Introduction
Cystic meningioma is a relatively rare condition
with incidence rates ranging between 1.7 and 10% worldwide
(1–5). While meningiomas are considered more
likely to appear in females, no substantial difference was
identified in the incidence rates between the two genders,
according to an analysis of 166 cases of cystic meningioma
(2). The clinical manifestation of
cystic meningioma include, but are not limited to: Headache,
seizure, dizziness, personality changes and motor disturbance
(1–10). Surgical removal of the entire tumor
and its cyst remains the predominant treatment for cystic
meningioma (1–10). Cystic meningioma may pose a
diagnostic dilemma preoperatively, since it is occasionally
difficult to differentiate among glioma, hemangioblastoma,
craniopharyngioma and metastatic brain tumor (6–10). The
accuracy of the diagnosis of cystic meningioma based on the results
of magnetic resonance imaging (MRI) has been reported to be 78%
preoperatively (4). The present
study reported two cases of benign meningioma with a large cyst,
which presented with a peritumoral cyst with neoplastic cells on
the cystic wall.
Case report
Case 1
A 57-year-old male patient presented at the Beijing
Sanbo Brain Hospital (Beijing, China) on November 2nd
2013 with a left-sided hemiparesis that persisted for 11 months,
which was accompanied by a headache lasting 3 days prior to
admission. A neurological examination was completed which revealed
clouding of consciousness, speech disturbance, decreased left-side
