Introduction
The history of paediatric infectious diseases
closely parallels the history of Paediatrics, as infections remain
the major causes of childhood morbidity and mortality (1,2). Viral
paediatric infectious diseases are characterised by a great
heterogeneity of clinical manifestations due to the unique
characteristics of the neonatal period and childhood. Almost 50
years ago, Paediatric Virology was not considered an isolated
discipline and was included in the paediatric infectious diseases
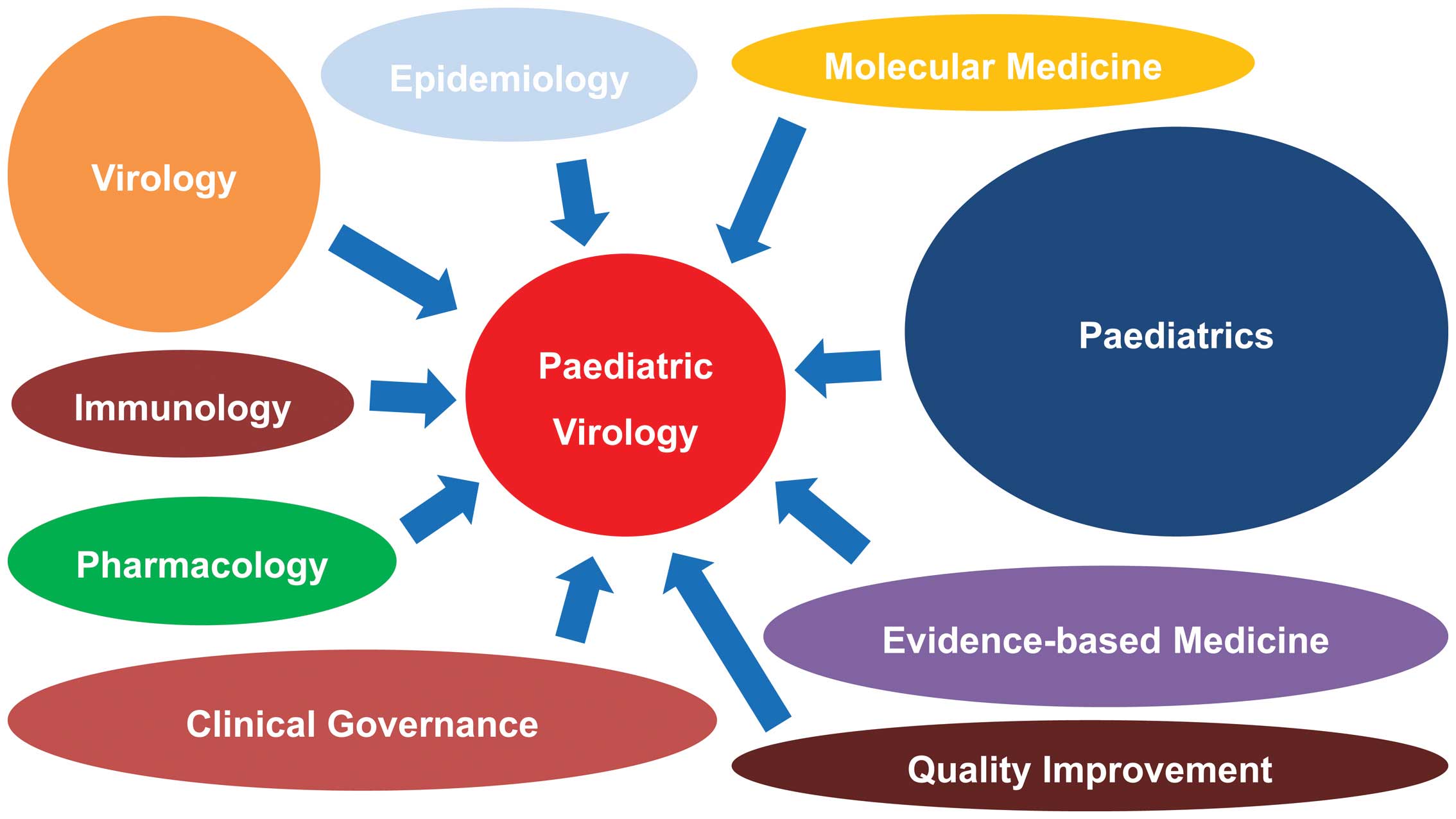
section of the scientific field of Paediatrics (3). However, during the past two decades,
new advances in the field of Clinical Virology and Molecular
Medicine have expanded the level of knowledge on the prevention,
diagnosis and treatment of viral infections occurring in infancy
and childhood. For this reason, although additional subspecialists
in several fields may be diminishing (4), Paediatric Virology as a bold new
scientific field can combine Paediatrics with Virology,
Epidemiology, Molecular Medicine, Evidence-based Medicine, Clinical
Governance, Quality Improvement, Pharmacology and Immunology
(Fig. 1).
To date, paediatric infectious diseases
professionals have achieved a distinct role within the scientific
field of Paediatrics and their contribution to tertiary paediatric
care is valued (2). Their current
clinical and research aims are to resolve important public health
issues in both developed and developing countries. Furthermore, new
emerging diseases, such as severe acute respiratory syndrome
(SARS), west Nile virus (WNV) and Ebola virus (EV) infections,
require new prevention strategies and therapeutic protocols. In
addition, paediatric infectious diseases professionals are involved
in specialised paediatric care and in the follow-up of children
with a history of viral infections, such as viral meningitis or
acquired immunodeficiency syndrome (AIDS), who survive to
adolescent years and beyond, requiring advanced medical care and
technological services. Moreover, newfound social issues have
arisen, including the recent anti-vaccination wave, the financial
crisis and the unprecedented immigration occurring globally and in
Mediterranean countries, in particular (5). These developments and changes
definitely highlight the demand for the continuous education of
paediatric health professionals, informing them of the ongoing
advances in paediatric care and management strategies involved in
the discipline of Paediatric Virology (6,7).
Workshop on Paediatric Virology
The 20th World Congress on Advances in Oncology and
the 18th International Symposium on Molecular Medicine was held in
Athens (Greece) and was attended by >500 participants from the
five continents (8). This annual
scientific meeting attracted its largest number of delegates to
date and over a period of three days, up-to-date basic and clinical
research findings on Molecular Medicine and Oncology were presented
and discussed. For the first time this year, during the third day
of the meeting, participants had the chance to participate in the
Workshop on Paediatric Virology, with the theme ‘Paediatric
Virology: from the lab to clinical practice’ (Fig. 2). This Workshop gathered world
experts on Paediatrics, Neonatology, Virology, Vaccinology,
Epidemiology, Microbiology and Public Health. It was co-chaired by
Professor Anne Greenough, Professor of Neonatology and Clinical
Respiratory Physiology at King's College London in London (UK) and
Vice-President of the Royal College of Paediatrics and Child Health
(RCPCH), Professor Anna Kramvis, Research Professor of Molecular
Virology at the University of the Witwatersrand in Johannesburg
(South Africa) and Professor Maria Theodoridou, Professor of
Paediatrics at the ‘Aghia Sophia’ Children's Hospital in Athens
(Greece). The Workshop was enthusiastically supported by the
Department of Clinical Virology, School of Medicine, University of
Crete in Heraklion (Greece) and the First Department of Paediatrics
of the School of Medicine at the University of Athens in Athens
(Greece).
