Introduction
Kimura's disease (KD), a chronic inflammatory
disease characterized by slowly growing subcutaneous nodules and
benign reactive lymphoid proliferation in the face and neck region
is predominantly observed in young Asian men (1). It is considered to be a benign disease
involving subcutaneous tissues, major salivary glands and lymph
nodes in the area of head and neck (2). Although numerous researchers have
conducted investigations into the etiology of KD (3–5), reports
concerning the underlying etiology of KD in oral and maxillofacial
areas are limited (6). Until
recently, the underlying cause of KD was unknown (7) In addition, the diagnosis of KD prior to
surgery has proven challenging, since a clinical examination alone
may not give an accurate diagnosis (8). In the present study, a case of KD
affecting the oral and maxillofacial areas was evaluated and the
corresponding pathogenesis was reported.
Case report
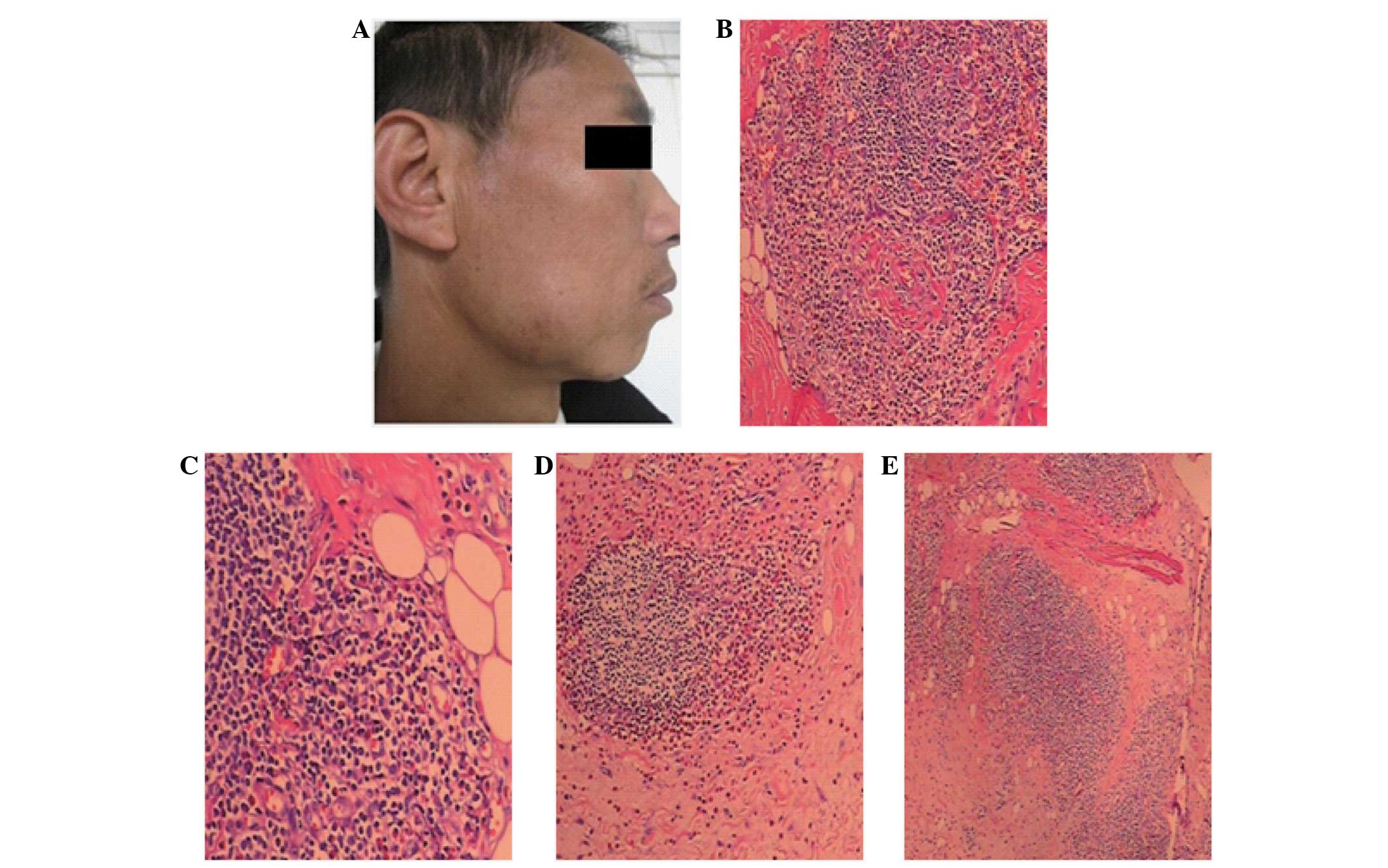
The patient in the present case was an otherwise
healthy 39-year-old man. The patient was admitted to the Shanghai
East Hospital Affiliated with Tongji University (Shanghai, China)
in October 2011 with an obvious swelling on his right cheek
(Fig. 1A). The patient had a 2-year
history of non-painful swelling of the right-side cheek without
additional symptoms. Three weeks prior to presentation, the patient
sought medical attention and self-treated with an anti-bacterial
agent administered orally (the name and dose of the drug are
unknown). After a 3-week treatment, the mass only minimally
responded to over-the-counter medication and no improvement in the
patient's condition was exhibited. Therefore, the patient was
referred to our hospital for further evaluation and treatment.
