed by incubation at 4°C overnight.
PBS substituting primary antibody was used as a control. After PBS
washing, phycoerythrin (PE)-labeled secondary goat anti-mouse IgG
antibody (1:500; sc-2031; Santa Cruz Biotechnology, Inc., La Jolla,
CA, USA) was added, followed by incubation at 37°C for 1 h.
Sections were stained using 4′,6-diamidino-2-phenylindole (DAPI;
Sigma-Aldrich), followed by observation under a BX61 fluorescent
microscope (Olympus Corporation, Tokyo, Japan) to obtain images.
The red fluorescence (PE staining) was presented in human nuclei,
and the blue fluorescence (DAPI staining) was presented in all
nuclei.
General observation of PU
wound-healing rate
Sterile, transparent graph paper was used to draw
the wound shape, in order to calculate the wound area and the
wound-healing rate. The wound-healing rate was calculated as
follows: Wound-healing rate = (Original wound area - area at
detection)/original wound area × 100%. A healing rate of >95%
was considered to indicate complete recovery.
Reverse transcription-quantitative
polymerase chain reaction (RT-qPCR)
On days 1, 3 and 7 post-transplantation, the animals
were intraperitoneally anesthetized and 3-g PU tissue specimens
were collected. The total RNA was extracted using TRIzol™ reagent
(Invitrogen Life Technologies Inc., Carlsbad, CA, USA) according to
manufacturer's instructions. RT-qPCR was performed using
PrimeScript™ RT kits (Takara Biotechnology Co., Ltd., Dalian,
China) according to the manufacturer's instructions. The reverse
transcription reaction condition occurred at 37°C for 15 min,
followed by 85°C for 5 sec, and the reaction system (20 µl for each
sample) was as follows: PrimeScript Buffer (5X), 4 µl; PrimeScript
RT Enzyme Mix I, 1 µl; Oligo Dt Primer (50 µmol/l), 1 µl; Random
6-mers (100 µmol/l), 1 µl; and total RNA, 13 µl. The PCR system (15
µl for each sample) was as follows: Premix Ex Taq (2X), 7.5 µl;
forward primer (10 µmol/l), 0.25 µl; reverse primer (10 µmol/l),
0.25 µl; cDNA (5 ng/µl), 3 µl; and dH2O, 4 µl. Primers
were designed and synthesized by Shanghai Invitrogen Biotechnology
Co., Ltd. (Shanghai, China) (Table
I). After an initial denaturation step of 15 min at 95°C, the
PCR cycling conditions were as follows: for TNF-α, 50 cycles of
95°C for 15 sec, 61°C for 15 sec, and 72°C for 15 sec; for VEGF, 40
cycles of 95°C for 10 sec, 58°C for 15 sec, and 72°C for 10 sec.
The relative expression level was determined using the
2−ΔΔCt analysis method (14).
 | Table I.Primer sequences. |
Table I.
Primer sequences.
| Gene | GenBank accession
no. | Forward (5′-3′) | Reverse (5′-3′) |
|---|
| TNF-α | NM_012675.3 |
TCAGTTCCATGGCCCAGAC |
GTTGTCTTTGAGATCCATGCCATT |
| VEGF | NM_031836.2 |
GCACGTTGGCTCACTTCCAG |
TGGTCGGAACCAGAATCTTTATCTC |
| β-actin | NM_031144.2 |
GGAGATTACTGCCCTGGCTCCTA |
GACTCATCGTACTCCTGCTTGCTG |
Enzyme-linked immunosorbent assay
(ELISA)
On days 1, 3 and 7 post-transplantation, the animals
were intraperitoneally anesthetized and whole blood samples were
extracted from the abdominal aorta. The samples were left at room
temperature for 1.5–2 h and then centrifuged at 1,509 × g at −4°C
for 20 min. Serum was isolated for the ELISA and the optical
density was measured at 450 nm. Serum levels of vascular
endothelial growth factor (VEGF) and tumor necrosis factor-α
(TNF-α) were calculated according to the linear regression equation
of standard curves.
Statistical analysis
All statistical analysis was performed using SPSS
software, version 17.0 (SPSS, Inc., Chicago, IL, USA). Data are
presented as the mean ± standard deviation. Comparisons between two
groups were performed using the t test. P<0.05 was considered to
indicate a statistically significant difference.