The initial idea for the birth of this Workshop was
inspired in 2007 at the Wirral University Teaching Hospital in
Wirral (UK), where cytomegalovirus (CMV)-positive twins were
treated at the local Neonatal Intensive Care Unit (NICU) (9), requiring the collaboration of an
extended scientific network in Merseyside and Manchester (UK) for
the management of this neonatal viral infection. Two years later,
in October 2009, during the oral session at the 14th World Congress
on Advances in Oncology and the 12th International Meeting in
Molecular Medicine, which was devoted to human papilloma virus
(HPV) infection in childhood (10)
and chaired by Professor Maria Theodoridou, Professor of
Paediatrics at the ‘Aghia Sophia’ Children's Hospital in Athens
(Greece), this idea was re-enforced by a group of young paediatric
trainees and junior researchers, leading to the creation of the
Paediatric Virology Study Group (PVSG). The fundamental aim of the
PVSG was to provide an array of scientific and educational
activities, bringing together Virology with Paediatrics within a
single entity. Covering Basic Sciences and Clinical Medicine, the
PVSG was open to scientists interested in the field of Paediatric
Virology, either as basic scientists, researchers and virologists
or as medical students, paediatric trainees, general
paediatricians, paediatric infectious diseases physicians and
allied health professionals. Six years later, on October 2015, the
PVSG had the great honour to coordinate the ‘Workshop on Paediatric
Virology’ as an official session of the 20th World Congress on
Advances in Oncology and the 18th International Meeting in
Molecular Medicine. This Workshop was dedicated to promoting
international scientific exchange and cooperation of both
clinicians and researchers on Paediatric Virology and improving
biomedical research and paediatric medical practice on viral
infections occurring in childhood. In this review, we present an
update on selected topics presented at the Workshop.
Update on current views and advances on
Paediatric Virology
Viral infections and long-term
outcomes of prematurely born infants
Respiratory syncytial virus (RSV) is a common
respiratory pathogen in young children (11). Between 1 and 2% of infected children
will require hospitalisation and up to 8% of those hospitalised
will require mechanical ventilation. Numerous studies (12–16) have
demonstrated that infants born at term, who were previously
healthy, subsequent to an RSV lower respiratory tract infection
(LRTI), develop chronic respiratory morbidity. There are many risk
factors for severe acute RSV infection, which include being born
prematurely and having developed bronchopulmonary dysplasia (BPD).
Greenough et al (12) have
demonstrated that up to school age, those prematurely born
children, who had developed BPD and an RSV LRTI requiring
hospitalisation in infancy, had increased healthcare utilisation
and worse lung function, particularly affecting small airways, than
children with BPD, who had not been hospitalised due to RSV.
Healthcare utilisation in the first two years after birth was also
shown to be increased even in moderately prematurely born infants
(32–35 weeks of gestation), who had were hospitalised due to RSV
(13). In two prospectively followed
cohorts, one very prematurely born cohort (14) and the other, which included pre-term
infants of a wide range of gestational ages (24–35 weeks),
respiratory morbidity was greater during infancy in those who had
had an RSV LRTI (15,16). In the very prematurely born cohort,
subsequent respiratory morbidity was increased after an RSV LRTI
regardless of whether hospitalisation was required or the infant
had BPD (14). The prematurely born
infants, who required hospitalisation due to an RSV LRTI, had
poorer premorbid lung function (17). It has also been identified that
prematurely born infants may have a genetic predisposition to
developing RSV LRTIs. In addition, single nucleotide polymorphisms
(SNPs) in several genes were found to be associated with chronic
respiratory morbidity during infancy and reduced lung function at
one year following an RSV LRTI (18). Other respiratory viral infections
also adversely influence respiratory outcomes during infancy in
those born prematurely, including human metapneumovirus (hMPV) and
human rhinovirus (HRV), particularly HRV-C (19).
Defeating polio: Vaccine anniversary
(1955–2015)
Poliomyelitis is an acute infectious disease
affecting humans, occurring particularly in children, which is
caused by small ribonucleic acid (RNA) viruses of the enterovirus
group of the family Picornavidae (20–26).
Three antigenically distinct strains (strains 1, 2 and 3) are
known, with-type 1 accounting for 85% of cases. The clinical
manifestations of the disease vary greatly. Most cases are
asymptomatic; paralytic illness is rare, affecting <1% of
infected individuals. The year 2015 is the 60th anniversary since
Jonas Salk launched the inactivated polio vaccine (IPV), enabling
children to be protected against the crippling disease of
poliomyelitis. With the development of the oral polio vaccine (OPV)
by Albert Sabin in 1961, the world was given the tools, with which
to stop outbreaks, strengthen and build immunity, to ensure that
children can grow up without the threat of polio. The combination
of OPV and IPV led to the eradication of polio in the Americas, the
western Pacific and Europe. Today, 80% of the world population
lives in polio-free regions. Nevertheless, Pakistan, Afghanistan
and Nigeria are countries where polio is still categorised as an
endemic viral infection. It should be noted that in 2013–2014 an
upsurge of polio in areas, which were considered polio-free,
occurred. The confirmed circulation of wild-type poliovirus (WPV)
in Israel and the outbreak of acute flaccid paralysis (AFP) in
Syria mean that there is a high risk of the disease being
reintroduced into Europe. Europe should implement a prevention
policy, which is based on enhancing the vaccination of resident and
refugee populations, strengthening surveillance and being prepared
to rapidly respond to the identification of polio. In Greece, there
is a national action plan, which includes programmes to sustain
high levels of polio immunisation coverage, AFP surveillance and
actions in the event of a suspected or confirmed poliomyelitis
case. Fighting polio with vaccination has been one of the most
successful public health programmes in history, reducing the number
of polio cases by 99%, making possible the expectation towards
disease eradication.
Clinical implications of hepatitis B
virus (HBV) genotypes in Paediatrics
Even though a successful vaccine against HBV has
been implemented in 184 countries, the eradication of HBV is still
not on the horizon (27). According
to the World Health Organization (WHO), there are 240 million
chronic carriers of the virus, globally (28). The risk of developing chronic
hepatitis ranges from >90% in newborns of hepatitis B e antigen
(HBeAg)-positive mothers, 25–35% in children under the age of 5 and
<5% in adults (29). HBeAg, a
non-particulate viral protein, is conventionally considered a
marker of HBV replication (30).