distal muscle strength (grade 0) and proximal muscle strength
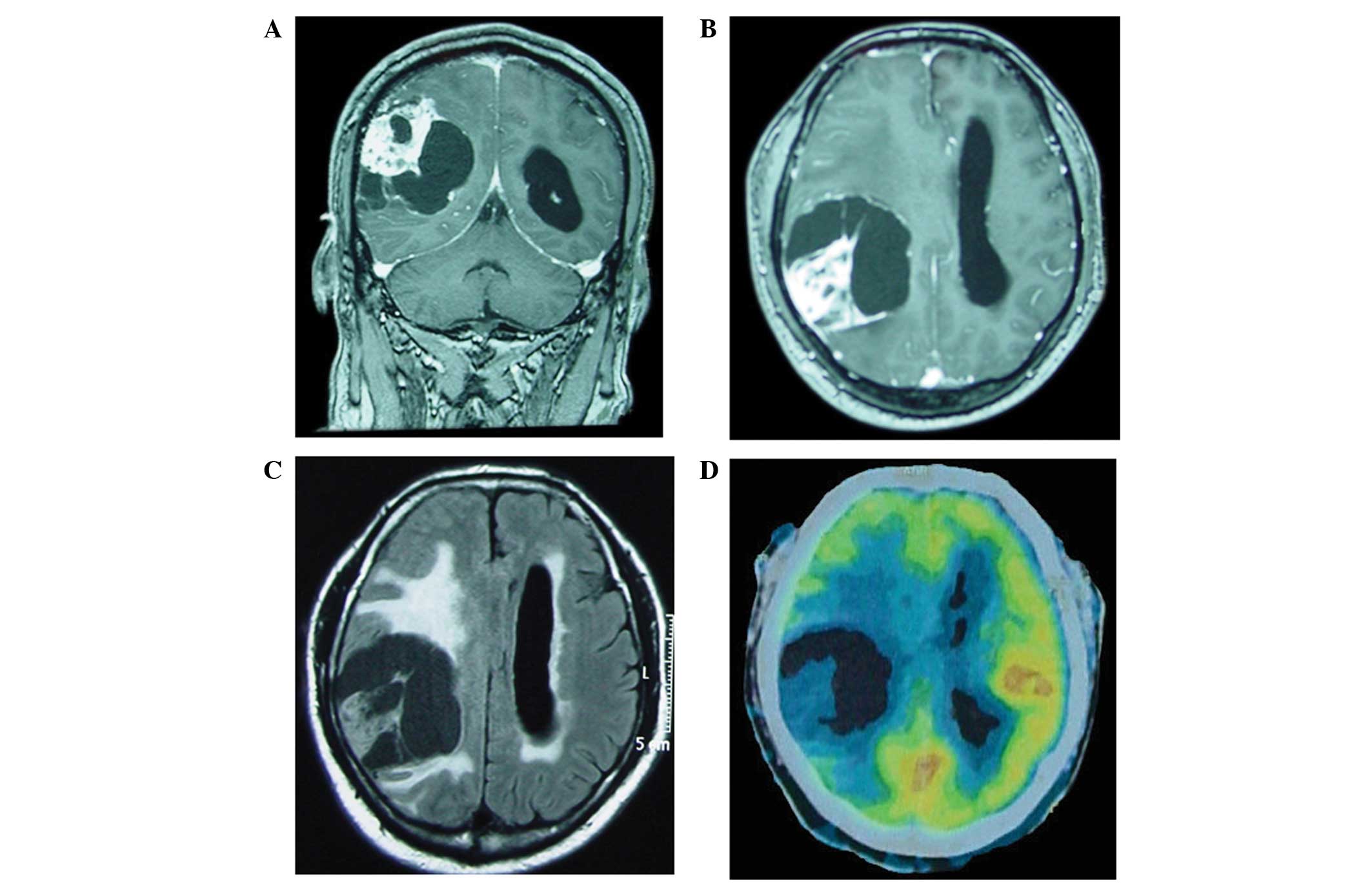
(grade III), according to the WHO classification (11). A contrast-enhanced MRI scan (Fig. 1A and B) was performed using 10 ml
gadolinium-diethylenetriaminepentaacetic acid (Bayer AG, Leverkusen
Germany) and reported according to previous studies (12,13). The
MRI scan revealed a large, homogeneously enhancing lesion with
multiple cysts with wall enhancement in the right hemisphere. The
midline was found to be markedly shifted and the left lateral
ventricle was dilated. The solid tumor parts and the cystic wall
were also found to be enhanced. The tumor measured 5.7×6.2×7.0 cm
and was surrounded by edema (Fig.
1C). A 2-deoxy-2-[18F]-fluoro-D-glucose positron emission
tomography/computed tomography scan revealed a slightly increased
metabolism in the solid components of the tumor and the maximum
standardized uptake value was 2.4 (Fig.
1D). Based on the clinical manifestations and the imaging
results, glioma was diagnosed and surgery was performed to remove
the tumor.
During surgery, a tumor was found within the cyst,
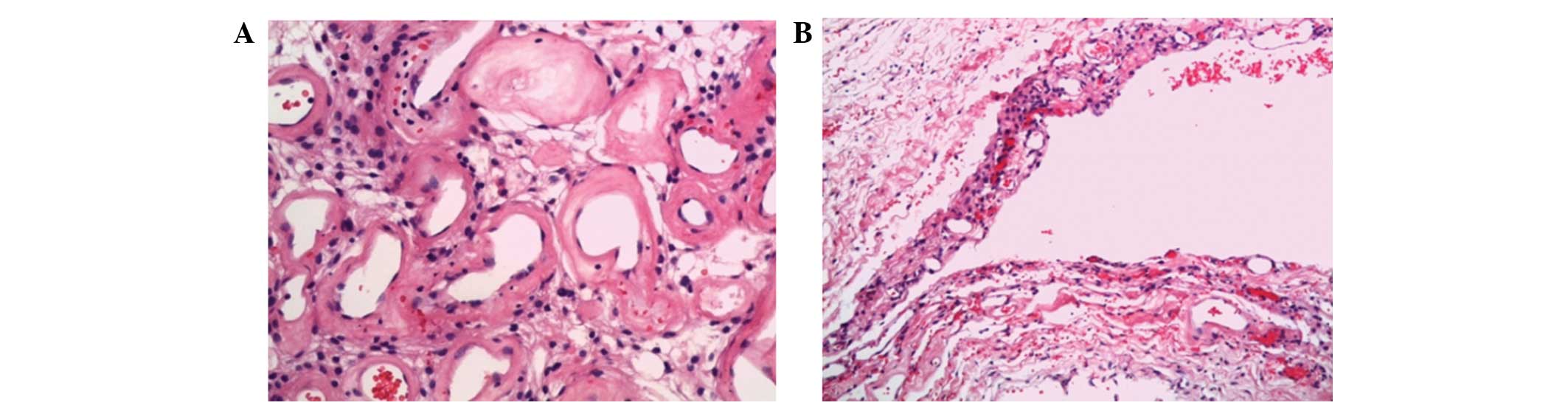
along with multiple other cysts within the tumor. Histological
examination demonstrated that the tumor was of the angiomatous type
with hyaline degeneration of the vessel wall (Fig. 2). Biopsy of the cystic wall revealed
gliosis and presence of tumor cells (Fig. 2). This configuration was classified
as a peritumoral cystic meningioma with neoplastic cells on the
cystic wall.