Results
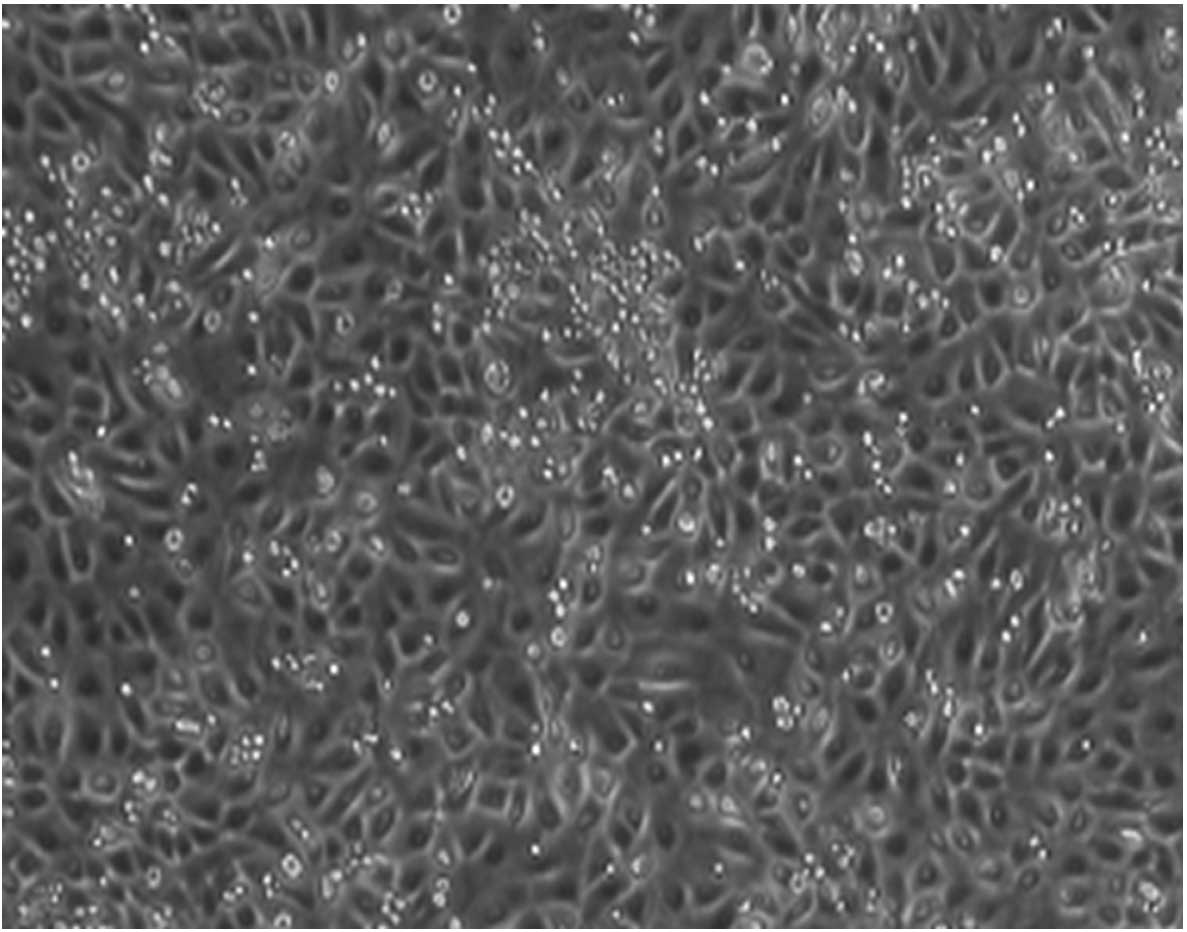
Morphology and phenotype
identification
The confluence rate of third-generation hAECs
cultured for 3–4 days was ≤80%. Cell morphology was predominantly
ovoid, with slabstone- and cobblestone-like growth patterns
(Fig. 1).
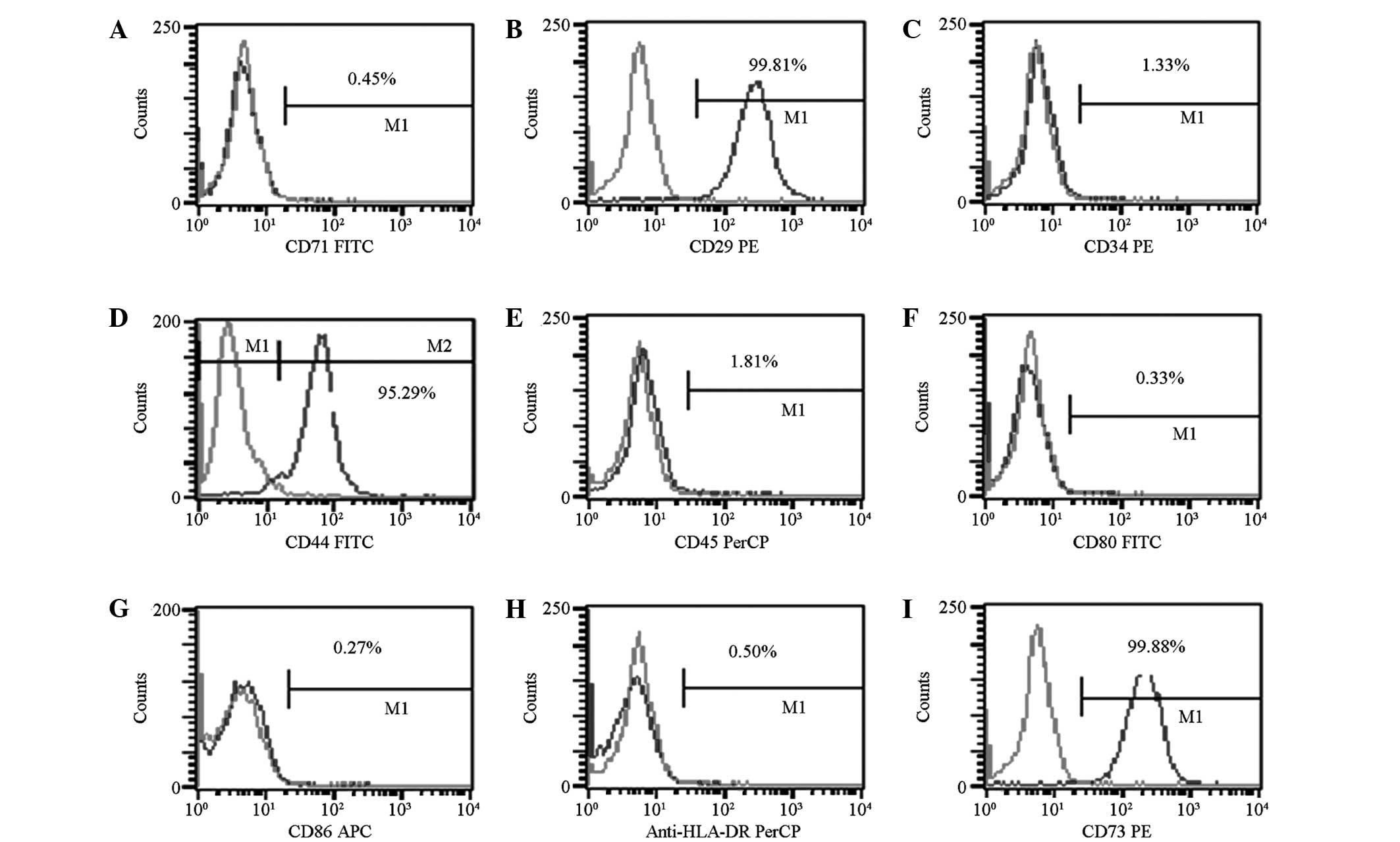
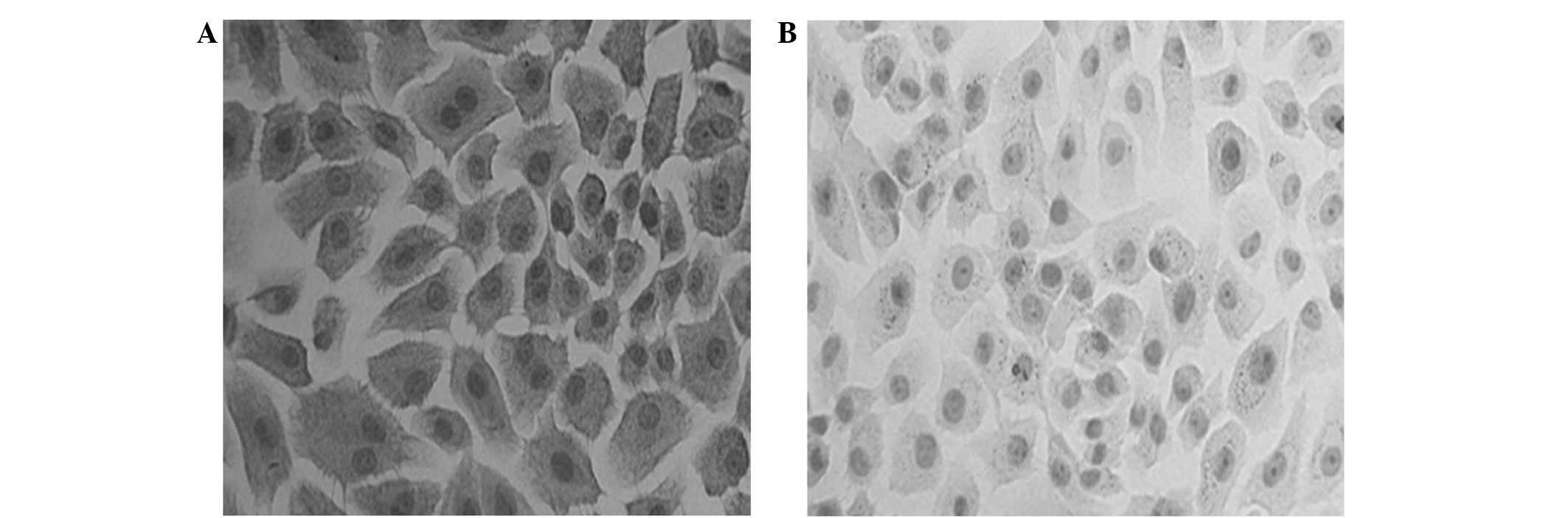
Identification of hAECs by flow
cytometry
Flow cytometric analysis and the immunocytochemical
staining revealed that the isolated and cultured third-generation
hAECs did not express cluster of differentiation (CD) 34, CD45,
CD71, CD80 or CD86; however, the cells did express CD44, CD29, CD73
and CK19, which is consistent with the characteristic features of
hAECs (Figs. 2 and 3).