This is the only antigen of HBV, which can cross the placenta
(31), leading to the specific
unresponsiveness of helper T cells to the hepatitis B capsid
protein (HBcAg) and HBeAg in newborns of HBeAg-positive mothers
(32). HBeAg is tolerated in
utero and acts as a tolerogen after birth (33). Thus, perinatal transmission is
frequent when mothers are HBeAg-positive, whereas it occurs
significantly less frequently when mothers are HBeAg-negative
(34–36).
Sequence heterogeneity is a characteristic of HBV,
the prototype member of the family Hepadnaviridae (37). Based on an intergroup divergence of
>7.5% across the complete genome, HBV has been classified
phylogenetically into at least 9 genotypes. With between ~4 and 8%
intergroup nucleotide divergence across the complete genome and
good bootstrap support, genotypes A-D, F, H and I are further
classified into subgenotypes. HBV genotypes and in some cases
subgenotypes have a distinct geographical distribution both
globally and locally (37). The
different genotypes/subgenotypes can develop different mutations in
the regions of the HBV genome, which code for HBeAg and the
envelope proteins. These differences can be related to the role of
the HBV genotypes, to their mode of transmission, to the clinical
manifestation of the disease following HBV infection and to their
response to antiviral therapy. Thus, the genotypes/subgenotypes of
HBV may be responsible for the different modes of transmission and
natural history of infection in children, noted in different
regions of the world, where distinct genotypes/subgenotypes
prevail.
Implementation of vaccination against
HPV in a country under financial crisis
Despite the invention of the Pap smear test by
George N. Papanicolaou almost 90 years ago, HPV is considered the
most frequent carcinogen in humans, causing approximately 530,000
cases of cervical cancer per annum, with the majority of cases
occurring in developing countries (38–40). The
link between this deoxyribonucleic acid (DNA) virus and cervical
cancer was firstly suspected in the early 1970s by Professor Harald
zur Hausen, who in 2008 received the Nobel Prize in Physiology and
Medicine (41). In the same year,
two vaccines against HPV, the bivalent HPV 16/18 and the
quadrivalent HPV 6/11/16/18, were implemented into clinical
practice in several countries, worldwide (42). However, despite the significant
calculated expected health benefits following the implementation of
HPV vaccination programmes, current trends indicate low HPV
vaccination uptake among female adolescents in several countries in
Europe (43–46). These studies have also focused on
potential socio-demographic factors, which influence parents'
decisions to decline HPV vaccination to their daughters, including
age, ethnicity, receipt of childhood vaccines, knowledge,
attitudes, parental and community acceptability. Of note, in
Greece, a country under financial crisis since 2010, in which
several health quality indexes have already deteriorated (47), financial reasons have also been
elucidated behind non-vaccination against HPV (38). Since data on HPV vaccination among
female adolescents in Greece remain limited, the first pilot
cross-sectional questionnaire-based study, known as the ELEFTHERIA
study, was expected to assess HPV vaccination uptake among female
adolescents in Greece during the period between 2008–2014 and to
investigate socio-demographic reasons for declining HPV vaccination
(38). It was designed by the First
Department of Paediatrics at the University of Athens and the
Department of Clinical Virology at the University of Crete and its
name was inspired by ‘Eleftheria’, the name of the first
adolescent, who was recruited in the study. The preliminary
findings of this project stress the need to provide and maintain
health insurance coverage to children in countries under financial
crisis (38). For this reason,
urgent health policy responses to the recent financial collapse in
Greece are required as the full impact of austerity measures
unfolds in the coming years.
Children and Ebola infection
EV was first discovered in 1976 and has caused three
outbreaks, two simultaneously in 1976 and one in 2014 (48). The exact mode of transmission of EV
remains unknown; however, it seems to be transmitted from the
biological fluids of wild animals and subsquently through
human-to-human contact (49).
According to the WHO, the 2014 west African outbreak claimed a case
fatality, which ranged from 25 to 90% and a total number of roughly
10,000 fatalities; the number of children is unknown (49). This fact makes it a potential lethal
tool in bio-warfare. If used in residential areas or within the
public transportation system, as a biological agent, EV can easily
affect the welfare and life of children.
Emergency Departments (EDs) should be ready for such
attacks, especially catering for the needs of paediatric victims
(50,51). Carley's consensus statement for
formulating major incident plans can be quite helpful (52). Local tertiary paediatric hospitals or
peadiatric units should play an active role by coordinating the
care of children. Planning for such events involving children
should be carried out by experienced clinicians in Paediatrics.
Approximately 10–15% of the equipment used in general hospitals
should be suitable for peadiatric victims of all ages. Staff
training for major incidents should be regular and should include
caring for children. While triaging, it is advisable to use
modified adult scoring systems. In particular, when triaging a
large number of children, the Eichelberger modification to the
triage revised trauma score should be used (48). If possible, children's assessment and
treatment, as well as transfers, when needed, should be provided by
experienced paediatric teams. If allowed by the senior clinician,
parents could possibly stay on site near their children. During
hospitalisation and following discharge, adequate support should be
provided to the families (52). An
ED should be ready to accommodate the needs of children following
an EV attack by offering personal protective equipment (PPE) to
staff, appropriate decontamination and isolation facilities and
antidotes, if available, as well as general paediatric equipment.
Staff should always suspect bioterrorism if a few or several people
present with unusual or unexpected symptoms or if their symptoms do
not conform with a certain medical diagnosis. Identify, isolate and
inform is the current standard approach to EV suspicion (53). Hopefully, none of this will be
actually needed in the near future.
Viral bronchiolititis in Paediatric
Intensive Care Unit (PICU)
Viral bronchiolitis, mainly caused by RSV infection,
remains the leading cause of infant admission to the PICU (54,55).
Recent laboratory tools have also confirmed many other viruses to
account for bronchiolitis, either as co-infection with RSV or as
the only aetiological pathogen. Such viruses are HRV, hMPV,
adenovirus, as well as influenza and parainfluenza viruses
(56). Even following the anti-RSV
post-prophylaxis era, RSV seems to be the most common cause of
bronchiolitis in infancy and is responsible for severe clinical
manifestations, longer hospitalisation and PICU admissions
(57). Severe bronchiolitis is
indicated by persistently increased respiratory effort (tachypnoea,
nasal flaring, intercostal, subcostal or suprasternal retractions,
accessory muscle use and grunting) hypoxaemia, apnoea or acute
respiratory failure. Risk factors for severe disease and/or
complications of bronchiolitis, even death, are considered to be
prematurity (gestational age <37 weeks), age <12 weeks,
chronic pulmonary disease, particularly BPD (also known as chronic
lung disease), congenital and anatomic defects of the airways,
congenital heart disease, immunodeficiency and neurologic disease
(58). Though it is a common and old
clinical entity, there is a wide variety in clinical practice and
the need to clarify each of the therapeutic means has to be done
with large, well-designed clinical studies. When it comes to the
treatment of critically ill children, there is a paucity of
evidence-based guidelines. Fluid replacement, oxygen
supplementation and close monitoring are the first steps in the
management of the disease. The role of epinephrine and nebulised
bronchodilators in combination with systemic corticosteroids is
questioned, but can be given on an individualised basis (59). Nebulised hypertonic saline is a new
therapeutic agent, which has not been investigated for possible use
in the PICU. Although it is recommended, its use remains to be
established. Other therapies, such as Heliox, surfactant and
ribavirin, are also being examined, with controversial results thus
far. As little seems to have been achieved when it comes to
treatment, a lot of emphasis has been given to the prevention of
the illness. Hygiene measures and education of caregivers, hospital
personnel, nurses and doctors on limiting transmission and
elimination of the environmental risk factors are strongly
recommended in published guidelines (59). Palivizumab prophylaxis is recommended
for infants with risk factors, such as chronic illnesses,
prematurity and immunodeficiency, as well as other conditions,
which are being clarified at the revised published guidelines
(59). Since the burden of RSV
bronchiolitis is high, research must aim for the development of an
anti-RSV vaccine, as well as new antiviral agents.