The patient did not receive further medical
treatment following the operation. An MRI scan was performed 3
months postoperatively without any evidence of tumor. The patient
was followed up on November 1st 2015 via telephone, he is in good
health with the exception that his left finger is not as flexible
as it previously has been. Written informed consent was obtained
from the patient.
Case 2
A 29-year old male patient presented at the Beijing
Sanbo Brain Hospital on November 12th 2013 with urinary
incontinence and memory decline for 2 months. A neurological
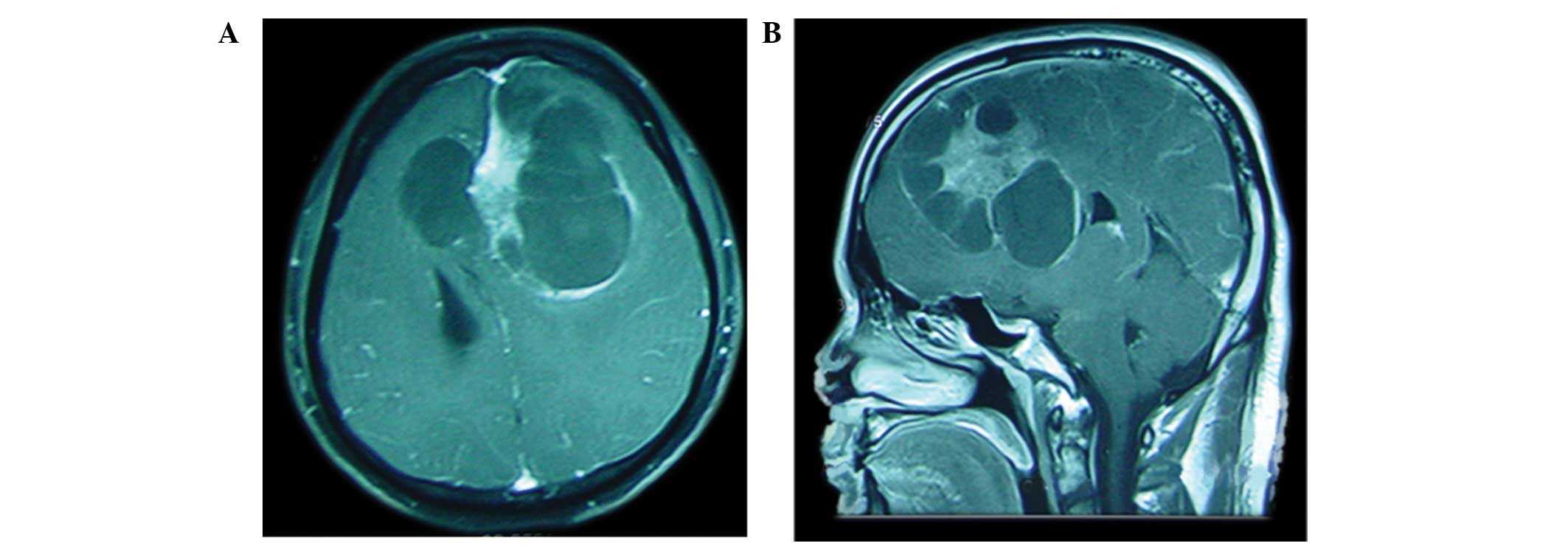
examination showed no deficits. MRI scans revealed an enhancing
frontal solid mass with multiple well-circumscribed peritumoral
cysts with an irregularly enhancing wall (Fig. 3). Based on the clinical
manifestations and the imaging results, glioma was diagnosed and
surgery was performed to remove the tumor.