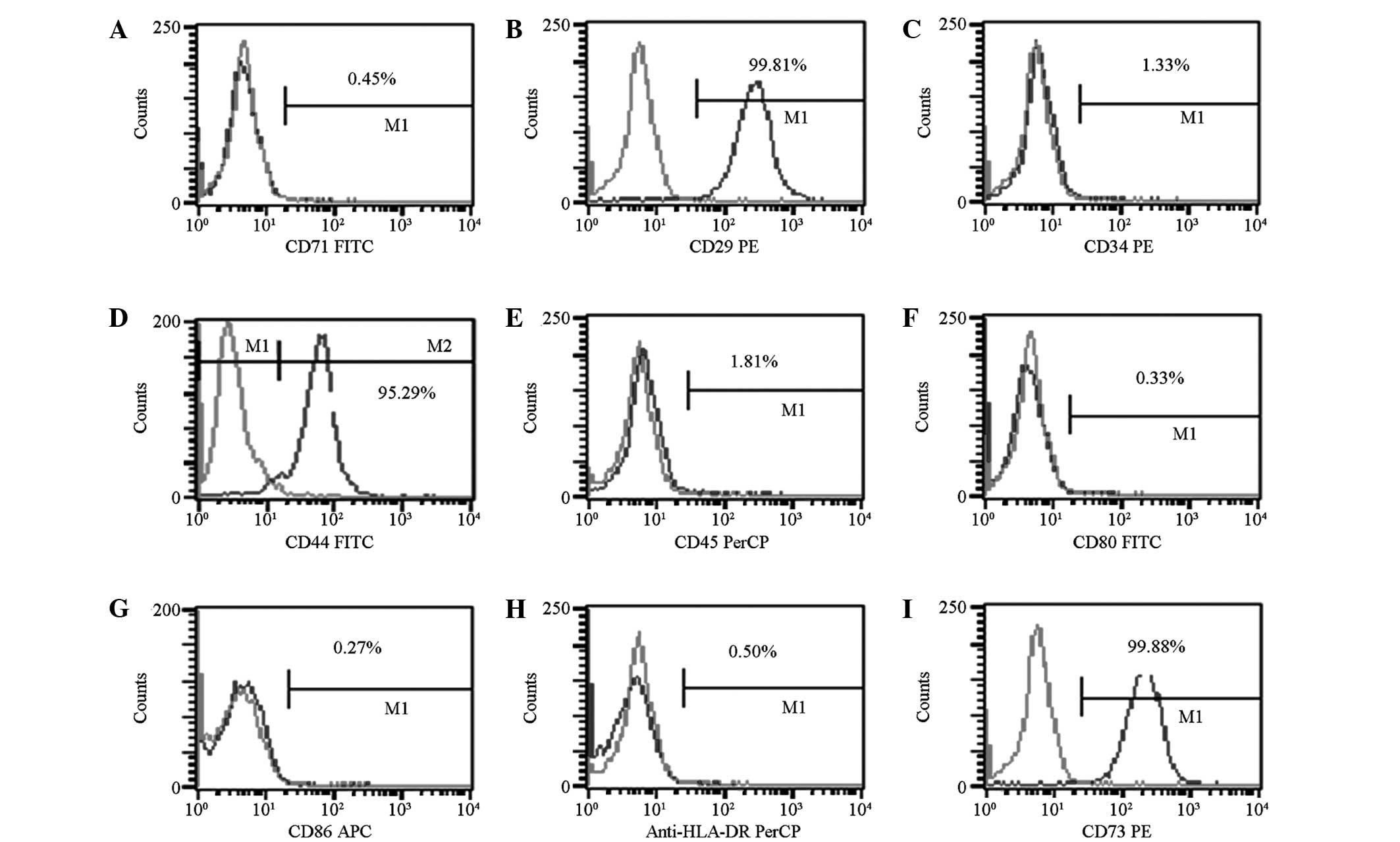 | Figure 2.Phenotypic identification of human
amniotic endothelial cells: (A) CD71, (B) CD29, (C) CD34, (D) CD44,
(E) CD45, (F) CD80, (G) CD86, (H) anti-HLA-DR and (I) CD73. CD,
cluster of differentiation; HLA-DR, anti-human leukocyte
antigen-death receptor; FITC, fluorescein isothiocyanate; PE,
phycoerythrin; APC, allophycocyanin. |
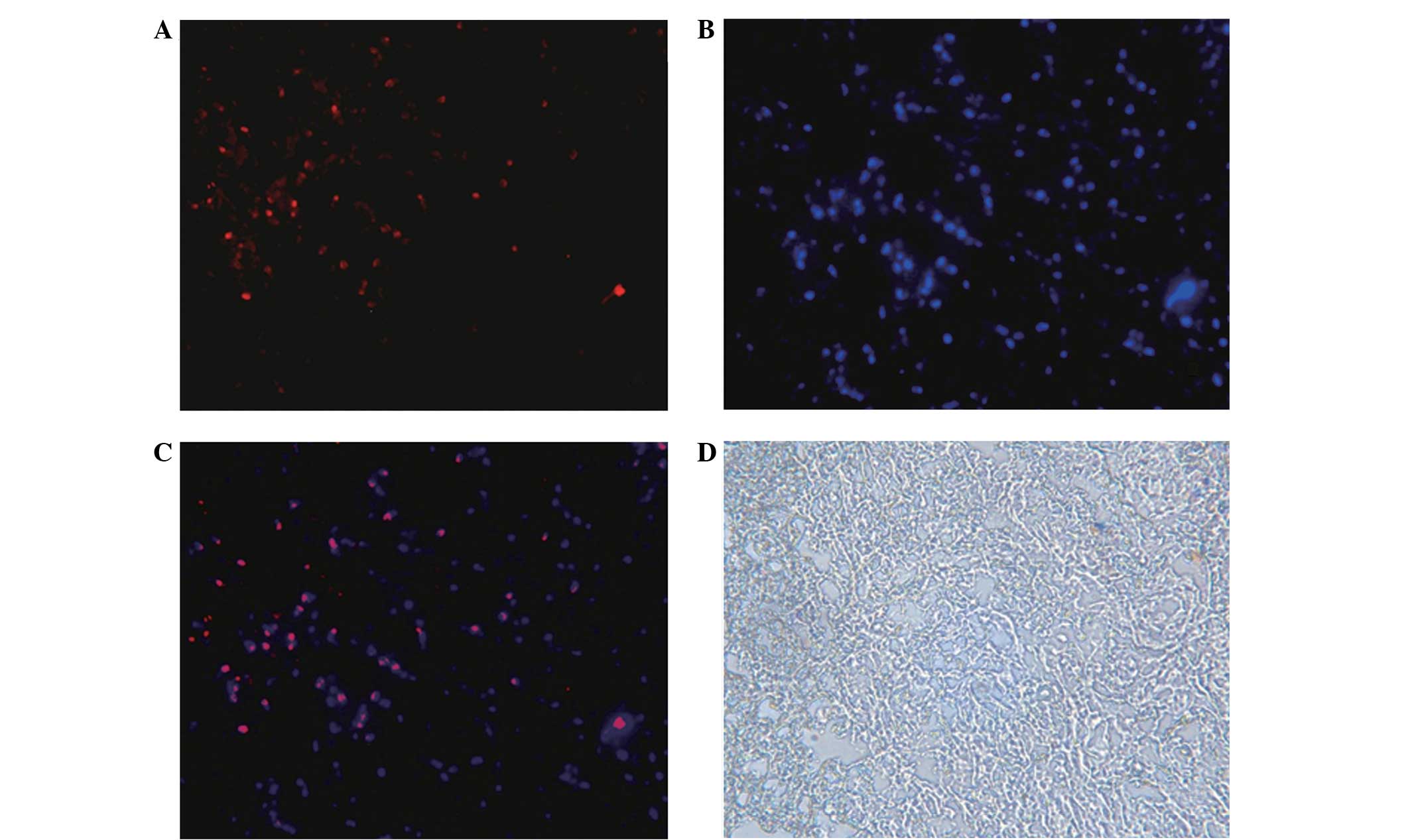
Survival status of hAECs
Immunofluorescence staining showed that, on
post-transplantation day 7, the hAECT-group cells were positive for
human nucleus-specific antigens under the transplantation
subcutaneous region (MAB1281 positive, red fluorescence),
indicating that on day 7 the hAECs remained alive in the rat skin
tissues (Fig. 4).
Wound observation
On day 1 after the corresponding treatment in each
group, the wound-healing rates of the conventional treatment and
hAECT group were increased compared with the rate of the model
group (P<0.05). At day 3, the wound-healing rate of the hAECT
group was significantly elevated compared with that of the model
group and the conventional treatment group (P<0.05). On day 7,
the wound-healing rate of the hAECT group remained significantly
elevated compared with that of the model and conventional treatment
groups (P<0.05), and the wound-healing rate of the conventional
treatment group was increased compared with that of the model group
(P<0.05) (Table II).
 | Table II.Would-healing rate changes following
hAECT. |
Table II.
Would-healing rate changes following
hAECT.
| Group | Day 1 (%) | Day 3 (%) | Day 7 (%) |
|---|
| Model |
9.67±1.11 |
14.83±1.47 |
70.29±2.54 |
| Conventional
treatment |
10.17±1.17a |
16.33±1.11 |
71.71±3.45a |