Vaccination against measles, mumps and
rubella (MMR) versus autism
Autism is a severe neurodevelopmental disorder
affecting the paediatric population (60). Autism spectrum disorders (ASD)
include disorders, such as psychomotor regression, language
impairment and behavioural social withdrawal, placing patients with
ASD in permanent need for healthcare and social support (61). Earlier reports have associated
vaccination against MMR with the occurrence of ASD in children
(62), thus leading in particularly
low vaccination coverage. As a result, outbreaks regarding the
vaccine preventable strains have reappeared throughout Europe
(63–65), Asia (66,67) and
the United States (68,69). Extensive research around the issue
has emerged, soundly dissociating MMR vaccination from any ASD
occurrence, even in high-risk populations (70–72).
However, the loss of credibility of the MMR vaccine remains a
concern. This can be partially explained by failure on behalf of
the scientific community to effectively communicate: i) the
limitations and bias of the original study of Wakefield et
al (62) in 1998, ii) the
mounting evidence supporting the lack of a causal relationship
between MMR vaccine receipt and autism onset, as proven by large
epidemiological studies (70–72) and
iii) adverse effects of vaccination in the general setting of
coincidental, rather than causal associations. Another contributing
factor must be attributed to a powerful influence by the public
media, such as television, newspapers and internet, regarding MMR
vaccination, ultimately leading to a subsequent negative public
health response. In the future, more effective communication
strategies are required to reassure parents of vaccine safety and
importance.
Ocular viral infections in neonates
and children
The ocular manifestations of viral infections in
neonates and children vary greatly and can range from innocuous to
vision threatening (73). The
majority of viral conjunctivitis in children are caused by
adenovirus, a DNA virus, which can cause a range of human diseases,
including upper respiratory tract infection. Viral conjunctivitis
is associated with epidemic keratoconjunctivitis,
pharyngoconjunctival fever and acute haemorrhagic conjunctivitis
(74). Signs include eyelid oedema
and tender pre-auricular lymphadenopathy, prominent conjunctival
hyperaemia, follicles and punctate epithelial keratitis. In viral
infections in children, the involvement of the anterior segment is
mild and self-limited; spontaneous resolution usually occurs within
2–3 weeks, except in cases of congenital infection, which are often
associated with significant alterations in ocular structures.
Neonatal conjunctivitis (also known as ophthalmia
neonatorum) is defined as conjunctival inflammation developing
within the first month of life. It is the most common type of
infection in neonates, occurring in up to 10% of neonates. It is
often identified as a specific entity distinct from conjunctivitis
in older infants as it is often the result of infection transmitted
from the mother to the infant during delivery (74). Molluscum contagiosum ocular
infection in children is caused by a specific double-stranded DNA
poxvirus, which typically affects otherwise healthy children with a
peak incidence between the ages of two and four. Transmission
occurs through contact, with subsequent autoinoculation.
Presentation is with chronic unilateral ocular irritation and mild
discharge, while lesions are usually self-limiting. Primary
infection with herpes simplex virus (HSV) is usually associated
with eyelid and periorbital vesicles, papillary conjunctivitis,
discharge and lid swelling. Dendritic corneal ulcers can also be
present, particularly in patients with atopic infection can lead to
eczema herpeticum, which can be very severe (75–77).
Varicella-zoster virus (VZV) is a serious, but rare, viral
infection in children, in which prolonged inflammation may lead to
corneal thinning or perforation, glaucoma and cataract formation
(74).
Involvement of the posterior structures mostly
related to HSV and VZV is potentially sight-threatening. Retinal or
optic nerve involvement should be suspected in any child, who
complains of an acute onset of blurred vision in the absence of
anterior segment inflammation or opacities in the ocular media.
Optic neuropathy may occur as an isolated sign, although it is more
often associated with a more generalised involvement of the central
nervous system (77,78). While specific therapy is not always
available, the early diagnosis of ocular viral disease in children
should aid in the amelioration of acute symptoms and in the
prevention of long-term complications.
Otorhinolaryngologists versus
HPV-associated lesions
HPV is responsible for many benign lesions of the
airway tract and the genital area in the adult population, as well
as for cancer of the larynx and oral cavity, particularly subtypes
16 and 18 (79,80). A recent study (81) also revealed an increased frequency of
HPV infections in neonates and children. Otorhinolaryngologists are
the specialists, who treat children with HPV-related lesions
localised in the oral cavity, the oropharynx and larynx. These
lesions are mostly benign. There are four types of HPV-related
lesions concerning the upper airway track: i) squamous papilloma,
ii) verruca vulgaris, iii) focal epithelial hyperplasia and iv)
condyloma acuminatum.
In children, the most common clinical expression of
HPV is recurrent respiratory papillomatosis (RRP). It causes
hoarseness of the voice and sometimes the lesions can cause
obstruction of the upper airway track. In adults, the clinical
behaviour differs, as the disease requires fewer surgical excisions
than in children. In children, the lesions caused by HPV often need
many surgical procedures before they become extinct and quiescent.
Inverted papilloma, which is a type of squamous papilloma, is
strongly associated with HPV subtypes 6 and 1 and its incidence in
children is twice as high compared to adults (82). Fortunately, the majority of these
lesions can be surgically removed and provide the young patient
with a good prognosis. Microsurgery, transoral laser microsurgery
(TLM) and endoscopic endonasal approach (EEA) are some of the most
frequent surgical methods of excision. A review of recent studies
dealing with HPV lesions in children revealed only a few cases,
which have been treated surgically. The most common approach of
surgical treatment is using TLM. However, laser treatment can cause
several complications, such as stenosis, burns of the airway tract
and scars. An alternative to TLM are microdebriders (83). Microdebriders provide a more accurate
excision, removing only the affected tissue and preserving the
healthy tissue. The preservation of healthy epithelium is very
useful, when repeated interventions are needed, particularly in
children. When the lesion causes obstruction of the airway tract, a
tracheotomy is necessary to keep the airway open. However, it
should be avoided and performed only when it is an emergency
because of the danger of spreading the disease to the respiratory
tract (84). In the future, the
association between HPV-related lesions in children and cancerous
lesions in adults needs to be considered carefully, revealing the
importance of vaccination in children against HPV (85).