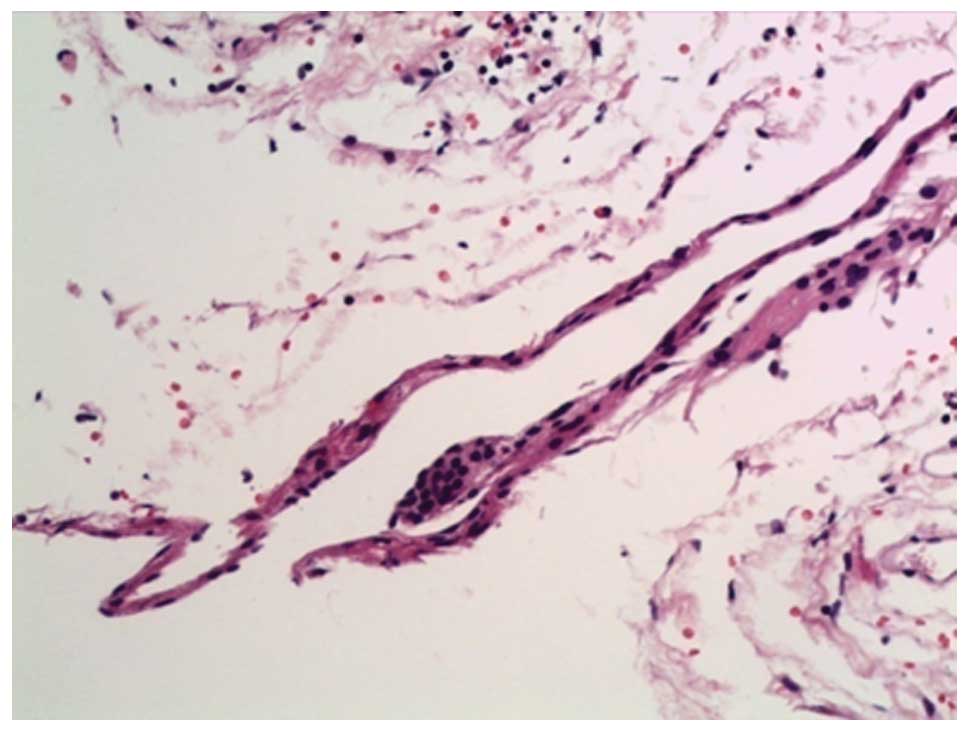
During surgery, the tumor nodule was found to be
surrounded by several closely applied cysts and multiple biopsies
of the cystic wall revealed the presence of tumor cells.
Histopathological analysis showed that the tumor was a
meningothelial meningioma that exhibited partly active
proliferation, and was classified as a grade II tumor according to
the World Health Organization classification (11). Necrosis, calcification, mitosis and
reactive gliosis were also observed. Biopsy of the cystic wall
demonstrated that it was composed of fibrous tissue and tumor cell
nests (Fig. 4). The final diagnosis
was peritumoral cystic meningioma with tumor invasion on the cystic
wall.
The patient received one dose of radiotherapy
following the operation. An MRI was performed in July 2015 and no
tumors were detected. The patient was followed up on November 1st
2015 via telephone, he is in good health and is able to work and
exercise as before. Written informed consent was obtained from the
patient.
Discussion
The most common site for the appearance of cystic
meningiomas is the cerebral convexity, particularly the frontal and
parietal lobes, while the cerebral falx is the second most frequent
location (2). Furthermore, cystic
meningiomas can also be identified in the cerebellopontine angle,
olfactory groove, suprasellar, falx and ventricle, olfactory groove
trigeminal nerve or optic nerve (3,5,6,14–19). The
most frequent histological subtype has been found to be the
meningothelial subtype (2,5,20).
Notably, atypical meningiomas have the tendency to form a cyst, as
opposed to other subtypes of meningioma (17,20).