| hAECT |
12.33±1.97a,b |
47.67±3.14a,b |
91.43±2.13a,b |
Compared with the model and conventional treatment
groups, the wound healing time of the hAECT group was significantly
reduced (P<0.01 and P<0.05, respectively). The wound healing
time of the conventional treatment group was significantly reduced
compared with that of the model group (P<0.05) (Table III).
 | Table III.Wound-healing time of each group. |
Table III.
Wound-healing time of each group.
| Group | Healing time
(days) |
|---|
| Model |
9.83±0.69a |
| Conventional
treatment |
9.17±0.69b,c |
| hAECT |
5.5±1.52 |
Expression of VEGF
On post-transplantation days 1, 3 and 7, the
expression levels of VEGF mRNA and protein in the model,
conventional treatment and hAECT groups were increased compared
with those in the normal control group (P<0.01). VEGF expression
levels in the hAECT group were significantly elevated compared with
those in the model and conventional treatment groups (P<0.05).
On post-transplantation day 7, the expression levels of VEGF mRNA
and protein in the conventional treatment group were higher
compared with those in the model group (P<0.05) (Tables IV and V).
 | Table IV.Relative expression levels of VEGF
mRNA in the pressure ulcer wound tissue of each group. |
Table IV.
Relative expression levels of VEGF
mRNA in the pressure ulcer wound tissue of each group.
| Group | Day 1 | Day 3 | Day 7 |
|---|
| Normal |
5.16±1.44 |
5.13±1.76 |
5.34±1.08 |
| Model |
11.83±4.94a |
11.76±3.52a |
8.64±1.16a,b |
| Conventional
treatment |
12.97±5.78a |
11.66±2.76a |
10.00±1.29a,c |
| hAECT |
24.88±7.39a,b,c |
24.33±6.58a,b,c |
15.63±3.46a,b,c |
 | Table V.Comparison of serum VEGF levels in
each group. |
Table V.
