Introduction
Myocardial apoptosis is associated with a number of
physiological and pathophysiological processes, and is the
cytological basis of the development and progression of a number of
cardiovascular diseases, including acute and chronic loss of
cardiomyocytes in myocardial infarction, ischemic heart disease,
reperfusion injury and various forms of cardiomyopathy; it is
regulated by the expression of various genes (1–3). There
are >27 viruses that are known to cause viral myocarditis (VMC),
including coxsackie virus, parvovirus B19, enterovirus, adenovirus,
rubella, polio, human immunodeficiency virus (HIV)-1,
cytomegalovirus, and hepatitis A and C (4,5). Fas and
FasL, which are members of the tumor necrosis factor/nerve growth
factor family, have been demonstrated to have pivotal roles in the
apoptosis of normal and cancerous cells (6–8). In
animal models of myocardial infarction and myocardial overload, Fas
levels have been demonstrated to increase 131- and 21-fold,
respectively (9,10). Furthermore, Fas mRNA levels were
observed to be elevated 2-fold in newborn animal models of
myocardial hypoxia (11). Fas, which
is also known as Apo-1 or CD95, is a cell-surface receptor that has
a key role in apoptotic signaling in various cell types (12). Fas ligand (FasL), which is also known
as CD95L, is a member of the tumor necrosis factor super family
that is capable of triggering an apoptotic cascade by cross-linking
with its Fas receptor (8). The roles
of Fas/FasL in the regulatory mechanisms and the apoptosis of
myocardiocytes have not yet been elucidated.
Shenqi Fuzheng injection (SFI) is an injectable
traditional Chinese herbal formulation comprising two Chinese
herbs, Radix Codonopsis (dangshen), which is the root of
Codonopsis pilosulae and Radix Astragali, which is the root
of Astragali mongolici, that, in China, are commonly used to
improve the immune functions of patients with chronic diseases in
an integrative and holistic manner (13). SFI was approved by the State Food and
Drug Administration of the People's Republic of China in 1999 as an
antitumor injection to be manufactured and marketed in China
(14,15). Codonopsis pilosula and
Astragalus membranaceus have previously been demonstrated to
promote the apoptosis of cancer cells (16,17). In
addition, a review of animal studies has reported that, to a
certain extent, Radix Astragali reduces pathological damage to
normal mice sperm cell and thymus cells in mice, and inhibits their
excessive apoptosis (18).
Furthermore, C. pilosula has been shown to prevent and
control the apoptosis of alveolar epithelium and pulmonary vascular
endothelial cells in burned mice via the Fas/FasL pathway (19). Aqueous extracts of A.
membranaceus increase immunity by upregulating Bc1-2 expression
and inhibiting cell apoptosis (20).
Furthermore, these aqueous extracts are capable of inhibiting
necrosis and the apoptosis of neurons following
ischemia/reperfusion injury; therefore, they may provide protective
effects for the treatment of acute phase stroke (20).
The present study established mouse models of
myocardial apoptosis by the injection of coxsackievirus group B
type 3 (CVB3). CVB3 damages myocardial cells directly, or
indirectly through autoimmune reactions, leading to the
degeneration and necrosis of myocardial cells or interstitial
inflammatory cell infiltration and fibrosis (21). Fas and FasL are apoptosis-inducing
proteins that play an important role in the clearance of T cells,
the regulation of lymphatic activation and in autoimmune processes
via cytotoxic T lymphocytes (22).
The therapeutic effects of SFI were investigated in the mouse
models of VMC by assessing myocardial apoptosis and the expression
levels of Fas and FasL.
Materials and methods
Preparation of virus and animal
models
Nancy strain CVB3 was purchased from the Wuhan
Institute of Virology of the Chinese Academy of Sciences (Wuhan,
China). A total of 120 male healthy BALB/c mice, aged 5 weeks and
weighing 16–20 g, were provided by Shanghai SLAC Experimental
Animals Co., Ltd. [Shanghai, China; animal quality license, SCXK
(HU) 2007-0005]. Mice were randomly divided into five groups as
follows: Blank control group (n=20), negative control group (n=28),
ribavirin group (n=24), low-dose SFI group (n=24) and high-dose SFI
group (n=24). Blank control group was administered 0.1 ml
Dulbecco's modified Eagle medium (Gibco; Thermo Fisher Scientific,
Inc., Waltham, MA, USA) without CVB3 and after 0.5 h, 0.4 ml NaCl
(0.9%) was injected into the abdominal cavity and mice were
provided with a normal diet for 30 days. The remaining four groups
were injected with 5×102 50% tissue culture infective
dose of CVB3 fluid (0.1 ml) and, after 0.5 h, 0.4 ml NaCl (0.9%),
0.4 ml ribavirin, 0.4 ml SFI and 0.9 ml SFI, respectively, and were
provided with normal diet for 30 days.
Reagents
Terminal deoxynucleotidyl transferase dUTP nick-end
labeling (TUNEL) assay kits were purchased from Roche Diagnostics
(Basel, Switzerland). Rabbit anti-Fas (sc-1024) and FasL (sc-834)
primary polyclonal antibody and biotinylated FasL secondary
antibody (sc-834) kits were purchased from Santa Cruz
Biotechnology, Inc. (Dallas, TX, USA). Antibody dilution-protection
fluid was purchased from Applygen Technologies, Inc., (Beijing,
China), and 3,3′-diaminobenzidine (DAB) kits were purchased from
Beijing Zhongshan Golden Bridge Biotechnology Co., Ltd. (Beijing,
China).
