Introduction
The incidence rates for colorectal cancer have
continued to increase in Korea; in 2012, colorectal cancer was the
second and third most frequently diagnosed cancer in males and
females, respectively (1). For
rectal cancer, an improvement in surgical techniques and the
introduction of multimodality treatments (radiotherapy and
chemotherapy) have improved treatment outcomes (2). The standard surgical procedure for the
treatment of rectal cancer is abdominoperineal resection, low
anterior resection or resection with coloanal anastomosis (3). However, local excision (LE) has been
regarded as an alternative method for selected cases that fulfill
stringent conditions of small-sized T1 tumors with no unfavorable
histological features (4). LE has
advantages in rapid postoperative recovery, avoiding sphincter
ablation (permanent colostomy) and morbidities associated with
radical resection, such as urinary and sexual dysfunction (4).
For locally advanced rectal cancer [LARC; also
referred to as stage T3–4 or N+ rectal cancer, according to the
American Joint Committee on Cancer (AJCC) Cancer Staging Manual]
(5), chemoradiotherapy (CRT) has
been established as a standard preoperative treatment, rather than
a postoperative treatment (6,7).
Preoperative CRT leads to significant improvement in the local
disease control of LARC (8). In
addition, preoperative CRT and a 6-8-week interval prior to the
surgical procedure result in a decrease in the stage and size of
the primary mural tumors, along with a lower risk of regional
lymphadenopathy (9). In a subset of
patients exhibiting marked tumor response to CRT, preoperative CRT
may transform LARC so that LE may safely replace radical
surgery.
The present study presents the case of a stage T3
rectal cancer patient who was treated with LE following
preoperative CRT, and discusses issues associated with this
approach.
Case report
A 69-year-old male was referred to the Soonchunhyang
University Hospital (Cheonan, South Korea) on 28th April
2013 for further evaluation and the treatment of rectal cancer,
which was diagnosed during national medical check-ups. The patient
had no specific symptoms associated with rectal cancer. The distal
portion of the mass was palpated 2 cm from the anal verge on a
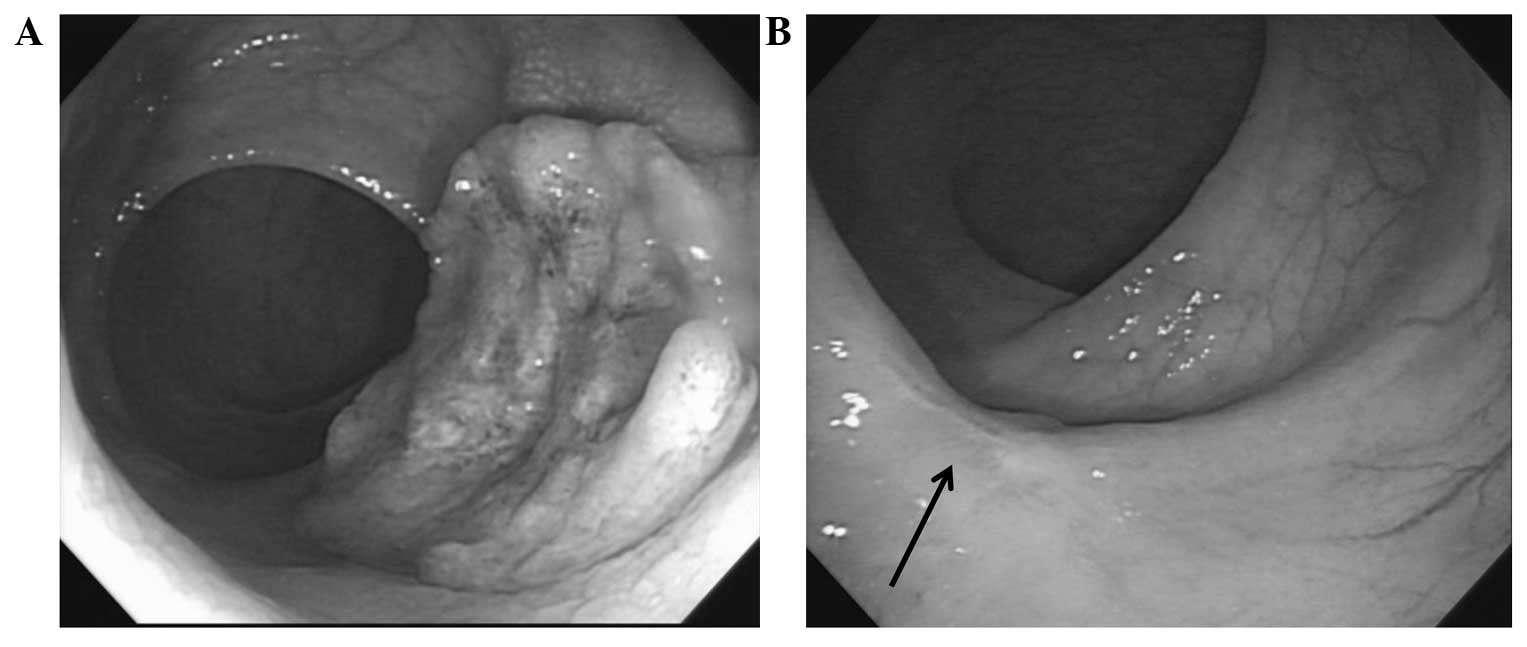
digital rectal examination. Colonoscopy showed the presence of an
ulcerofungating mass on the rectal wall (Fig. 1A). Pathological examination of a
biopsy specimen revealed moderately differentiated adenocarcinoma.