Comparison of serum VEGF levels in
each group.
| Group | Day 1 (ng/l) | Day 3 (ng/l) | Day 7 (ng/l) |
|---|
| Normal |
12.18±1.07 |
11.78±1.20 |
12.24±1.35 |
| Model |
14.46±1.16a |
22.50±2.96a |
17.35±1.60a |
| Conventional
treatment |
14.54±0.53a |
22.37±2.26a |
16.49±1.63a |
| hAECT |
21.28±2.39a,b,c |
25.45±1.11a,b,c |
19.65±0.42a,b,c |
Expression levels of TNF-α
On post-transplantation days 1, 3 and 7, the
expression levels of TNF-α mRNA and protein in the model and
conventional treatment groups were significantly increased compared
with those in the normal control group (P<0.01). On
post-transplantation days 3 and 7, the expression levels of TNF-α
mRNA and protein in the hAECT group were significantly reduced
compared with those in the model and conventional treatment groups
(P<0.01) (Tables VI and VII).
 | Table VI.Relative expression levels of TNF-α
mRNA in the pressure ulcer wound tissue of each group. |
Table VI.
Relative expression levels of TNF-α
mRNA in the pressure ulcer wound tissue of each group.
| Group | Day 1 | Day 3 | Day 7 |
|---|
| Normal |
2.12±0.53 |
2.11±0.21 |
2.19±0.37 |
| Model |
3.97±0.95a |
3.24±0.26a |
3.02±0.15a |
| Conventional
treatment |
3.97±0.68a |
3.41±0.36a |
3.09±0.12a |
| hAECT |
3.00±0.49a |
2.68±0.25a,b,c |
2.23±0.55a,b,c |
 | Table VII.Comparison of serum TNF-α levels in
each group. |
Table VII.
Comparison of serum TNF-α levels in
each group.
| Group | Day 1 (ng/l) | Day 3 (ng/l) | Day 7 (ng/l) |
|---|
| Normal |
28.46±1.96 |
28.94±1.98 |
27.71±1.78 |
| Model |
83.16±4.65a |
73.03±2.85a |
50.94±2.69a |
| Conventional
treatment |
80.69±5.02a |
71.40±4.67a |
50.54±1.99a |
| hAECT |
75.58±3.75a |
51.40±2.44a,b,c |
31.85±2.75a,b,c |
Discussion
hAECs exhibit the property of ‘immune privilege’ and
do not express the human leukocyte antigen-A, B, C and DR antigens.
Grafted hAECs are also able to secrete immunosuppressive factors,
such as TNF-α, TNF-related apoptosis-inducing ligand and TGF-β,
thus inhibiting the chemotactic activities of neutrophils and
macrophages (15,16). In addition, hAECs exhibit no
telomerase activity, and thus may avoid the occurrence of
post-transplantation teratoma. A previous study (17) reported that hAECs express the Oct-4
and Nanog genes, which are key genes in embryonic stem cells for
the maintenance of their differentiation abilities. To date, no
studies have confirmed the expression of HLA-A, B, C and DR
antigens in hAECs (18), indicating
that hAECs experience no repellency and may avoid immune rejection
following the transplantation (19).
In addition, hAECs possess no telomerase and exhibit no
tumorigenicity; therefore, from the view-point of biological
safety, hAECs are ideal donor cells for the treatment of PU
(20).
The results of RT-qPCR indicated that, on days 1, 3
and 7 post-transplantation, the expression levels of VEGF mRNA in
the wounds of the model and conventional treatment groups were
increased compared with those in the normal control group, while
the expression levels of the hAECT group were significantly higher
than those of the model and conventional treatment groups.
Furthermore, the ELISA results suggested that the serum VEGF level
began to increase on day 1 after hAECT, and was significantly
higher than that of the other groups by day 3. By day 7, the serum
VEGF content in the hAECT group remained elevated compared with
that in the other groups, while it was decreased compared with the
levels detected on day 1. VEGF, also known as vascular permeability
factor, is a glycoprotein originally isolated from an in
vitro culture of bovine pituitary stellate cells (21). Numerous experiments (22,23) have
confirmed that VEGF performs two primary functions: i) VEGF
specifically promotes the proliferation of endothelial cells and
induces angiogenesis in vitro and in vivo, with
experiments showing VEGF to be the strongest pro-vascular
endothelial cell mitogen; ii) VEGF induces enhanced microvascular
permeability, resulting in the widespread leakage of plasma
proteins, including fibrinogen, plasminogen and fibronectin
(22,23). These proteins directly or indirectly
alter the extracellular primary constituents, forming a temporary
new matrix to support the migration of endothelial cells and
fibroblasts, which promotes wound healing. In chronic wounds, as
the expression levels of VEGF protein and mRNA are downregulated
compared with those in normal wounds, the rate of angiogenesis
declines, which is considered to inhibit chronic wound healing
(24). The results of the present
study demonstrated that the tissue and serum VEGF content was
increased in the hAECT group, suggesting that hAECs stimulated the
surrounding tissues to secrete VEGF, thus promoting the recovery of
lesion areas.