Experimental drugs
SFI containing Radix Codonopsis, astragalus, and the
formulation additives sodium chloride and sodium metabisulfite was
produced by Lizhu Group Limin Pharmaceutical Factory (Shaoguan,
China), and each 250 ml SFI contained 10 g Radix Codonopsis and
Astragalus, respectively. Ribavirin (Virazole®) was
purchased from Tianjin Kingyork Group Co., Ltd., (Tianjin, China)
and supplemented with normal saline to form a 0.6825 mg/ml
ribavirin solution prior to abdominal injection.
Sampling of experimental animals
The protocol of the study was approved by the Animal
Ethics Committee and University Committee on the Use and Care of
Animals of Fujian Medical University (Fuzhou, China), in accordance
with the guidelines outlined by the Ethics Committee of the
Ministry of Health of China. Cardiac tissue samples were harvested
from randomly chosen mice, following sacrifice via spinal
dislocation at 8:00 a.m. on days 3, 10 and 30. Samples were fixed
using 10% paraformaldehyde and sliced to 4–6 µm following paraffin
embedding to be used for TUNEL and immunohistochemical
detection.
Detection of cardiac cell apoptosis
using TUNEL
Following conventional dewaxing and hydration,
cardiac muscle sections were incubated with proteinase K (20 mg/ml
in Tris/HCl, pH 7.4–8.0) for 15 min at room temperature. TUNEL
reaction mixture (50 µl TdT and 450 µl fluorescein-dUTP) was added,
the sections were placed in a humidified box at 37°C for 60 min and
the sections were analyzed using immunofluorescence under an
Olympus BH2 fluorescence microscope (Olympus Corporation, Tokyo,
Japan). Transforming agent was added, and the sections were
incubated in humidified box at 37°C for 30 min. Sections were
developed by incubation with DAB at room temperature, which was
monitored using an Olympus BH2 fluorescence microscope.
Subsequently, the sections were counterstained using hematoxylin
(Abcam, Cambridge, MA, USA), washed with tap water, dehydrated,
treated with xylene and sealed with neutral rubber. Apoptotic cells
were stained brown and visualized under an Olympus BH2 fluorescence
microscope. From each section, the mean of five fields of view was
selected and the apoptotic index (AI) was calculated using Motic
Images Advanced computed imaging software (version 3.2; Motic,
Xiamen, China) as follows: AI (%) = (number of positive
nuclei/total number of nuclei) × 100.
Detection of Fas and FasL protein
expression levels using immunohistochemistry
Following dewaxing and hydration using gradient
alcohol, sections were incubated for 10 min with 3% hydrogen
peroxide at room temperature in order to inhibit endogenous
peroxidase activity. Fas and FasL were subjected to heat-induced
antigen retrieval in Tris-EDTA (pH 9.0) buffer and citrate buffer,
respectively. Sections were incubated with anti-Fas (X-2O; 1:25)
and anti-FasL (N-2O; 1:40) primary antibodies overnight at 4°C in a
humidified box. Following washing with five times with PBS for 2
min, the sections were incubated with biotinylated FasL secondary
antibody (no dilution) for 20 min at room temperature. Horseradish