The serum levels of carcinoembryonic antigen were determined by a
routine blood test and were 4.4 ng/ml (normal range, 0–5.0 ng/ml).
Abdominopelvic computed tomography (CT) and pelvic magnetic
resonance imaging (MRI) revealed tumor invasion into the perirectal
tissues, but no enlargement of the lymph nodes was observed.
18F-fluorodeoxyglucose positron emission tomography
(PET)-CT showed a maximum standardized uptake value of 13.8 in the
primary rectal tumor. The pretreatment clinical stage (cStage) was
determined to be T3N0M0 (IIA) according to the AJCC Cancer Staging
Manual (5). The present study was
conducted in accordance with the guidelines of the Institutional
Review Board at the Soonchunhyang University Hospital.
Preoperative radiotherapy of 45 Gy in 25 fractions
was delivered to the pelvis, followed by a boost of 5.4 Gy in three
fractions within 5.5 weeks, according to guidelines (3). The patient underwent CT simulation in
the prone position using a belly board. The target volume included
the presacral space, mesorectum, gross tumor volume and the
regional lymphatics, including the presacral, internal iliac,
distal common iliac and perirectal lymphatics. The boost target
volume included the gross tumor volume and adjacent mesorectum. A
three-dimensional conformal radiotherapy plan was created using the
Eclipse Treatment Planning system (Varian Medical Systems, Inc.,
Palo Alto, CA, USA). The three-field plan consisted of a 15-MV
photon opposed lateral field with wedges of 45° and a 6-MV photon
posterior-anterior field. Radiotherapy was performed using a
Novalis Tx system (Varian Medical Systems, Inc.; BrainLab AG,
Feldkirchen, Germany). Preoperative chemotherapy with
5-fluorouracil (Ildong Pharmaceutical Co., Ltd., Seoul, South
Korea) and leucovorin (Samjin Pharmaceutical Co., Ltd., Seoul,
South Korea) was administered concurrently with the radiotherapy.
Briefly, two cycles of a bolus infusion of 5-fluorouracil (450
mg/m2/d) and leucovorin (20 mg/m2/d) were
administered for 5 days during weeks 1 and 5 of radiotherapy.
At 7 weeks following preoperative CRT completion,
the tumor response to CRT was assessed. The mass or stenosis was
not palpated on digital rectal examination. A scar lesion with
whitening of the mucosa, but no intraluminal mass or ulceration,
was observed on colonoscopy (Fig.
1B). A CT scan showed diminished rectal wall thickness.
Following discussion with the patient regarding the presence of a
presumed complete CRT response and description of the surgical
procedure methods, the patient selected to undergo LE, despite
being informed that it was not the standard treatment and carried
potential risks of disease recurrence. Written informed consent was
obtained from the patient.
Transanal full-thickness LE was performed with ≥1 cm
margin around the scar, including the adjacent perirectal fat
tissues. The defect of the rectal wall was closed by using
absorbable sutures. A pathological examination was conducted
according to guidelines (10), and
revealed no residual cancer cells in the specimen, with no
lymphovascular or perineural invasion. The patient was discharged
the following day after surgery. Treatment side-effects included
nausea during CRT and pain at the surgical site, both of which
subsided with conservative management, including treatment with 8
mg ondansetron (GlaxoSmithKline plc., Seoul, South Korea) and
Ultracet® tablets (37.5 mg tramadol HCl and 325 mg acetaminophen;
Janssen Korea Ltd., Seoul, South Korea). Postoperative chemotherapy
was not administered.