Immunology of infectious mononucleosis
(IM)
IM is the main clinical manifestation of Epstein
Barr virus (EBV) infection (86).
Other agents, such as CMV, toxoplasma and adenovirus, produce a
similar illness. The incubation period ranges from 33 to 49 days
(87). Clinical presentation is
usually prolonged (average 16 days) and ranges from a non-specific
flu-like illness to the more distinctive triad ‘fever, pharyngitis,
lymphadenopathy-splenomegaly’. Other clinical manifestations
include fatigue, hepatitis and eyelid oedema. Possible
complications are meningoencephalitis, haemolytic anaemia,
thrombocytopenia, rash, conjunctivitis, haemophagocytic syndrome,
myocarditis, neurologic diseases, pancreatitis, parotitis,
pericarditis, pneumonitis, psychological disorders and splenic
rupture. Laboratory findings include the elevation of liver enzymes
and lymphocytosis with a marked increase in the number of atypical
lymphocytes in the peripheral blood (87). Additionally, immunophenotypic
alterations of lymphocytes have been described in the various
phases of EBV infection (88). More
specifically, a reduction of B-lymphocytes and an increase in the
number of CD3+CD8+, T-lymphocytes, with a
subsequent decrease in the
CD3+CD4+/CD3+CD8+ ratio
is noted (89).
In the study by Panagopoulou et al (86), which was presented at the Workshop,
researchers aimed to examine whether there is an association
between the immunophenotypic alterations and the variability of the
clinical presentation of IM. Although several studies (89–91) have
examined the immunophenotype of lymphocytes in EBV infection, very
few (89) have correlated these with
the clinical course. The presented study (86) showed that the immunophenotypic
analysis of cytotoxic T cells provides important information on the
physiology of the immune response to EBV infection. Additionally,
it may potentially play a predicting role, providing information on
the expected clinical course, potential complications and the time
to recovery from EBV infection.
Merkel cell polyomavirus (MCPyV): A
novel emerging virus of childhood
MCPyV is a newly-discovered small, human DNA virus,
which causes a widespread, previously unrecognised, human infection
in adulthood and childhood (92,93). It
is classified in the family Polyomaviridae, a group of
non-enveloped, double-stranded DNA viruses with icosahedral
symmetry, which can infect a variety of vertebrates, including
humans and can cause malignant tumours upon their inoculation into
heterologous hosts (94). First
described in January 2008, the prototype sequence of MCPyV has a
5,387 base pair genome and contains the early region, which encodes
the large tumor (LT) antigen and the small tumour (sT) antigen and
the alternative tumor antigen open reading frame (ALTO), the late
region, which encodes VP 1, VP 2 and VP 3 and a non-coding
regulatory region. Of note, the genome of MCPyV has been detected
in approximately 80% of Merkel cell carcinoma (MCC) cases (95). Although MCC is a relatively rare,
highly aggressive, human skin cancer of neuroendocrine origin, its
worldwide incidence has increased over the past twenty years from
500 to 1,500 cases per year. In the majority of MCC cases, MCPyV is
integrated into the host genome in a monoclonal manner and the
viral T antigen has truncating mutations, which render the T
antigen unable to initiate the DNA replication required to
propagate the virus (94).
Recent serological data using enzyme-linked
immunosorbent assay (ELISA) techniques have suggested that MCPyV
infection is common in childhood and occurs during early childhood,
after the disappearance of specific maternal antibodies against
MCPyV (93). MCPyV DNA has been
detected in nasopharyngeal aspirate samples collected from
children, indicating the presence of MCPyV in the upper respiratory
tract of children (96,97). MCPyV is acquired in childhood through
close contact involving saliva and the skin (93). As to date, the mode of MCPyV
transmission has not been fully elucidated, the precise role of the
respiratory secretions in MCPyV transmission in childhood requires
further investigation. The respiratory tract system is involved as
a unique reservoir of MCPyV in children and respiratory secretions
seem to play a significant role in MCPyV transmission in childhood.
Moreover, future studies are required in order to fully elucidate
the potential implications of MCPyV infection in neoplasms in
children.
Acknowledgements
The authors would like to thank all of the chair
persons and the speakers of the Workshop on Paediatric Virology for
their continued support in providing the most up-to-date
information to the symposium. The authors would also like to thank
the participants, who attended the event and provided feedback so
that further study on improving the program can be achieved for the
future. Last but not least, this symposium would not have been
possible without the dedicated hard work and strong commitment from
the Congress Secretary Carol Kalogridis, the members of the PVSG
and the whole symposium organising team for developing the
scientific program, organising, coordinating and guaranteeing the
success of this scientific event.
Glossary
Abbreviations
Abbreviations:
|
AFP
|
acute flaccid paralysis
|
|
AIDS
|
acquired immunodeficiency syndrome
|
|
ALTO
|
alternative tumor antigen open reading
frame
|
|
ASD
|
autism spectrum disorders
|
|
BPD
|
bronchopulmonary dysplasia
|
|
CMV
|
cytomegalovirus
|
|
DNA
|
deoxyribonucleic acid
|
|
EBV
|
Epstein Barr virus
|
|
ED
|
emergency department
|
|
EEA
|
endoscopic endonasal approach
|
|
ELISA
|
enzyme linked immunosorbent assay
|
|
EV
|
Ebola virus
|
|
HBV
|
hepatitis B virus
|
|
HBcAg
|
hepatitis B capsid protein
|
|
HBeAg
|
hepatitis B e antigen
|
|
hMPV
|
human metapneumovirus
|
|
HPV
|
human papillomavirus
|
|
HRV
|
human rhinovirus
|
|
HSV
|
herpes simplex virus
|
|
IM
|
infectious mononucleosis
|
|
IPV
|
inactivated polio vaccine
|
|
LRTI
|
lower respiratory tract infection
|
|
LT
|
large tumor
|
|
MCC
|
Merkel cell carcinoma
|
|
MCPyV
|
Merkel cell polyomavirus
|
|
MMR
|
measles, mumps and rubella
|
|
NCRR
|
non-coding regulatory region
|
|
NICU
|
Neonatal Intensive Care Unit
|
|
OPV
|
oral polio vaccine
|
|
PICU
|
Paediatric Intensive Care Unit
|
|
PPE
|
personal protective equipment
|
|
PVSG
|
Paediatric Virology Study Group
|
|
RCPCH
|
Royal College of Paediatrics and Child
Health
|
|
RNA
|
ribonucleic acid
|
|
RRP
|
recurrent respiratory
papillomatosis
|
|
RSV
|
respiratory syncytial virus
|
|
SARS
|
severe acute respiratory syndrome
|
|
SNP
|
single nucleotide poly-morphism
|
|
sT
|
small tumor
|
|
TLM
|
transoral laser microsurgery
|
|
VP 1–3
|
viral protein 1–3
|
|
VZV
|
varicella-zoster virus
|
|
WHO
|
World Health Organization
|
|
WNV
|
west Nile virus
|
|
WPV
|
wild-type poliovirus
|
References
|
1
|
Shulman ST: The history of pediatric
infectious diseases. Pediatr Res. 55:163–176. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Starr M: Paediatric infectious diseases:
The last 50 years. J Paediatr Child Health. 51:12–15. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Portnoy B: Pediatric Virology. Calif Med.