peroxidase-conjugated avidin-biotin was subsequently added and the
sections were incubated for 20 min at room temperature. Mean
integral optical density of positive expression was measured in
five randomly selected visual fields using Image Pro Plus 6.0
software (Media Cybernetics, Inc., Rockville, MD, USA).
Statistical analysis
Statistical analysis was performed using SPSS
software, version 13.0 (SPSS, Inc., Chicago, IL, USA). All the data
are expressed as the mean ± standard deviation. Intergroup
differences were compared using one way-analysis of variance,
whereas between group comparisons were performed using least
significant difference test. P<0.05 was considered to indicate a
statistically significant difference.
Results
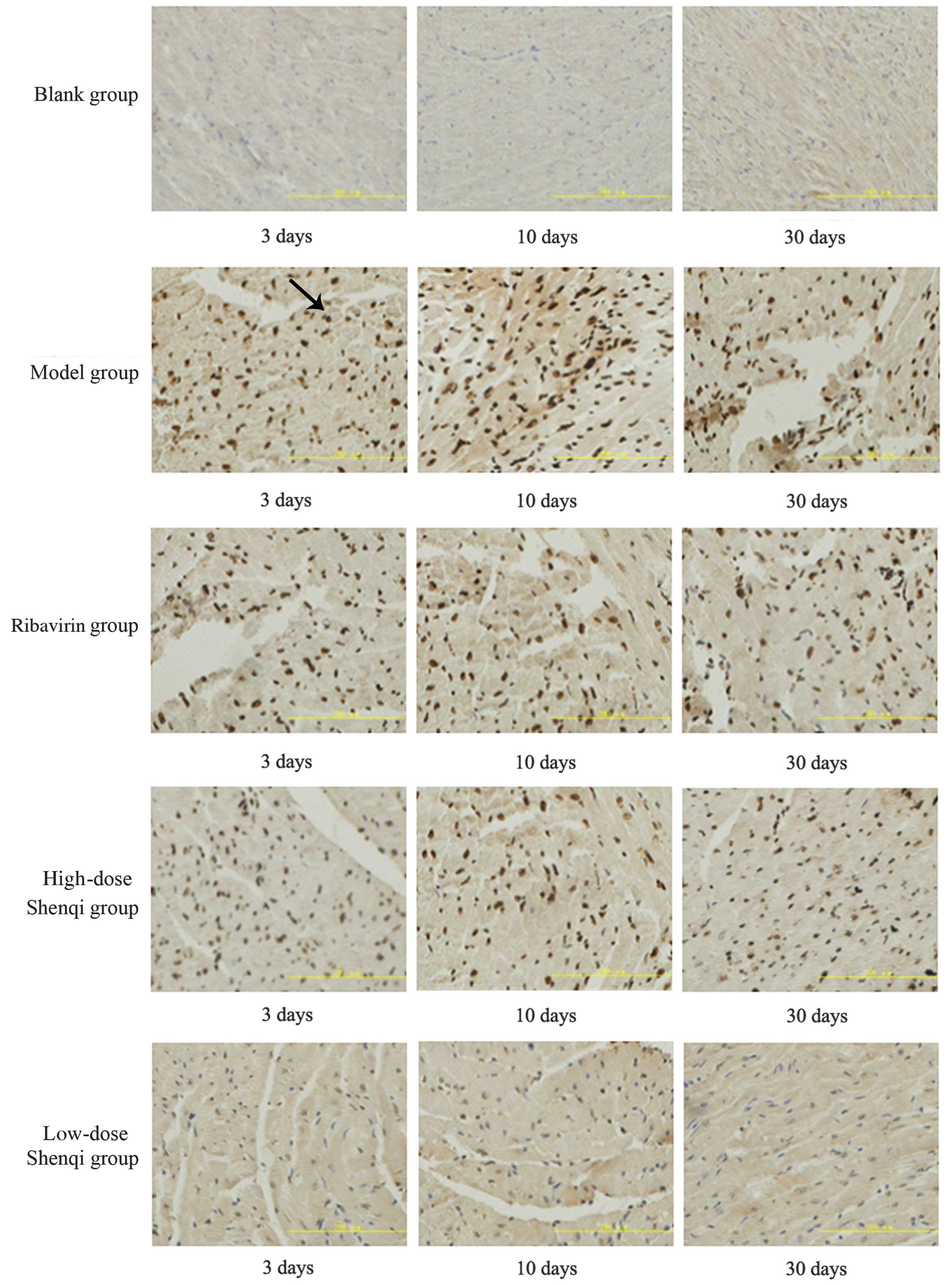
Myocardial apoptosis in the mice at
various time points
Myocardial apoptosis was identified by the presence
of brown apoptotic cells, rounded nuclear karyopyknosis and oval
brown masses (Fig. 1). In the blank
control group, normal myocardial cells were detected; the nuclei
were pale blue and nuclear pyknosis was not observed. However, in
the model group, a large number of cardiac muscle cells contained
brown round or oval nuclei and meniscus-shaped chromatin, which are
characteristic of apoptosis. Strong TUNEL positive staining was
detected in the nucleus, with minimal staining detected in the
cytoplasm. The brown masses and changed to the nuclei became more
evident at day 10, but cells appeared less apoptotic by day 30. In
the virally infected cells, low- and high-dose SFI administration
induced a reduction in the number of apoptotic cells in comparison
with the model group at various time points, with the high-dose SFI
group exhibiting the most evident difference from the model group
(Fig. 1).
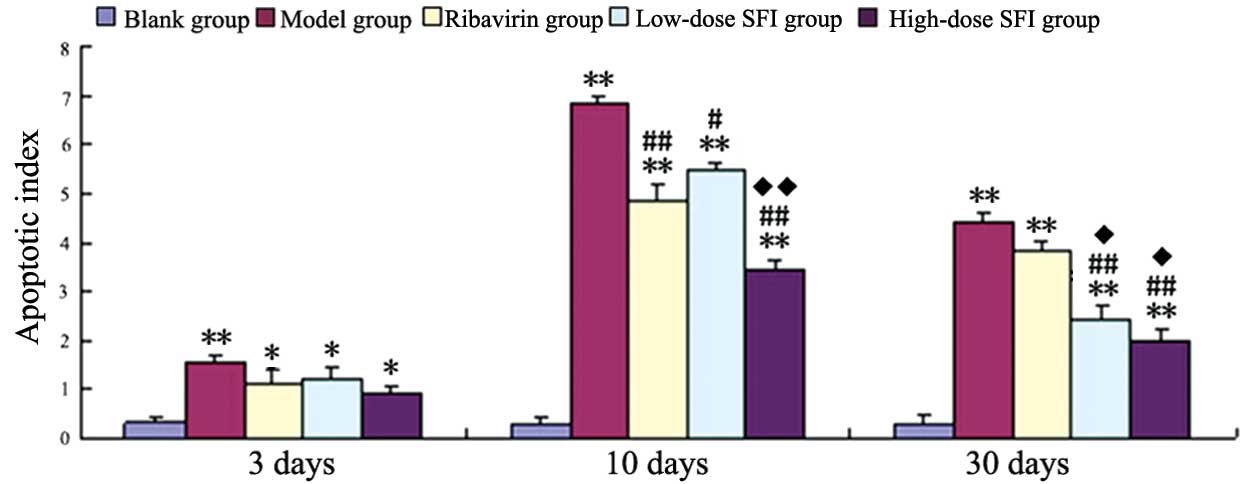
Effects of SFI on the apoptosis of
myocardial cells in the mouse model of VMC
In the model group, the AI of cardiomyocytes was
significantly increased, as compared with the blank group at all
three time points (P<0.01). The AI of myocardial cells in each
therapy group was not significantly reduced at day 3 (acute phase),
as compared with the model group; however, the AI was significantly
reduced by varying degrees on day 10 (acute phase; ribavirin and
high-dose SFI, P<0.01; low-dose SFI, P<0.05). The greatest
reduction was detected in the high-dose SFI group, which showed a
significant difference compared with the ribavirin group
(P<0.05). However, no significant difference was detected
between the ribavirin and low-dose SFI groups on day 10. A
significant reduction in the AI of cardiomyocytes was detected at
day 30 in the high- and low-dose SFI groups as compared with the
model group (P<0.01); however, no significant differences were
detected between these groups. The low- and high-dose SFI groups
exhibited significant differences from the ribavirin group on day
30 (P<0.05; Fig. 2 and Table I).
 | Table I.Effects of Shenqi Fuzheng injection
(SFI) on the apoptotic index in a mouse model of viral
myocarditis. |
Table I.