Follow-up evaluation consisted of physical and
digital rectal examination, complete blood counts, liver function
tests and measurement of carcinoembryonic antigen levels, every 3
months. Chest radiography and CT of the abdomen and pelvis were
conducted every 6 months. Colonoscopy and PET-CT was performed
every year. At 30 months post-treatment, the patient was alive with
no evidence of disease and no severe complications.
Discussion
The current oncology practice guidelines describe
the use of LE on rectal cancer appropriate only for highly selected
patients with a good prognosis. The eligibility criteria for LE in
the National Comprehensive Cancer Network guidelines include the
following: T1 tumor stage, tumor size of <3 cm, <30% bowel
circumference, clear margin (>3 mm), mobile non-fixed, no
lymphovascular or perineural invasion, well-to-moderate
differentiation and no lymphadenopathy on pretreatment imaging
(3). Stage T2–3 rectal cancer is
excluded from LE indications. However, T2–3 rectal tumors are a
heterogeneous group when assessed by CRT response. Patients with
LARC were demonstrated to have various outcomes according to the
degree of response to preoperative CRT (11,12). In
a previous study, patients with an initial cStage II–III and
post-treatment (y) pathological (p)Stage 0-I rectal cancer (staged
according to the AJCC Cancer Staging Manual) (5), showed similar favorable outcomes as
patients with pStage I cancer (7).
Therefore, the current LE criteria for T1 rectal cancer may be
expanded to include a subgroup of T2–3 rectal cancer that exhibits
excellent tumor response to preoperative CRT.
Few prospective clinical trials have been conducted
to address the feasibility of LE following preoperative CRT in T2–3
rectal cancer (13–15). In a previous trial in Italy, 63
patients with T2 (n=21) or T3 (n=42) rectal cancer were enrolled,
and clinical lymphadenopathy was present in 39 patients (62%)
(13). The criteria of observation
following LE (ypStage T0–1 with no cancer cells on resected
specimen margins) were satisfied in 43 patients (68%); among them,
only 1 patient developed recurrence, which presented as distant
metastases. In another trial in Poland, 86 patients with T1-3N0
rectal cancer received a short-course of radiotherapy or a
long-course of CRT, both with a 6-week interval until LE (14). A total of 63 (71%) patients responded
well to treatment, defined as ypT0–1 without unfavorable prognostic
factors (positive margin, tumor fragmentation, grade 3,
lymphovascular or perineural invasion) (14). In these patients, the Kaplan-Meier
incidence of local recurrence at 2 years was 10%, with no
significant difference between the two preoperative treatments
(14). No solitary distant
metastasis was observed.
To the best of our knowledge, only one randomized
controlled trial has been conducted to date. In this trial by
Lezoche et al (15), patients
with rectal cancer of a small size (≤3 cm), T2N0 stage,
well-to-moderately differentiated and distal location were
randomized following preoperative CRT, in order to receive
transanal endoscopic microsurgery or laparoscopic total mesorectal
excision. Long-term oncological outcomes, including local
recurrence, distant metastasis and cancer-associated survival, were
not significantly different between the two groups. Disease
recurrence, local or distant, developed only in patients with low
or no response to preoperative CRT in both treatment groups.
Although full-thickness LE occasionally retrieves
1–2 lymph nodes adjacent to the primary tumor, it can not address
mesorectal lymph nodes as thoroughly as total mesorectal excision
(16). Overall, without preoperative
treatments, T1 rectal cancer has a 10–20% rate of lymph node
metastasis (4,16). When excluding T1 tumors possessing
high-risk clinical and histological features, this rate is <10%;
this T1 subgroup constitutes the current inclusion criteria for LE
(16). In LARC, post-CRT positive
ypN rates in ypT0–1 have been reported to be <10% (17). Metastatic cancer cells on lymph nodes
regress along the primary tumor regression by CRT. The clinical
stage of the present case was determined to be T3N0; even when
subclinical mesorectal lymph node disease was presumed to be
present, CRT may have been sufficient for microscopic disease
eradication. Significant tumor regression following CRT also
represents favorable biological tumor behavior (12).