According to the investigation conducted at the hospital, there was
no history of recent febrile illness, pharyngitis, cough, rash or
diarrhea and the patient had never received blood or blood
products. Furthermore, the patient was not addicted to smoking or
drinking. As a public servant, he had no occupational exposures and
lived with his wife and daughter.
According to the results of a physical examination,
the patient was in a healthy condition with a body temperature of
36.8°C, blood pressure of 127/85 mmHg and heart rate of 80 beats
per minute. The swelling, located in the subcutaneous tissue, was
firm and non-tender with ill-defined margins and measured ~7×5
cm2. The lesion was clearly observed to be both intra-
and extra-oral without attachment to the right mandible. No signs
of inflammation were identified in the stretched adjoining oral
mucosa and overlying skin. The parotid salivary ducts were detected
to be normal and the enlarged lymph nodes were identified as
inconspicuous swellings in the submandibular or upper cervical
regions. Surgical excision was performed and the formation of a
lymphoid nodule was discovered surrounding the fibers between the
endoplasm. Microscopic observation with hematoxylin and eosin
staining revealed eosinophilic infiltration accompanied by the
intense proliferation of small blood vessels and eosinophils and
thickened cell walls (Fig. 1B–D). In
addition, the fat and fibrous tissues exhibited spotty lymphocytic
infiltration (Fig. 1E). These
histopathological features provide an insight into KD in the oral
and maxillofacial areas, which may serve as a reference in its
diagnosis.
A follow-up interview by telephone was carried out
once a year after this patient left the hospital and 3 years later,
the patient reported no recurrence of the mass or subjective
symptoms. Informed consent was obtained from the patient for the
publication of this report.
Discussion
KD presents as a benign tumor-like lesion or cyst,
which may be removed by a surgical procedure (9). The diagnosis of KD can be based on
characteristic findings following surgical excision in conjunction
with peripheral eosinophilia and elevated serum immunoglobulin E
(IgE) levels (10). In a review of
several cases, no clear conclusions were made regarding the cause
of KD (11), and computed tomography
and magnetic resonance imaging examinations exhibited no specific
intensity or signal changes (10).
Clinically, KD is typically diagnosed by oral and maxillofacial
surgeons when a patient has suffered from a long history of a mass
with blood eosinophilia and increased serum IgE levels, and
presents with single or multiple painless subcutaneous masses
(12). In addition, the confirmation
of the characteristic distribution morphology with lymphadenopathy,
in combination with the clinical features and laboratory
examination, enables a confident preoperative diagnosis of KD
(13). Despite various efforts to
establish a definitive treatment for KD, none has yet been
identified. The usual methods of treatment include observation,
drug administration (14,15), immunosuppressive therapy including
tacrolimus (FK-506) (16),
radiotherapy (17,18), surgical excision (19) and photodynamic therapy (20). Among them, surgical excision is
considered the most effective as it provides not only a treatment
for AD, but also a sample for histopathological investigations in
order to facilitate an accurate diagnosis (19).
Although nonspecific, the results of
histopathological analyses are considered able to eliminate the
occurrence of malignancies in the differential diagnosis of KD
(19). Typically, a
histopathological examination is performed before a definitive
diagnosis is made (21). In the
present case, a histopathological examination of the diseased
tissue was conducted in order to investigate the potential
diagnosis of KD affecting the oral and maxillofacial areas. The
examination revealed vigorous proliferation of vasculature and
lymphocytic infiltration enriched with eosinophils, which may be
considered as the gold standard for KD diagnosis.
The recurrence of disease is affected by various
factors, including disease duration time, lesion diameter, blood
eosinophil count, well-defined lesion boundaries, serum IgE levels
and single or multiple lesions (22). In the current case, a single
ill-defined lesion was exhibited, which was >5 cm in diameter.
However, no sign of recurrence of the mass has yet been observed on
the basis of the telephone follow-up interviews, although a
measurement of possible recurrence (i.e. a pathological
examination) should be performed in order to further address the
prognosis of the patient.