Effects of Shenqi Fuzheng injection
(SFI) on the apoptotic index in a mouse model of viral
myocarditis.
| Group | Day 3 | Day 10 | Day 30 |
|---|
| Blank control | 0.32±0.09 | 0.27±0.13 | 0.29±0.18 |
| Model |
1.54±0.17a |
6.83±0.16a |
4.40±0.17a |
| Ribavirin |
1.09±0.28b |
4.84±0.30a,c |
3.80±0.24a |
| Low-dose SFI |
1.21±0.22b |
5.49±0.11a,d |
2.40±0.33a,c,f |
| High-dose SFI |
0.91±0.16b |
3.43±0.17a,c,e |
2.00±0.25a,c,f |
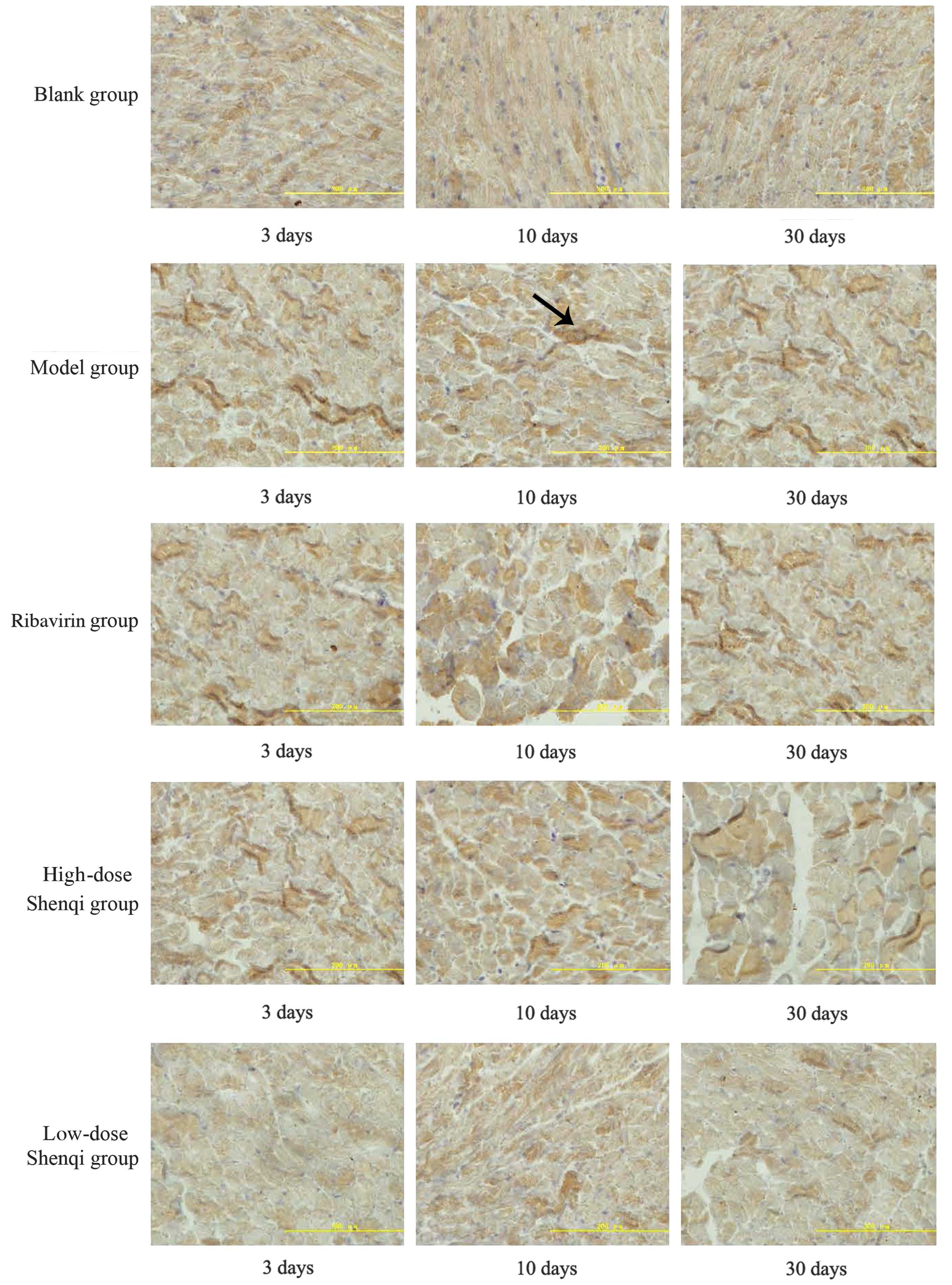
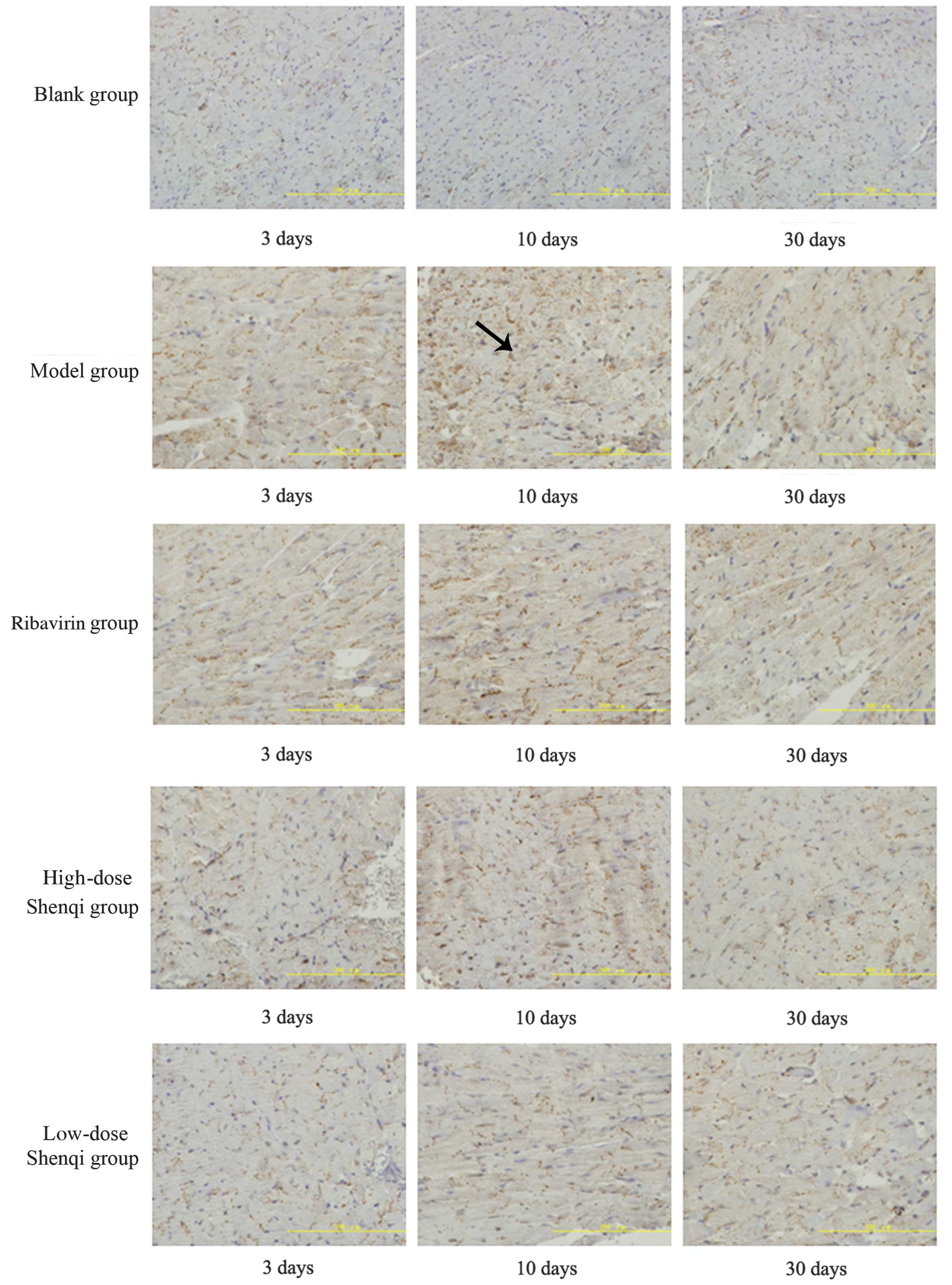
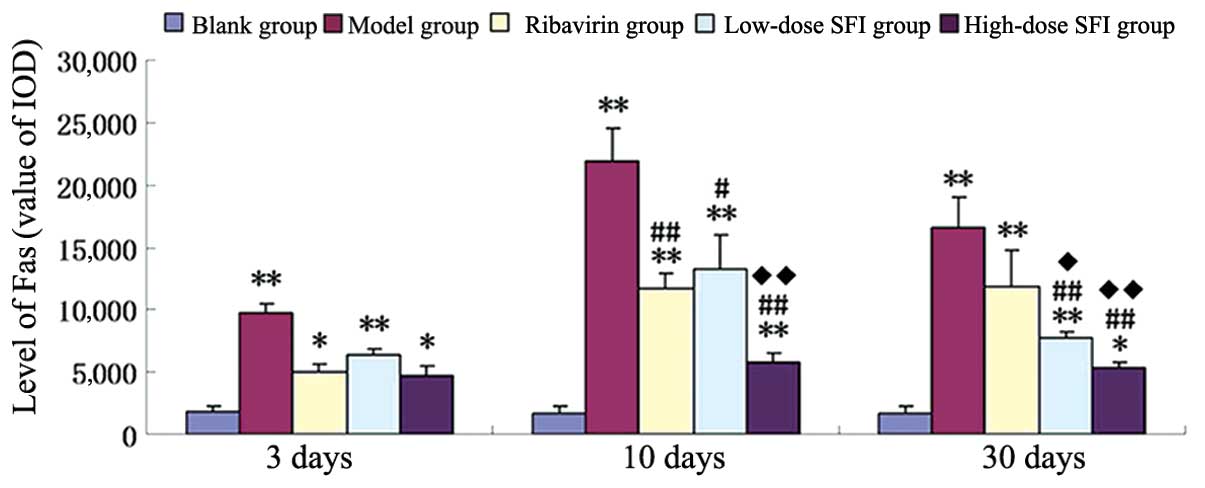
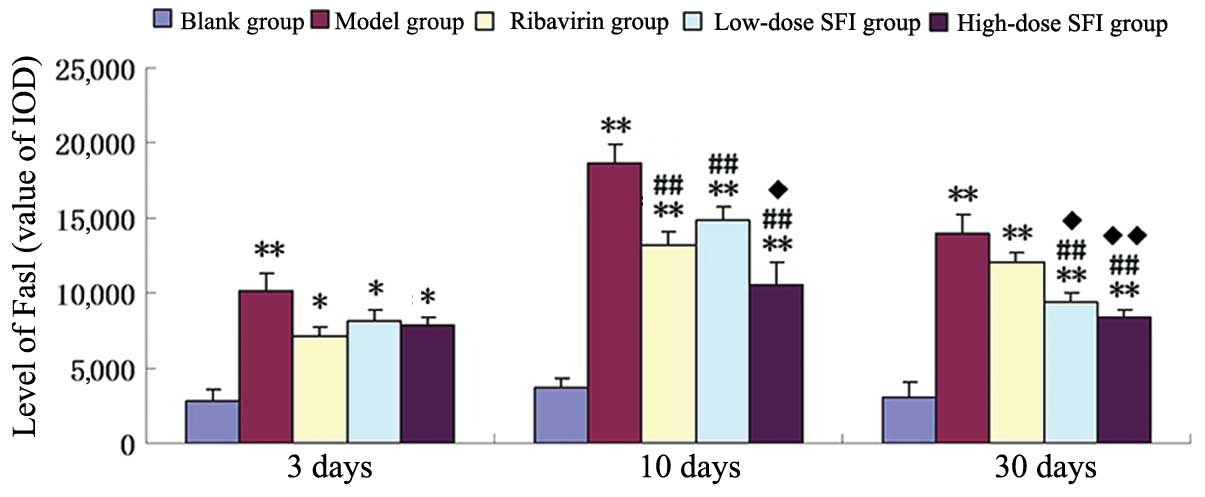
Immunohistochemical analysis of
Fas/FasL proteins in the myocardial cells of the mice at various
time points
Fas protein expression was demonstrated by
homogeneous brown staining of the cell membrane and cytoplasm and a
lack of nuclear staining (Fig. 3, as
indicated by an arrow). FasL protein expression was demonstrated by
homogeneous brown staining or dark brown particles located in the
cell membrane and cytoplasm, and a lack of nuclear staining
(Fig. 4, as indicated by an arrow).
Low expression levels of Fas and FasL proteins were detected in the
blank group at each time point. The greatest amount of brown
staining was detected in the model group on day 3, and no
significant reduction in the amount was detected in the therapy