The results of the RT-qPCR analysis demonstrated
that, on post-transplantation days 1, 3 and 7, the TNF-α mRNA
expression levels in the PU wound tissues of the model and
conventional treatment groups were significantly elevated compared
with those in the normal control group; on days 3 and 7, the TNF-α
mRNA expression levels in the PU wound tissues of the hAECT group
were significantly reduced compared with those in the model and
conventional treatment groups, while the rat serum TNF-α level was
increased compared with that of the normal group (P<0.05). On
days 3 and 7, the serum TNF-α content of the hAECT group was
significantly reduced compared with that of the model and
conventional treatment groups. TNF is an oligomer of glycoproteins;
its receptor is widely distributed and numerous normal cells,
including human vascular endothelial cells, fibroblasts, human
embryonic lung cells and rat liver cells, are able to express TNF
receptor (25). TNF can stimulate
the generation, release and chemotactic response of
polymorphonuclear (PMN) leukocytes in the peripheral blood,
activating and generating a large quantity of toxic products that
cause damage to tissues (26). TNF
exerts direct toxic effects in endothelial cells, such as causing
the cell surface to become procoagulant, thus promoting thrombosis,
and inducing the secretion of neurotransmitters, resulting in the
adhesion and activation of PMN leukocytes. TNF can also affect
liver cells, inhibiting the generation of albumin and promoting the
synthesis of certain acute-phase proteins (27). Two molecular forms of human TNF have
been identified: TNF-α and TNF-β (28,29).
TNF-α, also known as cachectin, is produced by bacterial
lipopolysaccharide-activated monocytes and macrophages and can
induce hemorrhage and necrosis in tumor tissues. TNF-β, also known
as lymphotoxin, is produced by antigen- or mitogen-stimulated
lymphocytes, exhibiting tumor-killing and immunoregulatory
functions (28,29); however, research has tended to focus
on TNF-α, which is a key inflammatory cytokine involved in the
regulation of the immune and inflammatory responses. TNF-α serves
an anti-infection function, in addition to promoting the healing of
damaged tissues. Under certain conditions, TNF-α may be favorable
to the body; however, the excessive generation of TNF-α or
disordered interaction between TNF-α and other cytokines, may cause
a series of inflammatory lesions (26).
The results of the present study suggested that the
wound-healing rate of the hAECT group was increased compared with
that of the model and conventional treatment groups, and the
healing time was reduced compared with that of the model and
conventional treatment groups. The expression levels of TNF-α in
the hAECT group on post-transplantation days 1, 3 and 7 were
significantly elevated compared with those in the normal control,
model and conventional treatment groups, indicating that the hAECs
were able to differentiate and promote wound healing in the
ischemic and hypoxic PU wounds (30,31);
however, the level of TNF-α at day 7 was reduced compared with that
in the model and conventional treatment groups, which further
indicated that, in the late period of wound healing, the
overexpression of TNF-α may lead to its disordered interaction with
other cytokines, resulting in increased inflammatory damage
(20).
In conclusion, hAECs are able to secrete various
growth factors, and hAECT, through subcutaneous injection, appears
to significantly improve the wound-healing rate of stage III PUs in
rats. Further studies may help to elucidate the biological
mechanisms underlying the effects of hAECs in treating PU.
Acknowledgements
This study was funded by the Guizhou Provincial
Science and Technology Fund Committee [no. Qiankehe J LKZ (2012)
no. 23].
References
|
1
|
European Pressure Ulcer Advisory Panel
(EPUAP) and National Pressure Ulcer Advisory Panel (NPUAP):
Pressure Ulcer Treatment: Quick Reference Guide. http://www.epuap.org/guidelines/Final_Quick_Treatment.pdf
|
|
2
|
Gould LJ, Olney CM, Nichols JS, Block AR,
Simon RM and Guihan M: Spinal cord injury survey to determine
pressure ulcer vulnerability in the outpatient population. Med
Hypotheses. 83:552–558. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Lui TH: Technical tip: Percutaneous bone
shaving and ulcer endoscopy to manage abnormal pressure point of
the sole. Foot (Edinb). 24:190–194. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Baharestani MM and Ratliff C: Pressure
ulcers in neonates and children: An NPUAP white paper. Adv Skin
Wound Care. 20(208): 210, 212, 214, 216. 218–220. 2007.
|
|
5
|
Barrufet MP, Vendrell E, Force L, Sauca G,
Rodríguez S, Martínez E, Palomera E, Serra-Prat M, Capdevila JA,
Cornudella J, et al: Prevalence and risk factors for
meticillin-resistant Staphylococcus aureus in an acute care
hospital and long-term care facilities located in the same
geographic area. Rev Esp Quimioter. 27:190–195. 2014.PubMed/NCBI
|
|
6
|
Wang LH, Chen HL, Yan HY, Gao JH, Wang F,
Ming Y, Lu L and Ding JJ: Inter-rater reliability of three most
commonly used pressure ulcer risk assessment scales in clinical
practice. Int Wound J. Sep 16–2014.(Epub ahead of print).
|
|
7
|
Lunn JS, Sakowski SA, Federici T, Glass
JD, Boulis NM and Feldman EL: Stem cell technology for the study
and treatment of motor neuron diseases. Regen Med. 6:201–213. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Lunn JS, Sakowski SA, Hur J and Feldman
EL: Stem cell technology for neurodegenerative diseases. Ann
Neurol. 70:353–361. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Nishimura K and Takahashi J: Therapeutic
application of stem cell technology toward the treatment of
Parkinson's disease. Biol Pharm Bull. 36:171–175. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Miki T, Lehmann T, Cai H, Stolz DB and
Strom SC: Stem cell characteristics of amniotic epithelial cells.
Stem Cells. 23:1549–1559. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Marcus AJ, Coyne TM, Rauch J, Woodbury D
and Black IB: Isolation, characterization and differentiation of
stem cells derived from the rat amniotic membrane. Differentiation.