Rengachary et al (21) recognized two types of cystic
meningioma, including the intratumoral and peritumoral cystic
meningiomas. Nauta et al (22) subdivided these two types according to
the association between the tumor, associated cysts and the
surrounding brains, as follows: Type I, which has a central cyst;
type II, which has a peripheral intratumoral cyst; type III, which
has a peritumoral cyst that lies within the adjacent brain region;
and type IV, which has a peritumoral cyst at the interface of the
tumor and brain. Worthington et al (23) then added a fifth type to the Nauta
classification: Type V, in which the cysts enclosed the tumor
nodule with the neoplastic cells on the cystic wall. Weber et
al (24) subdivided the
peritumoral cystic meningioma according to the presence of tumor
invasion in the cystic wall.
The underlying mechanism of cyst formation remains
unclear. Intratumoral cysts (Nauta types I and II) are likely to be
caused by microcystic degeneration, ischemic necrosis or hemorrhage
within the tumor (2,23,25). In
addition, transudation or secretory changes within the meningioma
may also lead to the formation of cysts (25); therefore, the cystic wall of
intratumoral cysts (Nauta types I and II) contains neoplastic cells
and its immediate removal is required (3,26,27). The
formation of peritumoral cysts (Nauta type III) may be due to
reactive gliosis toward the meningioma or the evolution of cerebral
edema to form peritumoral cystic cavities (22,23).
Nauta type IV cysts may be a result of the widening of the
subarachnoid spaces and the trapped cerebrospinal fluid around the
tumor (21–23,25,28). A
previous study reported a strong expression of aquaporin 1 in a
case of peritumoral cystic meningioma (29). Consequently, the wall of peritumoral
cysts is likely to be free from tumor cells and its excision is not
required (7,26). However, the cystic wall of
peritumoral cystic meningioma has frequently been reported to be
composed of neoplastic cells (3,19,21,24,30).
The presence of tumor cells on the cystic wall was believed to
result from the spreading of the xanthochromic fluid in the
peritumoral cyst to the wall (3,17,24).
This point of view, however, may provide an insufficient
explanation based on the following two reasons: A study showed that
despite the existence of meningioma cells (atypical) in the
xanthochromic fluid, the cystic wall was not invaded by tumor cells
(24). In addition, other studies
found that the cystic wall was composed of neoplastic cells
(meningothelial type, benign) without the presence of tumor cells
in the xanthochromic fluid (21,23,24).
However, in chordoid or papillary meningiomas, which take on
aggressive metastatic properties, the cystic wall has frequently
been shown to be composed of tumor cells (19,30,31).
This is likely to occur due to the subarachnoid dissemination of
tumor cells (19,32). The presence of meningioma cells in
the cystic fluid is not necessarily an indicator of tumor invasion
in the wall. The formation of peritumoral cystic meningioma with
neoplastic cells on the wall has been suggested to result from
active secretion by the functional tumor cells and responsive glial
proliferation, as well as the possible involvement of necrotic
degeneration (3,23). Degeneration, necrosis, calcification
and mitosis were also observed in the present two cases. The
mechanism underlying the formation of peritumoral cyst meningioma
with neoplastic cells on the wall involves degeneration, necrosis,
responsive glial proliferation, spreading of neoplastic cells in
the fluid or a combination of these (11).
MRI remains the optimal diagnostic means for the
diagnosis of cystic meningioma, but it is not sufficient to
determine the particular tumor type (27). Only microsurgical inspection and
histological examination can lead to the final diagnosis of the
type of cystic meningioma (27).
Combined MRI and diffusion-weighted imaging (DWI) may be efficient
in diagnosing the type of cystic meningioma (4,33);
however, as glioma was the initial diagnosis in the present study,
DWI was not utilized. Chen et al (33) reported that the apparent diffusion
coefficient ratio of intratumoral cystic meningioma obtained using
DWI was lower compared with that of peritumoral cystic meningioma,
based on only three cases. Contrast-enhanced MRI may assist
surgeons in determining whether neoplastic cells are present in the
cystic wall; however, the wall could be enhanced despite the
absence of tumor cells (34).
Furthermore, biopsy was found to detect tumor cells on the cystic
wall, even in cases where these were not detected by
contrast-enhanced MRI (3,27). It is therefore not accurate to
support the absence of tumor cells based merely on the negative
results of contrast-enhanced MRI (20,27,35).