groups. A significant increase in the amount of brown staining was
detected in each group, with the exception of the blank group, on
day 10, with the greatest increase demonstrated in the model group,
and the smallest increase in the high-dose SFI group. The low-dose
SFI and ribavirin groups exhibited more evident deposits of brown
particles. At day 30, the number of brown particles was reduced in
all the groups, with the greatest reductions detected in the high-
and low-dose SFI groups.
Effects of SFI on the expression
levels of Fas and FasL proteins in the myocardial cells of a mouse
model of VMC
A significant increase in the expression levels of
Fas and FasL proteins was detected in the model group, as compared
with the blank group at all time points (P<0.01). No significant
reduction in Fas and FasL protein expression levels was detected in
each of the therapy groups, as compared with the model group on day
3 (acute phase); however, all the groups demonstrated a reduction
in the expression levels of Fas and FasL on day 10 (acute phase),
to varying degrees (P<0.01 or P<0.05). The high-dose SFI
group demonstrated the largest reductions compared with the model
group (P<0.01), and also exhibited significant differences in
Fas (P<0.01) and FasL (P<0.05) as compared with the ribavirin
group (P<0.01). No significant differences were detected between
the low-dose SFI and ribavirin groups. At day 30 (chronic phase),
both the low- and high-dose SFI groups demonstrated significant
reductions in the expression levels of Fas and FasL compared with
the model group, although no significant differences were detected
between the two SFI groups. Furthermore, Fas and FasL protein
expression levels were significantly lower in the low- and
high-dose SFI groups, as compared with the ribavirin group
(P<0.05 and P<0.01, respectively) (Figs. 5 and 6; Tables II
and III, respectively).
 | Table II.Effects of Shenqi Fuzheng injection
(SFI) on expression levels of Fas protein in a mouse model of viral
myocarditis. |
Table II.
Effects of Shenqi Fuzheng injection
(SFI) on expression levels of Fas protein in a mouse model of viral
myocarditis.
| Group | Day 3 | Day 10 | Day 30 |
|---|
| Blank control | 1,817.54±450.86 | 1,644.11±648.06 | 1,697.95±588.73 |
| Model |
9,685.17±793.86a |
21,984.39±2,474.56a |
16,572.54±2,463.92a |
| Ribavirin |
5,082.85±588.02b |
11,670.44±1,203.63a,c |
11,949.95±2,778.89a |
| Low-dose SFI |
6,369.82±437.53a |
13,275.05±2,736.71a,d |
7,782.85±438.33a,c,e |
| High-dose SFI |
4,793.96±629.65b |
5,782.85±692.68a,c,f |
5,329.74±502.10a,c,f |
 | Table III.Effects of Shenqi Fuzheng injection
(SFI) on expression levels of FasL protein in a mouse model of
viral myocarditis. |
Table III.