76:130–144. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ghionzoli M, Repele A, Sartiani L,
Costanzi G, Parenti A, Spinelli V, David AL, Garriboli M, Totonelli
G, Tian J, et al: Human amniotic fluid stem cell differentiation
along smooth muscle lineage. FASEB J. 27:4853–4865. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Jiang ZX, Zhou AT, Zheng XL, et al: The
animal model machine of pressure sores. China Patent
ZL201420090436X Filed. July 16–2014.
|
|
14
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Wu CC, Wu TC, Liu FL, Sytwu HK and Chang
DM: TNF-α inhibitor reverse the effects of human umbilical
cord-derived stem cells on experimental arthritis by increasing
immunosuppression. Cell Immunol. 273:30–40. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Manuelpillai U, Lourensz D, Vaghjiani V,
Tchongue J, Lacey D, Tee JY, Murthi P, Chan J, Hodge A and Sievert
W: Human amniotic epithelial cell transplantation induces markers
of alternative macrophage activation and reduces established
hepatic fibrosis. PLoS One. 7:e386312012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Wan P, Wang X, Ma P, Gao N, Ge J, Mou Y
and Wang Z: Cell delivery with fixed amniotic membrane reconstructs
corneal epithelium in rabbits with limbal stem cell deficiency.
Invest Ophthalmol Vis Sci. 52:724–730. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Marcus AJ, Coyne TM, Black IB and Woodbury
D: Fate of amnion-derived stem cells transplanted to the fetal rat
brain: Migration, survival and differentiation. J Cell Mol Med.
12:1256–1264. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Le Blanc K, Tammik C, Rosendahl K,
Zetterberg E and Ringdén O: HLA expression and immunologic
properties of differentiated and undifferentiated mesenchymal stem
cells. Exp Hematol. 31:890–896. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Javanmard SH, Hasanpour Z, Abbaspoor Z,
Naderian GA and Jahanmard M: Aqueous concentrations of VEGF and
soluble VEGF receptor-1 in diabetic retinopathy patients. J Res Med
Sci. 17:1124–1127. 2012.PubMed/NCBI
|
|
21
|
Neuss S, Becher E, Wöltje M, Tietze L and
Jahnen-Dechent W: Functional expression of HGF and HGF
receptor/c-met in adult human mesenchymal stem cells suggests a
role in cell mobilization, tissue repair and wound healing. Stem
Cells. 22:405–414. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Shizukuda Y, Tang S, Yokota R and Ware JA:
Vascular endothelial growth factor-induced endothelial cell
migration and proliferation depend on a nitric oxide-mediated
decrease in protein kinase Cdelta activity. Circ Res. 85:247–256.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Murohara T, Horowitz JR, Silver M, Tsurumi
Y, Chen D, Sullivan A and Isner JM: Vascular endothelial growth
factor/vascular permeability factor enhances vascular permeability
via nitric oxide and prostacyclin. Circulation. 97:99–107. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Miki T and Strom SC: Amnion-derived
pluripotent/multipotent stem cells. Stem Cell Rev. 2:133–142. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Ma DH, Yao JY, Kuo MT, See LC, Lin KY,
Chen SC, Chen JK, Chao AS, Wang SF and Lin KK: Generation of
endostatin by matrix metalloproteinase and cathepsin from human
limbocorneal epithelial cells cultivated on amniotic membrane.
Invest Ophthalmol Vis Sci. 48:644–651. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Zhang S, He H, Day AJ and Tseng SC:
Constitutive expression of inter-α-inhibitor (IαI) family proteins
and tumor necrosis factor-stimulated gene-6 (TSG-6) by human
amniotic membrane epithelial and stromal cells supporting formation
of the heavy chain-hyaluronan (HC-HA) complex. J Biol Chem.
287:12433–12444. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Li H, Niederkorn JY, Neelam S, Mayhew E,
Word RA, McCulley JP and Alizadeh H: Immunosuppressive factors
secreted by human amniotic epithelial cells. Invest Ophthalmol Vis
Sci. 46:900–907. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Chen X and Oppenheim JJ: Contrasting
effects of TNF and anti-TNF on the activation of effector T cells
and regulatory T cells in autoimmunity. FEBS Lett. 585:3611–3618.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Higashi N: Function, molecular structure
and gene expression regulation of tumor necrosis factor and
lymphotoxin. Nihon Rinsho. 50:1939–1944. 1992.(In Japanese).
PubMed/NCBI
|
|
30
|
Zani A, Cananzi M, Fascetti-Leon F,
Lauriti G, Smith VV, Bollini S, Ghionzoli M, D'Arrigo A, Pozzobon
M, Piccoli M, et al: Amniotic fluid stem cells improve survival and
enhance repair of damaged intestine in necrotising enterocolitis
via a COX-2 dependent mechanism. Gut. 63:300–309. 2014.PubMed/NCBI
|
|
31
|
Akrami H, Soheili ZS, Sadeghizadeh M,
Khalooghi K, Ahmadieh H, Kanavi MR, Samiei S and Pakravesh J:
Evaluation of RPE65, CRALBP, VEGF, CD68 and tyrosinase gene
expression in human retinal pigment epithelial cells cultured on
amniotic membrane. Biochem Genet. 49:313–322. 2011. View Article : Google Scholar : PubMed/NCBI
|