In conclusion, combined MRI and DWI may provide
valuable assistance in the diagnosis of cystic meningioma and its
various types. The diagnosis value of PET/CT in cystic meningioma
requires further investigation and previous studies have
demonstrated that DWI may be superior at distinguishing between the
various types of meningioma (4,30). Two
cases of cystic meningioma were evaluated in the present case
report and microsurgical inspection, multiple biopsies and frozen
sections were sufficient to evaluate the presence or absence of
tumor cells on the cystic wall (17,24,27).
However, the diagnostic accuracy of the presence of tumor cells on
the cyst wall was not 100%; therefore, biopsy remains the most
accurate and reliable treatment option, as compared with imaging
methods, and we recommend whole surgical removal of the cyst.
References
|
1
|
Zee CS, Chen T, Hinton DR, Tan M, Segall
HD and Apuzzo ML: Magnetic resonance imaging of cystic meningiomas
and its surgical implications. Neurosurgery. 36:482–488. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Fortuna A, Ferrante L, Acqui M, Guglielmi
G and Mastronardi L: Cystic meningiomas. Acta Neurochir (Wien).
90:23–30. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Jung TY, Jung S, Shin SR, Moon KS, Kim IY,
Park SJ, Kang SS and Kim SH: Clinical and histopathological
analysis of cystic meningiomas. J Clin Neurosci. 12:651–655. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Zhang D, Hu LB, Zhen JW, Zou LG, Feng XY,
Wang WX and Wen L: MRI findings of intracranial cystic meningiomas.
Clin Radiol. 64:792–800. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sridhar K, Ravi R, Ramamurthi B and
Vasudevan MC: Cystic meningiomas. Surg Neurol. 43:235–239. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Goyal A, Singh AK, Gupta V, Singh D, Tatke
M and Kumar S: Suprasellar cystic meningioma: Unusual presentation
and review of the literature. J Clin Neurosci. 9:702–704. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ueno Y, Tanaka A, Nakayama Y and Nomoto Y:
Intracerebral cyst associated with meningioma. Clin Neurol
Neurosurg. 101:271–274. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Guan TK, Pancharatnam D, Chandran H, Hooi
TK, Kumar G and Ganesan D: Infratentorial benign cystic meningioma
mimicking a hemangioblastoma radiologically and a pilocytic
astrocytoma intraoperatively: A case report. J Med Case Rep.
7:872013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Yamada SM, Fujimoto Y, Kawanishi Y and
Shimizu K: A cystic meningioma misdiagnosed as malignant glioma by
radiologic and intraoperative histological examinations. Brain
Tumor Pathol. 27:111–115. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Rishi A, Black KS, Woldenberg RW, Overby
CM, Eisenberg MB and Li JY: Microcystic meningioma presenting as a
cystic lesion with an enhancing mural nodule in elderly women:
Report of three cases. Brain Tumor Pathol. 28:335–339. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Louis DN, Ohgaki H, Wiestler OD, Cavenee
WK, Burger PC, Jouvet A, Scheithauer BW and Kleihues P: The 2007
WHO classification of tumours of the central nervous system. Acta
Neuropathol. 114:97–109. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Xia L, Zhang H, Yu C, Zhang M, Ren M, Qu
Y, Wang H, Zhu M, Zhao D, Qi X and Yao K: Fluid-fluid level in
cystic vestibular schwannoma: A predictor of peritumoral adhesion.
J Neurosurg. 120:197–206. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wang YQ, Fan T, Zhao XG, Liang C, Qi XL
and Li JY: Pituitary carcinoma with intraspinal metastasis: Report
of two cases and review of the literature. Int J Clin Exp Pathol.
8:9712–9717. 2015.PubMed/NCBI
|
|
14
|
Deb P, Sahani H, Bhatoe HS and Srinivas V:
Intraventricular cystic meningioma. J Cancer Res Ther. 6:218–220.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Obeng K, Rumboldt Z, Tuite G, Welsh CT,
Patel S and Spampinato MV: Atypical cystic meningioma of the
trigeminal nerve in a pediatric patient. AJNR Am J Neuroradiol.