Effects of Shenqi Fuzheng injection
(SFI) on expression levels of FasL protein in a mouse model of
viral myocarditis.
| Group | Day 3 | Day 10 | Day 30 |
|---|
| Blank control |
2,775.22±815.23 |
3,622.22±723.71 |
3,091.64±906.83 |
| Model |
10,121.14±1,142.29a |
18,643.45±1,261.34a |
14,001.09±1,273.42a |
| Ribavirin |
7,114.32±603.02b |
13,210.27±815.73a,c |
12,023.18±660.12a |
| Low-dose SFI |
8,131.18±722.24b |
14,802.36±964.35a,c,d |
9,433.29±551.72a,c,e |
| High-dose SFI |
7,921.25±512.43b |
10,536.04±1,480.64a,c,e |
8,419.39±507.09a,c,f |
Discussion
SFI contains two Chinese medicinal herbs: Radix
Astragali, which is commonly used as an immunomodulating agent in
the treatment of immunodeficiency diseases and to alleviate the
adverse effects of chemotherapeutic drugs, and Radix Codonopsis,
which is typically used to treat dyspepsia, fatigue, bronchitis,
cough, inflammation (23).
Myocarditis is considered to belong to the VMC
category of traditional Chinese medicine (TCM) (19). VMC is most common among individuals
with deficiencies of both energy and Yin Qi who are vulnerable to
‘fire due to yin-deficiency’ (FFYD), also known as ‘Re Shang Qi’ or
‘Re Shang Yi Yin’; therefore, these are contributing factors for
the development of VMC (17). A
study conducted by Cao and Yin (24)
demonstrated that combined energy and Yin Qi deficiency is the main
mechanism of VMC pathogenesis, which affects the whole disease
progress; therefore, insufficiency of heart-qi and yang (IHQY)
therapy is the predominant basic treatment option for VMC. Since Qi
(vital energy) can be generated in body fluid, it may be the basis
and driving force for the production and transportation of fluid.
Furthermore, Qi may implement fluid functions and, therefore,
variability in the activity of Qi may stimulate the excretion or
re-production of fluid (25). Since
Qi helps to transport fluid between cells, it regulates the
excretion of fluid and nourishes the lungs, thus preventing the
over-excretion of fluids. The TCM, Qi and fluids maintain the
balance of water metabolism, thus making SFI the preferred
treatment option (25). As a TCM,
Chen Qi infusion is a formulation that predominantly consists of
Codonopsis pilosula and Astragalus. C.
pilosula contains polysaccharides, multiple amino acids and
various other inorganic elements; whereas the Astragalus
genus contains saponins, polysaccharides, flavonoids, flavonoid
analogs and multiple amino acids (24). In TCM, Radix Codonopsis and Astragali
are compatible, with beneficial effects on the spleen and kidney,
protecting and strengthening the functions of the body. Current
understanding of the pathogenesis of VMC remains poor; however,
animal and in vivo experiments, established using coxsackie
B group viruses, have indicated that damage following the infection
and the immune response generated are the main mechanisms of VMC
pathophysiology (26). The apoptotic
changes of cells during VMC have garnered considerable attention
worldwide in recent years. The Fas/FasL system is of particular
interest, as it is a direct initiator of the signaling pathway
during apoptosis and has an important role in the apoptosis of
cardiac muscle cells (27).
The results of the present study demonstrated that
the AI and expression levels of Fas and FasL proteins were
increased in the model group, as compared with the blank control
group, indicating that apoptosis induced by the Fas/FasL system is
involved in the development and progression of VMC. In the acute
phase, AI and Fas/FasL protein expression levels were reduced in
the high-dose SFI group, as compared with the other groups,
suggesting that SFI may inhibit the expression of Fas/FasL proteins
in a dose-dependent manner, thus inhibiting apoptosis. During the
chronic phase, the low-dose SFI group demonstrated decreased AI and
decreased expression levels of Fas/FasL proteins compared with the
model group; however, a dose-dependent trend was not detected.
Considering that the protective roles of SFI to ‘Zheng Qi’ (the
ability of the body to resist disease) are involved, potentially
meaning appropriate dose is sufficient to protect Zheng Qi. It has
previously been demonstrated that A. membranaceus plus
supportive therapy is effective at improving myocardial enzymes,
abnormal electrocardiogram and cardiac function, and SFI is
effective at improving the immune system of mice (23,28).
There are currently three basic therapeutic approaches for the
treatment of VMC using TCM, including excretory function
enhancement, cardiovascular system improvement and tonic effect
reinforcement.
The present study had certain limitations and
further robust trials are required in order to explore the use of
herbal medicines in the treatment of VMC. In particular, the
specific immunological and cytotoxic mechanisms require
investigation, and the main effective components of the formulation
should be identified. Furthermore, any potential interactions
between the components require investigation.
In conclusion, apoptosis induced by the Fas/FasL
system is associated with the pathogenesis of VMC, and may be
pivotal. SFI inhibited the apoptosis of cardiac cells and may have
a therapeutic role in the treatment of VMC by downregulating the
expression of Fas/FasL proteins. Therefore, the results of the
present study suggested that SFI may be used to treat VMC; however,
the mechanisms underlying the Fas/FasL-downregulating effects of
SFI and the subsequent apoptosis of cardiac cells require further
elucidation.
Acknowledgements
The authors would like to thanks the Professor Fund
at The Education Department of Fujian Province (grant no. JS07013)
for support.
References
|
1
|
Kang PM and Izumo S: Apoptosis in heart:
Basic mechanisms and implications in cardiovascular diseases.
Trends Mol Med. 9:177–182. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Gottlieb RA, Burleson KO, Kloner RA,
Babior BM and Engler RL: Reperfusion injury induces apoptosis in
rabbit cardiomyocytes. J Clin Invest. 94:1621–1628. 1994.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Olivetti G, Abbi R, Quaini F, Kajstura J,
Cheng W, Nitahara JA, Quaini E, Di Loreto C, Beltrami CA, Krajewski
S, et al: Apoptosis in the failing human heart. N Engl J Med.