An obstacle in implementing this approach in
patients with rectal cancer is the limited ability for preoperative
clinical or radiological assessment of the post-CRT tumor status
(18). Radiology investigations
using PET and diffusion-weighted MRI are undergoing to improve the
accuracy in evaluating the response of rectal cancer to CRT
(19,20). However, the post-LE ypT status
(ypT0-1) remains the most reliable parameter for determining
whether to proceed with LE. Radical resection following initial LE
in patients who exhibit a lower than predicted response was
reported to not compromise long-term outcomes (21,22).
Among the pretreatment patient or tumor characteristics, low serum
levels of carcinoembryonic antigen (≤5 ng/ml) have been
demonstrated to be independently associated with a good
pathological response of LARC to CRT (23). The patient discussed in the present
study had carcinoembryonic antigen levels of 4.4 ng/ml, and a
post-CRT pathological complete response.
LE requires strict adherence to an intense
surveillance schedule to detect any recurrence early in order to
provide salvage treatment. The present patient has been
disease-free for 30 months post-treatment; however, further close
follow-up is required as rectal cancer has a tendency for late
recurrence following preoperative CRT (24).
In conclusion, the present case report supports that
LE may be a feasible alternative for T3 rectal cancer treatment
following significant response to CRT. The physician may need to
discuss this treatment option with a patient suspected of a
significant CRT response. Until further prospective and randomized
clinical trials are conducted, this approach may be particularly
valuable in elderly and comorbid patients for whom radical surgery,
currently the sole standard treatment, includes high morbidity and
mortality risks, or patients who are reluctant to undergo
sphincter-ablation surgery.
Acknowledgements
The present study was supported by the Soonchunhyang
University Research Fund.
References
|
1
|
Jung KW, Won YJ, Kong HJ, Oh CM, Cho H,
Lee DH and Lee KH: Cancer statistics in Korea: Incidence,
Mortality, Survival, and Prevalence in 2012. Cancer Res Treat.
47:127–141. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kosinski L, Habr-Gama A, Ludwig K and
Perez R: Shifting concepts in rectal cancer management: A review of
contemporary primary rectal cancer treatment strategies. CA Cancer
J Clin. 62:173–202. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
National Comprehensive Cancer Network
(NCCN): Rectal cancer. NCCN Clinical Practice Guidelines in
Oncology Version 1. http://www.nccn.org/professionals/physician_gls/f_guidelines.aspAccessed.
November 23–2014
|
|
4
|
Maeda K, Koide Y and Katsuno H: When is
local excision appropriate for ‘early’ rectal cancer? Surg Today.
44:2000–2014. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Edge SB, Byrd DR, Compton CC, Fritz AG,
Greene FL and Trotti A: AJCC Cancer Staging Manual (7th).
Springer-Verlag. New York, NY: 2010.
|
|
6
|
Lee JW, Lee JH, Kim JG, Oh ST, Chung HJ,
Lee MA, Chun HG, Jeong SM, Yoon SC and Jang HS: Comparison between
preoperative and postoperative concurrent chemoradiotherapy for
rectal cancer: An institutional analysis. Radiat Oncol J.
31:155–161. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Yeo SG, Kim DY, Park JW, Choi HS, Oh JH,
Kim SY, Chang HJ, Kim TH and Sohn DK: Stage-to-stage comparison of
preoperative and postoperative chemoradiotherapy for T3 mid or
distal rectal cancer. Int J Radiat Oncol Biol Phys. 82:856–862.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Yeo SG and Kim DY: An update on
preoperative radiotherapy for locally advanced rectal cancer. J
Korean Soc Coloproctol. 28:179–187. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Yeo SG, Kim DY, Kim TH, Chang HJ, Oh JH,
Park W, Choi DH, Nam H, Kim JS and Cho MJ: Pathologic complete
response of primary tumor following preoperative chemoradiotherapy
for locally advanced rectal cancer: Long-term outcomes and
prognostic significance of pathologic nodal status (KROG 09–01).
Ann Surg. 252:998–1004. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Iacobuzio-Donahue CA and Montgomery EA:
Gastrointestinal and Liver Pathology. Foundations in Diagnostic
Pathology. Goldblum JR: (2nd). Elsevier. (Philadelphia, PA).