References
|
1
|
Lee J and Hong YS: Kimura disease
complicated with bowel infarction and multiple arterial thromboses
in the extremities. J Clin Rheumatol. 20:38–41. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Shehwaro N, Langlois AL, Gueutin V, Debchi
L, Charlotte F, Rouvier P, Rottembourg J and Izzedine H: Kimura's
disease: An unrecognized cause of adult-onset nephrotic syndrome
with minimal change disease. Nephrol Ther. 10:46–50. 2014.(In
French). View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Reddy PKS, Prasad ALS, Sumathy TK,
Shivaswamy KN and Ranganathan C: An Overlap of Angiolymphoid
Hyperplasia with Eosinophilia and Kimura's Disease: Successful
Treatment of Skin Lesions with Cryotherapy. Indian J Dermatol.
60:2162015.PubMed/NCBI
|
|
4
|
Sah P, Kamath A, Aramanadka C and
Radhakrishnan R: Kimura's disease - An unusual presentation
involving subcutaneous tissue, parotid gland and lymph node. J Oral
Maxillofac Pathol. 17:455–459. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
O'Malley DP and Grimm KE: Reactive
lymphadenopathies that mimic lymphoma: Entities of unknown
etiology. Semin Diagn Pathol. 30:137–145. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kapoor NS, O'Neill JP, Katabi N, Wong RJ
and Shah JP: Kimura disease: Diagnostic challenges and clinical
management. Am J Otolaryngol. 33:259–262. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Koh H, Kamiishi N, Chiyotani A, Takahashi
H, Sudo A, Masuda Y, Shinden S, Tajima A, Kimura Y and Kimura T:
Eosinophilic lung disease complicated by Kimura's disease: A case
report and literature review. Intern Med. 51:3163–3167. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Dai L, Wei XN, Zheng DH, Mo YQ, Pessler F
and Zhang BY: Effective treatment of Kimura's disease with
leflunomide in combination with glucocorticoids. Clin Rheumatol.
30:859–865. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Shetty AK, Beaty MW, McGuirt WF Jr, Woods
CR and Givner LB: Kimura's disease: A diagnostic challenge.
Pediatrics. 110:e392002. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zhang R, Ban XH, Mo YX, Lv MM, Duan XH,
Shen J, Li JP, Liu XW and Xie CM: Kimura's disease: The CT and MRI
characteristics in fifteen cases. Eur J Radiol. 80:489–497. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Punia RP, Aulakh R, Garg S, Chopra R,
Mohan H and Dalal A: Kimura's disease: Clinicopathological study of
eight cases. J Laryngol Otol. 127:170–174. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Guimaraes CS, Moulton-Levy N, Sapadin A
and Vidal C: Kimura's Disease. Case Rep Med.
2009:4240532009.PubMed/NCBI
|
|
13
|
Steiner D, Tudge S, Thomson P and McLean
C: Kimuras disease: An unusual cause of neck mass. ANZ J Surg.
76:866–868. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Takeishi M, Makino Y, Nishioka H, Miyawaki
T and Kurihara K: Kimura disease: Diagnostic imaging findings and
surgical treatment. J Craniofac Surg. 18:1062–1067. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Xu X, Fu J, Fang Y and Liang L: Kimura
disease in children: A case report and a summary of the literature
in Chinese. J Pediatr Hematol Oncol. 33:306–311. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Shu DL, Ran W, Guo B, Zhang YY, Liu XZ and
Liao X: Tacrolimus on Kimura's disease: A case report. Oral Surg
Oral Med Oral Pathol Oral Radiol. 117:e74–e78. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Wang Z, Zhang J, Ren Y, Dai Z, Ma H, Cui
D, Su X and Song SJ: Successful treatment of recurrent Kimura's
disease with radiotherapy: A case report. Int J Clin Exp Pathol.
7:4519–4522. 2014.PubMed/NCBI
|
|
18
|
Monzen Y, Kiya K and Nishisaka T: Kimura's
Disease of the Orbit Successfully Treated with Radiotherapy Alone:
A Case Report. Case Rep Ophthalmol. 5:87–91. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Milentijeví MJ, Basić M and Petrović A:
Kimura's disease in a young Balkan male. Vojnosanit Pregl.
66:66–68. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Abbas S, Jerjes W, Upile T, Vincent A and
Hopper C: Treatment of Kimura disease with photodynamic therapy: A
case study. Photodiagnosis Photodyn Ther. 9:83–86. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Uysal IO, Eryilmaz MA, Salk I and
Abasiyanik F: Kimura disease in the parotid gland. J Craniofac
Surg. 22:337–338. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Lin YY, Jung SM, Ko SF, Toh CH, Wong AM,
Chen YR, Chan SC, Cheung YC and Ng SH: Kimura's disease: Clinical
and imaging parameters for the prediction of disease recurrence.
Clin Imaging. 36:272–278. 2012. View Article : Google Scholar : PubMed/NCBI
|