29:398–399. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Fujimoto Y, Kato A, Taniguchi M, Maruno M
and Yoshimine T: Meningioma arising from the trigeminal nerve: A
case report and literature review. J Neurooncol. 68:185–187. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Hu SL, Li F, Hu R, Cui G, Meng H and Feng
H: Atypical histopathologic type of cystic meningioma. Acta
Neurochir (Wien). 152:105–109. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Rosca TI, Carstocea BD, Vlãdescu TG, St
Tihoan C and Gherghescu GG: Cystic optic nerve sheath meningioma. J
Neuroophthalmol. 26:121–122. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Zhi L, Bing L, Yang L, Bo-ning L and Quan
H: Cystic papillary meningioma with subarachnoid dissemination: A
case report and review of the literature. Pathol Res Pract.
205:582–587. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Senbokuya N, Asahara T, Uchida M,
Yagishita T and Naganuma H: Atypical meningioma with large cyst.
Case report. Neurol Med Chir (Tokyo). 46:147–151. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Rengachary S, Batnitzky S, Kepes JJ,
Morantz RA, O'Boynick P and Watanabe I: Cystic lesions associated
with intracranial meningiomas. Neurosurgery. 4:107–114. 1979.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Nauta HJ, Tucker WS, Horsey WJ, Bilbao JM
and Gonsalves C: Xanthochromic cysts associated with meningioma. J
Neurol Neurosurg Psychiatry. 42:529–535. 1979. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Worthington C, Caron JL, Melanson D and
Leblanc R: Meningioma cysts. Neurology. 35:1720–1724. 1985.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Weber J, Gassel AM, Hoch A, Kilisek L and
Spring A: Intraoperative management of cystic meningiomas.
Neurosurg Rev. 26:62–66. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Odake G: Cystic meningioma: Report of
three patients. Neurosurgery. 30:935–940. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Zhao X, Sun JL, Wang ZG, Zhang TG, Wang CW
and Ji Y: Clinical analysis for an unusual large cystic meningioma:
Case report and review of the literature. Clin Neurol Neurosurg.
110:605–608. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Ferrante L, Acqui M, Lunardi P, Qasho R
and Fortuna A: MRI in the diagnosis of cystic meningiomas: Surgical
implications. Acta Neurochir (Wien). 139:8–11. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Sigel RM and Messina AV: Computed
tomography; the anatomic basis of the zone of diminished density
surrounding meningiomas. AJR Am J Roentgenol. 127:139–141. 1976.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Marton E, Feletti A, Basaldella L, Dei Tos
AP, Bendini M and Longatti P: Atypical cystic meningioma
overexpressing AQP1 in early infancy: Case report with literature
review. Acta Paediatr. 97:1145–1149. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Zhao SL, Li Y, Tian XY, Li Z, Huang Q and
Li B: Intraparenchymal cystic chordoid meningioma: A case report
and review of the literature. Neuropathology. 31:648–653. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Enam SA, Abdulrauf S, Mehta B, Malik GM
and Mahmood A: Metastasis in meningioma. Acta Neurochir (Wien).
138:1172–1177; discussion 1177–1178. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Wakabayashi K, Suzuki N, Mori F, Kamada M
and Hatanaka M: Rhabdoid cystic papillary meningioma with diffuse
subarachnoid dissemination. Acta Neuropathol. 110:196–198. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Chen TY, Lai PH, Ho JT, Wang JS, Chen WL,
Pan HB, Wu MT, Chen C, Liang HL and Yang CF: Magnetic resonance
imaging and diffusion-weighted images of cystic meningioma:
Correlating with histopathology. Clin Imaging. 28:10–19. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Arai M, Kashihara K and Kaizaki Y:
Enhancing gliotic cyst wall with microvascular proliferation
adjacent to a meningioma. J Clin Neurosci. 13:136–139. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Demir MK, Müslüman M, Kilicoglu G, Hakan T
and Aker FV: Imaging features of unusual intracranial cystic
meningiomas. Can Assoc Radiol J. 58:109–115. 2007.PubMed/NCBI
|