336:1131–1141. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kearney MT, Cotton JM, Richardson PJ and
Shah AM: Viral myocarditis and dilated cardiomyopathy: Mechanisms,
manifestations, and management. Postgrad Med J. 77:4–10. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Cooper LT Jr: Myocarditis. N Engl J Med.
360:1526–1538. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Suda T, Takahashi T, Golstein P and Nagata
S: Molecular cloning and expression of the Fas ligand, a novel
member of the tumor necrosis factor family. Cell. 75:1169–1178.
1993. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ashkenazi A and Dixit VM: Death receptors:
Signalling and modulation. Science. 281:1305–1308. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Krammer PH: The CD95 (APO-1/Fas) CD95L
system. Toxicol. Lett. 103:131–137. 1998.
|
|
9
|
Cheng W, Li B, Kajstura J, et al:
Stretch-induced programmed myocyte cell death. J Clin Invest.
96:2247–2259. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kajstura J, Cheng W, Reiss K, Clark WA,
Sonnenblick EH, Krajewski S, Reed JC, Olivetti G and Anversa P:
Apoptotic and necrotic myocyte cell deaths are independent
contributing variables of infarct size in rats. Lab Invest.
74:86–107. 1996.PubMed/NCBI
|
|
11
|
Yaniv G, Shilkrut M, Lotan R, Berke G,
Larisch S and Binah O: Hypoxia predisposes neonatal rat ventricular
myocytes to apoptosis induced by activation of the Fas (CD95/Apo-1)
receptor: Fas activation and apoptosis in hypoxic myocytes.
Cardiovasc Res. 54:611–623. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Monroe EW: Desloratidine for the treatment
of chronic urticaria. Skin Therapy Lett. 7:1–5. 2002.PubMed/NCBI
|
|
13
|
Lu Y and Lu YX: Clinical application and
pharmacology function of Shenqi fuzheng injection. Shizhen Guo Yi
Guo Yao. 17:2083. 2006.(In Chinese).
|
|
14
|
Pan L: The practice of digital traditional
Chinese medicine of Shenqi Fuzheng injection. Zhongguo Chu Fang
Yao. 1:37–39. 2009.(In Chinese).
|
|
15
|
Zhong ZH: Oral history: The
industrialization of Shenqi Fuzheng injection - from proved recipe
to SFDA approved new drug. Zhongguo Chu Fang Yao. 1:33–36. 2009.(In
Chinese).
|
|
16
|
Li Y, Mai GR, Chen BF and Li T: The
relationship between the apoptosis mediated by Fas/Fasl ligand
system and virus myocarditis in mice. Shi Yong Er Ke Lin Chuang Za
Zhi. 17:631–632. 2002.(In Chinese).
|
|
17
|
Wang SH, Wang Q and Liu BC: Experience on
the treatment of viral myocarditis through the lungs. Xin Zhong Yi.
39:15–16. 2007.
|
|
18
|
Luo H, Han M and Liu JP: Systematic review
and meta-analysis of randomized controlled trials of Chinese herbal
medicine in the treatment of Sjogren's syndrome. Zhong Xi Yi Jie He
Xue Bao. 9:257–274. 2011.(In Chinese). View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Jiao HJ: The pharmacology efficacy and
clinical application about dangshen. Chinese Journal of Clinical
Medicine. 25:89–92. 2005.
|
|
20
|
Shao BM, Xu W, Dai H, Tu P, Li Z and Gao
XM: A study on the immune receptors for polysaccharides from the
roots of astragalus membranaceus, a Chinese medicinal herb. Biochem
Biophys Res Commun. 320:1103–1111. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Zhang MX and Cao HQ: Effects of Yi qi
compound on cardiac muscle cells of CVB3 viral myocarditis. Zhong
Guo Zhong Yi Yao Xin Xi Za Zhi She. 8:35–38. 2011.(In Chinese).
|
|
22
|
Bi MR: The association between Fas
expression and the prognosis of myocarditis. Shandong Da Xue Xue
Bao. 4:60–61. 2006.(In Chinese).
|
|
23
|
Xu CR and Zhou JH: Astragalus injection in
the treatment of acute viral myocarditis. Yi Xue Li Lun Yu Shi
Jian. 22:655–656. 2009.(In Chinese).
|
|
24
|
Cao HH and Yin HJ: Clinical practice of Yi
qi yang yin therapy on viral myocarditis. Zhong Yi Jiao Yu.
18:52–53. 1999.
|
|
25
|
Sun GY, Tong Y, Chen KW and Li QZ: Basic
theory of TCM. Beijing: Zhongguo Zhong Yi Yao Za Zhi. 8:150–153.
2002.
|
|
26
|
Zhang JH and Zhang YL: Shenqifuzheng
infusion treats viral myocarditis - observational study of 32
patients. Zhongguo Meitan Gongye Yixue Zazhi. 4:5802010.(In
Chinese).
|
|
27
|
Mei H, Ren SM and Bo L: Role of Fas/Fas
ligand apoptotic pathway of peripheral blood lymphocytes in the
development of viral myocarditis. Zhongguo Xiao Er Ji Jiu Yi Xue.
4:320–322. 2011.(In Chinese).
|
|
28
|
Niu RY, Yan XY and Wang JD: Effects of
Shenqi Fuzheng injection on the immune function in mice. Shanxi
Nong Ye Ke Xue. 36:86–88. 2008.(In Chinese).
|