102:431–445. 1965.PubMed/NCBI
|
|
4
|
Lannon CM and Peterson LE: Pediatric
collaborative networks for quality improvement and research. Acad
Pediatr. 13(Suppl 6): S69–S74. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Theodoridou M: Professional and ethical
responsibilities of health-care workers in regard to vaccinations.
Vaccine. 32:4866–4868. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Stoddard JJ, Cull WL, Jewett EA,
Brotherton SE, Mulvey HJ and Alden ER: Providing pediatric
subspecialty care: A workforce analysis. AAP Committee on Pediatric
Workforce Subcommittee on Subspecialty Workforce. Pediatrics.
106:1325–1333. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Global Pediatric Education Consortium: The
Global Pediatric Education Consortium: Transforming pediatric
training and child health through collaboration. Pediatr Int.
52:684–686. 2010.PubMed/NCBI
|
|
8
|
20th World Congress on Advances in
Oncology and 18th International Symposium on Molecular Medicine.
October 8–10–2015.Athens, Greece: Metropolitan Hotel. http://www.spandidos-publications.com
|
|
9
|
Mammas I, Breen L, Rackham O and Hughes A:
Congenital cytomegalovirus (CMV) infection in twins born by a
CMV-negative mother. Acta Paediatr. 97:2642008.
|
|
10
|
Mammas IN, Sourvinos G and Spandidos DA:
The paediatric story of human papillomavirus (Review). Oncol Lett.
8:502–506. 2014.PubMed/NCBI
|
|
11
|
Greenough A, Drysdale S, Broughton S and
Bont L: The impact of viral infections on the long-term outcomes of
prematurely born infants. Int J Mol Med. 36:S892015.
|
|
12
|
Greenough A, Alexander J, Boit P, Boorman
J, Burgess S, Burke A, Chetcuti PA, Cliff I, Lenney W, Lytle T, et
al: School age outcome of hospitalisation with respiratory
syncytial virus infection of prematurely born infants. Thorax.
64:490–495. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Shefali-Patel D, Paris MA, Watson F,
Peacock JL, Campbell M and Greenough A: RSV hospitalisation and
healthcare utilisation in moderately prematurely born infants. Eur
J Pediatr. 171:1055–1061. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Broughton S, Roberts A, Fox G, Pollina E,
Zuckerman M, Chaudhry S and Greenough A: Prospective study of
healthcare utilisation and respiratory morbidity due to RSV
infection in prematurely born infants. Thorax. 60:1039–1044. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Drysdale SB, Lo J, Prendergast M, Alcazar
M, Wilson T, Zuckerman M, Smith M, Broughton S, Rafferty GF,
Peacock JL, et al: Lung function of preterm infants before and
after viral infections. Eur J Pediatr. 173:1497–1504. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Drysdale SB, Alcazar-Paris M, Wilson T,
Smith M, Zuckerman M, Peacock JL, Johnston SL and Greenough A:
Viral lower respiratory tract infections and preterm infants'
healthcare utilisation. Eur J Pediatr. 174:209–215. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Drysdale SB, Wilson T, Alcazar M,
Broughton S, Zuckerman M, Smith M, Rafferty GF, Johnston SL and
Greenough A: Lung function prior to viral lower respiratory tract
infections in prematurely born infants. Thorax. 66:468–473. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Drysdale SB, Prendergast M, Alcazar M,
Wilson T, Smith M, Zuckerman M, Broughton S, Rafferty GF, Johnston
SL, Hodemaekers HM, et al: Genetic predisposition of RSV
infection-related respiratory morbidity in preterm infants. Eur J
Pediatr. 173:905–912. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Drysdale SB, Alcazar-Paris M, Wilson T,
Smith M, Zuckerman M, Broughton S, Rafferty GF, Peacock JL,
Johnston SL and Greenough A: Rhinovirus infection and healthcare
utilisation in prematurely born infants. Eur Respir J.
42:1029–1036. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Theodoridou M: Defeating polio: Vaccine
anniversary (1955–2015). Int J Mol Med. 36:S892015.
|
|
21
|
WHO: Polio vaccines: WHO position paper,
January 2014 - recommendations. Vaccine. 32:4117–4118. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
European Centre for Disease Prevention and
control: Risk assessment: Wild-type poliovirus 1 transmission in
Israel - what is the risk to the EU/EEA? ECDC (Stockholm).
2013.
|
|
23
|
European Centre for Disease Prevention and
Control: Rapid risk assessment: Suspected outbreak of poliomyelitis
in Syria: Risk of importation and spread of poliovirus in the EU.
ECDC (Stockholm). 2013.
|
|
24
|
Global Polio Eradication Initiative: Data
and monitoring. http://www.polioeradication.org
|
|
25
|
Porter KA, Diop OM, Burns CC, Tangermann
RH and Wassilak SG: Tracking progress toward polio eradication -
worldwide. 2013–2014. MMWR Morb Mortal Wkly Rep. 64:415–420.
2015.PubMed/NCBI
|
|
26
|
Orenstein WA: Committee on Infectious
Diseases: Eradicating polio: how the world's pediatricians can help
stop this crippling illness forever. Pediatrics. 135:196–202. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Kramvis A: The clinical implications of
hepatitis B virus genotypes in Paediatrics. Int J Mol Med.
36:S892015.
|
|
28
|
World Health Organization: Hepatitis B.
Fact sheet No. 204. Updated. July;2015.http://www.who.int/mediacentre/factsheets/fs204/en/
|
|
29
|
Ni YH: Natural history of hepatitis B
virus infection: pediatric perspective. J Gastroenterol. 46:1–8.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Lok AS and McMahon BJ: Chronic hepatitis
B. Hepatology. 45:507–539. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Milich D and Liang TJ: Exploring the
biological basis of hepatitis B e antigen in hepatitis B virus
infection. Hepatology. 38:1075–1086. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Hsu HY, Chang MH, Hsieh KH, Lee CY, Lin
HH, Hwang LH, Chen PJ and Chen DS: Cellular immune response to
HBcAg in mother-to-infant transmission of hepatitis B virus.
Hepatology. 15:770–776. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Chen M, Sällberg M, Hughes J, Jones J,
Guidotti LG, Chisari FV, Billaud JN and Milich DR: Immune tolerance
split between hepatitis B virus precore and core proteins. J Virol.