2012.
|
|
11
|
Yeo SG, Kim DY, Park JW, Oh JH, Kim SY,
Chang HJ, Kim TH, Kim BC, Sohn DK and Kim MJ: Tumor volume
reduction rate after preoperative chemoradiotherapy as a prognostic
factor in locally advanced rectal cancer. Int J Radiat Oncol Biol
Phys. 82:e193–e199. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Maas M, Nelemans PJ, Valentini V, Das P,
Rödel C, Kuo LJ, Calvo FA, García-Aguilar J, Glynne-Jones R,
Haustermans K, et al: Long-term outcome in patients with a
pathological complete response after chemoradiation for rectal
cancer: A pooled analysis of individual patient data. Lancet Oncol.
11:835–844. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Pucciarelli S, De Paoli A, Guerrieri M, La
Torre G, Maretto I, De Marchi F, Mantello G, Gambacorta MA,
Canzonieri V, Nitti D, et al: Local excision after preoperative
chemoradiotherapy for rectal cancer: Results of a multicenter phase
II clinical trial. Dis Colon Rectum. 56:1349–1356. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Bujko K, Richter P, Smith FM, Polkowski W,
Szczepkowski M, Rutkowski A, Dziki A, Pietrzak L, Kołodziejczyk M
and Kuśnierz J: Preoperative radiotherapy and local excision of
rectal cancer with immediate radical re-operation for poor
responders: A prospective multicentre study. Radiother Oncol.
106:198–205. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Lezoche E, Baldarelli M, Lezoche G,
Paganini AM, Gesuita R and Guerrieri M: Randomized clinical trial
of endoluminal locoregional resection versus laparoscopic total
mesorectal excision for T2 rectal cancer after neoadjuvant therapy.
Br J Surg. 99:1211–1218. 2012. View
Article : Google Scholar : PubMed/NCBI
|
|
16
|
Heafner TA and Glasgow SC: A critical
review of the role of local excision in the treatment of early (T1
and T2) rectal tumors. J Gastrointest Oncol. 5:345–352.
2014.PubMed/NCBI
|
|
17
|
Read TE, Andujar JE, Caushaj PF, Johnston
DR, Dietz DW, Myerson RJ, Fleshman JW, Birnbaum EH, Mutch MG and
Kodner IJ: Neoadjuvant therapy for rectal cancer: Histologic
response of the primary tumor predicts nodal status. Dis Colon
Rectum. 47:825–831. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Hingorani M, Hartley JE, Greenman J and
Macfie J: Avoiding radical surgery after pre-operative
chemoradiotherapy: A possible therapeutic option in rectal cancer?
Acta Oncol. 51:275–284. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kim JW, Kim HC, Park JW, Park SC, Sohn DK,
Choi HS, Kim DY, Chang HJ, Baek JY, Kim SY, et al: Predictive value
of (18)FDG PET-CT for tumour response in patients with locally
advanced rectal cancer treated by preoperative chemoradiotherapy.
Int J Colorectal Dis. 28:1217–1224. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Genovesi D, Filippone A, Ausili Cèfaro G,
Trignani M, Vinciguerra A, Augurio A, Di Tommaso M, Borzillo V,
Sabatino F, Innocenti P, et al: Diffusion-weighted magnetic
resonance for prediction of response after neoadjuvant
chemoradiation therapy for locally advanced rectal cancer:
Preliminary results of a monoinstitutional prospective study. Eur J
Surg Oncol. 39:1071–1078. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Gagliardi G, Newton TR and Bailey HR:
Local excision of rectal cancer followed by radical surgery because
of poor prognostic features does not compromise the long term
oncologic outcome. Colorectal Dis. 15:e659–e664. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Levic K, Bulut O, Hesselfeldt P and Bülow
S: The outcome of rectal cancer after early salvage TME following
TEM compared with primary TME: A case-matched study. Tech
Coloproctol. 17:397–403. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Yeo SG, Kim DY, Chang HJ, Park JW, Oh JH,
Kim BC, Baek JY, Kim SY and Kim TH: Reappraisal of pretreatment
carcinoembryonic antigen in patients with rectal cancer receiving
preoperative chemoradiotherapy. Tumori. 99:93–99. 2013.PubMed/NCBI
|
|
24
|
Yeo SG and Kim MJ, Kim DY, Chang HJ, Baek
JY, Kim SY, Kim TH, Park JW, Oh JH and Kim MJ: Patterns of failure
in patients with locally advanced rectal cancer receiving
pre-operative or post-operative chemoradiotherapy. Radiat Oncol.
8:1142013. View Article : Google Scholar : PubMed/NCBI
|