79:3016–3027. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Beasley RP, Trepo C, Stevens CE and
Szmuness W: The e antigen and vertical transmission of hepatitis B
surface antigen. Am J Epidemiol. 105:94–98. 1977.PubMed/NCBI
|
|
35
|
Okada K, Kamiyama I, Inomata M, Imai M,
Miyakawa Y and Mayumi M: e antigen and anti-e in the serum of
asymptomatic carrier mothers as indicators of positive and negative
transmission of hepatitis B virus to their infants. N Engl J Med.
294:746–749. 1976. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Tong MJ, Thursby MW, Lin JH, Weissman JY
and McPeak CM: Studies on the maternal-infant transmission of the
hepatitis B virus and HBV infection within families. Prog Med
Virol. 27:137–147. 1981.PubMed/NCBI
|
|
37
|
Kramvis A: Genotypes and genetic
variability of hepatitis B virus. Intervirology. 57:141–150. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Mammas IN, Sourvinos G, Theodoridou M and
Spandidos DA: Understanding the factors affecting human
papillomavirus vaccination acceptance among adolescents. Int J Mol
Med. 36:S902015.
|
|
39
|
Mammas IN and Spandidos DA: George N.
Papanicolaou (1883–1962): Fifty years after the death of a great
doctor, scientist and humanitarian. J BUON. 17:180–184.
2012.PubMed/NCBI
|
|
40
|
Tota JE, Chevarie-Davis M, Richardson LA,
Devries M and Franco EL: Epidemiology and burden of HPV infection
and related diseases: Implications for prevention strategies. Prev
Med. 53(Suppl 1): S12–S21. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
zur Hausen H: Papillomaviruses and cancer:
From basic studies to clinical application. Nat Rev Cancer.
2:342–350. 2002. View
Article : Google Scholar : PubMed/NCBI
|
|
42
|
Kahn JA: HPV vaccination for the
prevention of cervical intraepithelial neoplasia. N Engl J Med.
361:271–278. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Fagot JP, Boutrelle A, Ricordeau P, Weill
A and Allemand H: HPV vaccination in France: uptake, costs and
issues for the National Health Insurance. Vaccine. 29:3610–3616.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Deleré Y, Böhmer MM, Walter D and Wichmann
O: HPV vaccination coverage among women aged 18–20 years in Germany
three years after recommendation of HPV vaccination for adolescent
girls: results from a cross-sectional survey. Hum Vaccin
Immunother. 9:1706–1711. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Steens A, Wielders CC, Bogaards JA,
Boshuizen HC, de Greeff SC and de Melker HE: Association between
human papillomavirus vaccine uptake and cervical cancer screening
in the Netherlands: Implications for future impact on prevention.
Int J Cancer. 132:932–943. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Fisher H, Audrey S, Mytton JA, Hickman M
and Trotter C: Examining inequalities in the uptake of the
school-based HPV vaccination programme in England: a retrospective
cohort study. J Public Health (Oxf). 36:36–45. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Vandoros S, Hessel P, Leone T and Avendano
M: Have health trends worsened in Greece as a result of the
financial crisis? A quasi-experimental approach. Eur J Public
Health. 23:727–731. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Christaki I, Beattie T and Midgley P: The
challenge of modern biowarfare: ED preparedness for paediatric
victims of the Ebola virus. Int J Mol Med. 36:S902015.
|
|
49
|
Elshabrawy HA, Erickson TB and Prabhakar
BS: Ebola virus outbreak, updates on current therapeutic
strategies. Rev Med Virol. 25:241–253. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Venkat A, Asher SL, Wolf L, et al:
American College of Emergency Physicians; Emergency Nurses
Association; Society for Academic Emergency Medicine: Ethical
issues in the response to Ebola virus disease in United States
emergency departments: A position paper of the American College of
Emergency Physicians, the Emergency Nurses Association, and the
Society for Academic Emergency Medicine. Acad Emerg Med.
22:605–615. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Bogucki S and Isakov A: Patients under
investigation for Ebola virus disease in the United States:
hospital preparedness planning and alternate care facilities. Acad
Emerg Med. 22:600–604. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Mackway-Jones K, Carley SD and Robson J:
Planning for major incidents involving children by implementing a
Delphi study. Arch Dis Child. 80:410–413. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Richardson KJ: Ebola virus disease. Adv
Emerg Nurs J. 37:102–115. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Koutsaftiki C: The clinical profile of
infants with RSV bronchiolitis in PICU. Int J Mol Med.
36:S902015.
|
|
55
|
Koutsaftiki C, Tsialla A, Sideri G,
Bampanelou A, Papadatos I and Sianidou L: Management of infants
with severe bronchiolitis who were admitted to two PICUs. Int J Mol
Med. 36:S912015.
|
|
56
|
Bamberger E, Srugo I, Raya Abu B, Segal E,
Chaim B, Kassis I, Kugelman A and Miron D: What is the clinical
relevance of respiratory syncytial virus bronchiolitis?: Findings
from a multi-center, prospective study. Eur J Clin Microbiol Infect
Dis. 31:3323–3330. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Eggleston HA, Gunville CF, Miller JI,
Sontag MK and Mourani PM: A comparison of characteristics and
outcomes in severe human metapneumovirus and respiratory syncytial
virus infections in children treated in an intensive care unit.
Pediatr Infect Dis J. 32:1330–1334. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Hasegawa K, Pate BM, Mansbach JM, Macias
CG, Fisher ES, Piedra PA, Espinola JA, Sullivan AF and Camargo CA
Jr: Risk factors for requiring intensive care among children
admitted to ward with bronchiolitis. Acad Pediatr. 15:77–81. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Ralston SL, Lieberthal AS, Meissner HC, et
al: Clinical practice guideline: the diagnosis, management, and
prevention of bronchiolitis. Pediatrics. 134:e1474–e1502. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Koutsaki M: MMR vaccination and autism: An
update. Int J Mol Med. 36:S912015.
|
|
61
|
Rapin I and Tuchman RF: Autism:
Definition, neurobiology, screening, diagnosis. Pediatr Clin North
Am. 551129–1146. (viii)2008. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Wakefield AJ, Murch SH, Anthony A, Linnell
J, Casson DM, Malik M, Berelowitz M, Dhillon AP, Thomson MA, Harvey
P, et al: Ileal-lymphoid-nodular hyperplasia, non-specific colitis,
and pervasive developmental disorder in children. Lancet.
351:637–641. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Piccirilli G, Lazzarotto T, Chiereghin A,
Serra L, Gabrielli L and Lanari M: Spotlight on measles in Italy:
why outbreaks of a vaccine-preventable infection continue in the
21st century. Expert Rev Anti Infect Ther. 13:355–362. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Maillet M, Bouvat E, Robert N,
Baccard-Longère M, Morel-Baccard C, Morand P, Vabret A and Stahl
JP: Mumps outbreak and laboratory diagnosis. J Clin Virol.
62:14–19. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Pegorie M, Shankar K, Welfare WS, Wilson
RW, Khiroya C, Munslow G, Fiefield D, Bothra V and McCann R:
Measles outbreak in Greater Manchester, England, October 2012 to
September 2013: epidemiology and control. Euro Surveill. 19(pii):
209822014. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Ryu JU, Kim EK, Youn YS, Rhim JW and Lee
KY: Outbreaks of mumps: An observational study over two decades in
a single hospital in Korea. Korean J Pediatr. 57:396–402. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Centers for Disease Control and Prevention
(CDC): Nationwide rubella epidemic - Japan. 2013. MMWR Morb Mortal
Wkly Rep. 62:457–462. 2013.PubMed/NCBI
|
|
68
|
Gahr P, DeVries AS, Wallace G, et al: An
outbreak of measles in an undervaccinated community. Pediatrics.
134:e220–e228. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Kutty PK, Lawler J, Rausch-Phung E, et al:
Epidemiology and the economic assessment of a mumps outbreak in a
highly vaccinated population, Orange County, New York. 2009–2010.
Hum Vaccin Immunother. 10:1373–1381. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Jain A, Marshall J, Buikema A, Bancroft T,
Kelly JP and Newschaffer CJ: Autism occurrence by MMR vaccine
status among US children with older siblings with and without
autism. JAMA. 313:1534–1540. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Uno Y, Uchiyama T, Kurosawa M, Aleksic B
and Ozaki N: Early exposure to the combined measles-mumps-rubella
vaccine and thimerosal-containing vaccines and risk of autism
spectrum disorder. Vaccine. 33:2511–2516. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Taylor LE, Swerdfeger AL and Eslick GD:
Vaccines are not associated with autism: An evidence-based
meta-analysis of case-control and cohort studies. Vaccine.
32:3623–3629. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Portaliou D: Ocular viral infections in
neonates and children. Int J Mol Med. 36:S912015.
|
|
74
|
Matoba A: Ocular viral infections. Pediatr
Infect Dis. 3:358–368. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Corey L and Wald A: Maternal and neonatal
herpes simplex virus infections. N Engl J Med. 361:1376–1385. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Sanders JE and Garcia SE: Pediatric herpes
simplex virus infections: an evidence-based approach to treatment.
Pediatr Emerg Med Pract. 11:1–19; quiz 19. 2014.PubMed/NCBI
|
|
77
|
Fong CY, Aye AM, Peyman M, Nor NK,
Visvaraja S, Tajunisah I and Ong LC: Neonatal herpes simplex virus
type-1 central nervous system disease with acute retinal necrosis.
Pediatr Infect Dis J. 33:424–426. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Modrzejewska M, Lachowicz E, Karczewicz D
and Zdanowska A: Chorioretinitis in infants. Klin Oczna.
113:352–356. 2011.PubMed/NCBI
|
|
79
|
Kostagianni G: HPV infections in children:
Current surgical treatment of HPV lesions found in the oral cavity,
oropharynx, larynx and nose cavity. Int J Mol Med. 36:S902015.
|
|
80
|
Marur S, D'Souza G, Westra WH and
Forastiere AA: HPV-associated head and neck cancer: a virus-related
cancer epidemic. Lancet Oncol. 11:781–789. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Krüger M, Pabst AM, Walter C, Sagheb K,
Günther C, Blatt S, Weise K, Al-Nawas B and Ziebart T: The
prevalence of human papilloma virus (HPV) infections in oral
squamous cell carcinomas: a retrospective analysis of 88 patients
and literature overview. J Craniomaxillofac Surg. 42:1506–1514.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Summersgill KF, Smith EM, Levy BT, Allen
JM, Haugen TH and Turek LP: Human papillomavirus in the oral
cavities of children and adolescents. Oral Surg Oral Med Oral
Pathol Oral Radiol Endod. 91:62–69. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Stamataki S, Nikolopoulos TP, Korres S,
Felekis D, Tzangaroulakis A and Ferekidis E: Juvenile recurrent
respiratory papillomatosis: still a mystery disease with difficult
management. Head Neck. 29:155–162. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Carifi M, Napolitano D, Morandi M and
Dall'Olio D: Recurrent respiratory papillomatosis: Current and
future perspectives. Ther Clin Risk Manag. 11:731–738. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Wierzbicka M, Józefiak A, Jackowska J,
Szydłowski J and Goździcka-Józefiak A: HPV vaccination in head and
neck HPV-related pathologies. Otolaryngol Pol. 68:157–173. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Panagopoulou P, Fleva A,
Papadopoulou-Alataki E, Pavlitou-Tsiontsi A and
Emporiadou-Petikopoulou M: Correlation between the clinical course
and the immunophenotypic profile of T-cytotoxic lymphocytes in
children with infectious mononucleosis. Int J Mol Med.
36:S922015.
|
|
87
|
Odumade OA, Hogquist KA and Balfour HH Jr:
Progress and problems in understanding and managing primary
Epstein-Barr virus infections. Clin Microbiol Rev. 24:193–209.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Scherrenburg J, Piriou ER, Nanlohy NM and
van Baarle D: Detailed analysis of Epstein-Barr virus-specific CD4+
and CD8+ T cell responses during infectious mononucleosis. Clin Exp
Immunol. 153:231–239. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Papadopoulou-Alataki E, Fleva A, Antari V,
Pavlitou-Tsiontsi A, Moskofidis M and Varlamis G: Study of the
immunophenotype of peripheral blood lymphocyte subsets in children
with Epstein-Barr virus and cytomegalovirus infection: Association
with outcome. Paidiatriki. 71:135–140. 2008.
|
|
90
|
Hamann D, Baars PA, Rep MH, Hooibrink B,
Kerkhof-Garde SR, Klein MR and van Lier RA: Phenotypic and
functional separation of memory and effector human CD8+ T cells. J
Exp Med. 186:1407–1418. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Hudnall SD, Patel J, Schwab H and Martinez
J: Comparative immunophenotypic features of EBV-positive and
EBV-negative atypical lymphocytosis. Cytometry B Clin Cytom.
55:22–28. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Sourvinos G, Mammas IN and Spandidos DA:
Merkel cell polyomavirus (MCPyV): A novel emerging virus of infancy
and childhood. Int J Mol Med. 36:S912015.
|
|
93
|
Sourvinos G, Mammas IN and Spandidos DA:
Merkel cell polyomavirus infection in childhood: current advances
and perspectives. Arch Virol. 160:887–892. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
zur Hausen H: Novel human polyomaviruses -
re-emergence of a well known virus family as possible human
carcinogens. Int J Cancer. 123:247–250. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Ehlers B and Wieland U: The novel human
polyomaviruses HPyV6, 7, 9 and beyond. APMIS. 121:783–795. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Goh S, Lindau C, Tiveljung-Lindell A and
Allander T: Merkel cell polyomavirus in respiratory tract
secretions. Emerg Infect Dis. 15:489–491. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Abedi Kiasari B, Vallely PJ and Klapper
PE: Merkel cell polyomavirus DNA in immunocompetent and
immunocompromised patients with respiratory disease. J Med Virol.
83:2220–2224. 2011. View Article : Google Scholar : PubMed/NCBI
|